Relationship between negative emotions and perceived support among parents of hospitalized,critically ill children
Brad E.Phillips,Laurie A.Theeke,Katie M.Sarosi
West Virginia University School of Nursing,Morgantown,WV,United States
Keywords:Child Critical illness Emotional support Negative emotions Parents Psychological state
ABSTRACT Objectives:The purpose of this study was to describe relationships between negative emotions and perceived emotional support in parents of children admitted to the pediatric intensive care unit (PICU).Methods:This cross-sectional descriptive study conducted face-to-face interviews between January 2019 and January 2020.Study variables included depression (PHQ-9 Scale),anxiety (Emotional Distress-Anxiety-Short Form 8a),anger (Emotional Distress-Anger-Short Form 5a),fear (Fear-Affect Computerized Adaptive Test),somatic fear (Fear-Somatic Arousal-Fixed Form),loneliness (Revised 20-item UCLA Loneliness Scale),and perceived emotional support (Emotional Support-Fixed Form).Results:Eighty parents reported symptoms of depression 8.00(4.00,13.75),anxiety(23.43±7.80),anger(13.40 ± 5.46),fear (72.81 ± 27.26),somatic fear 9.00(6.00,12.75),loneliness (39.35 ± 12.00),and low perceived emotional support (32.14 ± 8.06).Parents who were young,single,low-income,and with limited-post secondary education reported greater loneliness and lower perceived emotional support.Fear correlated with depression (r=0.737,P < 0.01) and anxiety (r=0.900,P < 0.01).Inverse relationships were discovered between perceived emotional support and loneliness(r=-0.767,P<0.01),anger(r=-0.401,P < 0.01),and depression (r=-0.334,P < 0.01).Conclusions:The cluster of negative emotions identified will serve as potential targets for future interventions designed to enhance support for parents of critically ill children.
What is known?
·The PICU is a high stress environment for parents of critically ill children.It is known that parents experience symptoms of depression,anxiety,and stress during admission and after discharge.
What is new?
·In addition to depression and anxiety,parents in the PICU experience anger,fear,loneliness,and low perceived emotional support.All symptoms are intercorrelated,creating a cluster of negative emotions.No differences were noted between gender and psychological status.However,those that are young,single,with low income and limited post-secondary education report greater loneliness and lower perceived emotional support.
1.Introduction
The pediatric intensive care unit (PICU) provides high-quality care to the most vulnerable and critically ill children in the region.The acuity of illness and high stress environment of the PICU presents a variety of challenges to those involved in the child’s care.With a recent push for family-centered care,parents are being empowered to actively participate in their child’s treatment plan[1].As nurses work to include parents in the care of their critically ill child,it will become increasingly important to truly understand the psychological and emotional responses of parents with children in the PICU.
Overall,there is a paucity of studies that have assessed psychological or emotional health of parents whose children are admitted to intensive care units.Studies that have measured emotions of stress,anxiety,and/or depression in parents of children in the PICU report that approximately 25% of parents experience moderate to severe anxiety and up to 50% report symptoms of depression during admission [2,3].There have also been studies that identify the presence of these emotions after discharge [4].Parents have also exhibited symptoms of both acute traumatic stress[2]and post-traumatic stress disorder[3,4]during admission and as far as 19 months post-discharge [5].
Qualitative studies described PICU parents as feeling traumatized during their experience,reporting helplessness,uncertainty,and fear concerning the outcome of their critically ill child [6].Some parents even described their experiences as“being in another world” [7].
It is critical that nurses understand the emotions of parents so that clinical interventions can be developed and tested to inform practice changes to meet identified needs.Several gaps exist when seeking to understand the range of emotions experienced by parents of critically ill children in the PICU.Though it is likely that parents experience a range of negative emotions when a child is admitted to the PICU,the current body of literature reflects a limited view of emotions that parents may experience.It is the premise of this work that parents may experience fear,anger,loneliness,and low perceived emotional support concurrently with psychological symptoms of anxiety and depression.Furthermore,gender and other socio-demographic differences may exist and have been under-explored in parents of critically ill children.In addition,there have been limited studies that assessed the conduciveness of the PICU environment for recruiting and enrolling parents in nursing research projects.Therefore,the purpose of this study was twofold:to describe the emotional responses of parents of acute critically ill children and,to assess the feasibility of conducting nursing research with parents in the PICU environment.
McCubbin and Patterson’s (1982) Theory of Family Stress and Adaptation served as the guiding theoretical framework for the study.The theory describes how families respond to a stressor in a crisis situation based on their perception of the stressor and the availability of resources.This theory has demonstrated previous success in its use with families in the PICU environment [8].
The study purpose was met with the following two aims:1)identify and describe relationships among gender,sociodemographics,depression,anxiety,anger,fear,loneliness,and perceived emotional support in parents of acute critically ill children,and 2) evaluate the feasibility of the proposed project on recruitment,eligibility criteria for enrollment,and completion of responses on selected measures.Hypotheses for Aim 1 included:(a)parents will report one or more symptoms of the psychological study variables,(b) parents who report loneliness will be more likely to report symptoms of depression and/or anxiety,and (c)parents who report low perceived emotional support will be more likely to report symptoms of fear.
2.Materials and methods
2.1.Participants and sample size
This study employed a cross-sectional descriptive quantitative design.The sample size was calculated using a sample size calculator [9]to determine representativeness of an accessible population of 500 inpatient children (estimated number of critical admissions to the PICU in one year).Using the population size of 500 with a confidence level of 90% and margin of error of 10%,we initially calculated a needed sample of 60.We then used the same error probability and power in G-power [10]to determine the sample size needed to detect a moderate effect for differences by gender.It was found that the required sample was 72 (36 per gender).To allow for these comparisons we oversampled to a sample size of 80.
Eligibility for participation was established using dual criteria.Parents who wished to enroll had to be the biological parent or designated caregiver of the child,18 years old or greater,and able to independently answer survey questions in English.In addition,the parents had to have a child who met two or more of the following criteria:length of stay(LOS) greater than or equal to three days in the PICU,intubated,receiving one continuous vasopressor or inotrope,current placement of a central intravenous catheter,and/or admission for an acute illness,unexpected injury,or trauma.Parents with known mental illness,of children who were already designated as Do Not Resuscitate status,or of children who were admitted for a chronic problem or planned procedure were excluded.Benchmarks for Aim 2 related to recruitment included:(a)a sample of 80 parents will be enrolled in a 120-day period,and(b)an adequate sample size will be enrolled for the study based on eligibility criteria.
2.2.Instruments
Self-report data was collected on the following study variables:depression was assessed using the Patient Health Questionnaire-9(PHQ-9) [11],anxiety was assessed using the Emotional Distress/Anxiety (Short Form 8a) [12],anger was assessed using the Emotional Distress/Anger (Short Form 5a) [13],fear was assessed using the Fear-Affect Computerized Adaptive Test [14]and Fear-Somatic Arousal-Fixed Form [15],loneliness was assessed using the Revised 20-item UCLA Loneliness Scale [16],and perceived emotional support was assessed using Emotional Support-Fixed Form[17].
The PHQ-9 is openly available for non-commercial and research purposes [11].It includes nine items with available responses ranging from 0 (not at all) to 3 (nearly every day) and is to be answered based on a time frame of the previous two weeks.Scores can range from 0 to 27,with the total score representing severity of depression.A score of 10-14 is indicative of mild major depression,15-19 is moderate,and 20 or greater is severe.Cronbach’s α coefficient range from 0.86 to 0.89 with sensitivity and specificity 74%and 91% respectively [18].
Emotional Distress/Anxiety (Short Form 8a) is openly available for non-commercial and research purposes [12].It includes eight items with available responses ranging from 1(never)to 5(always)and is to be answered based on a time frame of the previous seven days.Scores can range from 8 to 40 with higher numbers indicative of greater anxiety symptoms.Cronbach’s α coefficient is 0.93,with a correlation of 0.96 between the short form and the full-item bank[19].
Emotional Distress/Anger(Short Form 5a)is openly available for non-commercial and research purposes [13].It includes five items with available responses ranging from 1(never)to 5(always)and is to be answered based on a time frame of the previous seven days.Scores can range from 5 to 25 with higher numbers indicative of greater anger symptoms.Cronbach’s α coefficient is 0.90,with a correlation of 0.96 between the short form and full-item bank[19].
The Fear-Affect Computerized Adaptive Test is openly available for non-commercial and research purposes [14].It includes 29 items with available responses ranging from 1(never)to 5(always)and is to be answered based on a time frame of the previous seven days.Scores can range from 29 to 145 with higher numbers indicative of greater fear symptoms.Cronbach’s α coefficient is 0.98,with a total-item correlation of 0.70 [20].
The Fear-Somatic Arousal-Fixed Form is openly available for non-commercial and research purposes [15].It includes six items with available responses ranging from 1(never)to 5(always)and is to be answered based on a time frame of the previous seven days.Scores can range from 6 to 30 with higher numbers indicative of greater somatic symptoms.Cronbach’s α coefficient is 0.85 [21].
The Revised 20-item UCLA Loneliness Scale is openly available for non-commercial and research purposes [16].It includes 20 items with available responses ranging from 1(never)to 4(often).Scores can range from 20 to 80 with higher numbers indicative of greater perception of loneliness.Cronbach’s α coefficient is 0.94,with a correlation of 0.91 between the revised and original measures [22].
The Emotional Support-Fixed Form is openly available for noncommercial and research purposes [17].It includes eight items with available responses ranging from 1(never)to 5(always)and is to be answered based on a time frame of the previous seven days.Scores can range from 8 to 40 with higher numbers indicative of greater perceived emotional support.Cronbach’s α coefficient is 0.97 [21].
The raw scores of five instruments (anxiety,anger,fear-affect,fear-somatic,and emotional support) can be converted to Tscores to compare response means to the general population.The average T-score of the general population is 50 with a SD of 10.Tscore conversion tables are available within the scoring guide for each instrument.
For Aim 2,parents who participated completed a study evaluation that was designed by the research team.The evaluation included 10 items with available responses ranging from 1(strongly disagree)to 5 (strongly agree.)
2.3.Procedure of data collection
Flyers were placed in the PICU waiting room and throughout the Children’s Hospital to recruit participants.The study team rounded in the PICU once a week to identify potential participants.Additionally,the team presented the plan for the study to the staff nurses in the unit at a regular staff meeting to enhance staff engagement in accomplishing the study.Once deemed eligible,all participants completed informed consent with a HIPAA waiver prior to being interviewed for data collection.Interviews were completed face-to-face,took approximately 25-30 min,and participants received a$10.00 gift card.Benchmarks for Aim 2 related to data collection included:(c)enrolled participants will not report study burden or the perception of being overwhelmed during the data collection process,and (d) the research site will demonstrate an environment that is conducive to the successful implementation of nursing research.
2.4.Data analysis
All quantitative data were cleaned and explored prior to analysis.Data were analyzed using SPSS Version 26 [23].Sociodemographics were analyzed using descriptive statistics and reported in means,medians,standard deviations (SD),interquartile range,frequencies and percentages.Differences between gender,socio-demographics,and key study variables were analyzed using independent T-tests,Chi square comparisons,ANOVA,and nonparametric testing as appropriate based on variable type.For continuous psychological variables where differences were discovered based on categorical socio-demographic variables,appropriate post hoc testing was conducted for pairwise comparisons.Relationships between key study variables were analyzed using Pearson correlations.Feasibility was analyzed using process evaluations to assess for discrepancies between expected and observed recruitment and enrollment results compared to the planned study timeline.Field notes were used to determine the length of the interview and track enrollment compared to potential participants who decline to participate after being made aware of the study.All participants completed an evaluation to identify any burdens in the interview process and to assess the usefulness,clarity,and organization of the overall study.
2.5.Ethical considerations
Prior to conducting the study,a letter of approval was obtained from the West Virginia University Institutional Review Board(Protocol #1805113279).All participants received a copy of their informed consent that contained contact information for the research team and institutional research compliance office.A list of psychological supportive resources was available to each participant upon their request.All data was stored in a secured location and data that was identifiable was stored separate from other survey data.All participants completed an informed consent with HIPAA waiver prior to participating in the study.
3.Results
3.1.Results for overall sample
Eighty parents of 63 children were enrolled in the study.Ninety percent (72/80) of the parents were from West Virginia and the remainder were from surrounding states including Maryland,Pennsylvania,and Ohio.The sample was representative of the region but non diverse,including 78 parents who were white,with one Black and one Asian.The sample was comprised of 60 women and 20 men.Age of parents ranged from 19 to 63(33.29±9.62).All parents reported having another child living in the home.Child age ranged from less than one month old to 18 years.Child diagnoses included congenital heart defects,respiratory failure,sepsis,trauma/injury,neurological disorders,oncological complications,and surgical related diagnoses.Twenty-seven children were intubated and receiving mechanical ventilation,and 49 children had a central intravenous line.Average LOS in the PICU at the time of interview was 8.6 days.
Hypothesis 1a.was supported.Parents self-reported moderate to high scores for depression 8.00(4.00,13.75),anxiety(23.43±7.80),anger (13.40 ± 5.46),fear (72.81 ± 27.26),somatic fear 9.00(6.00,12.75),loneliness (39.35 ± 12.00),and low perceived emotional support (32.14 ± 8.06).
3.2.Demographic characteristics and psychological variables
Table 1 reports differences in psychological variables by respondent’s demographic characteristics.Men and women did not differ significantly when comparing psychological variables.Pairwise comparisons were conducted by demographic subgroups for psychological variables when there were significant differences in means.
Those that were ≤25 year’s old reported significantly higher loneliness scores than those in the 26-35 (P=0.022),36-45(P=0.020),or ≥46 (P=0.002) subgroups.In relation to marital status,those that were married or partnered reported significantly lower loneliness scores than those separated/divorced/widowed(P=0.009) or never married (P=0.020),and higher perceived emotional support than those who were never married(P=0.007).Although there was a significant difference between anger and marital status (P=0.042),there was no significance in pairwise comparisons between subgroups.Those that had obtained a college degree reported significantly lower loneliness scores and higher emotional support scores than those who had never completed their college degree(P=0.029/0.020)or had achieved a high school diploma or less (P=0.012/0.041).There was also significantly higher loneliness (P=0.001) and lower emotional support scores(P=0.018) for those that earned a yearly income less $40,000 compared to greater than $40,000.Finally,there was a significant difference in loneliness (P=0.029),somatic fear (P=0.039),and emotional support (P=0.024) and self-rated health with higher loneliness and somatic fear,and lower emotional support scores for those that rated their health poorly.

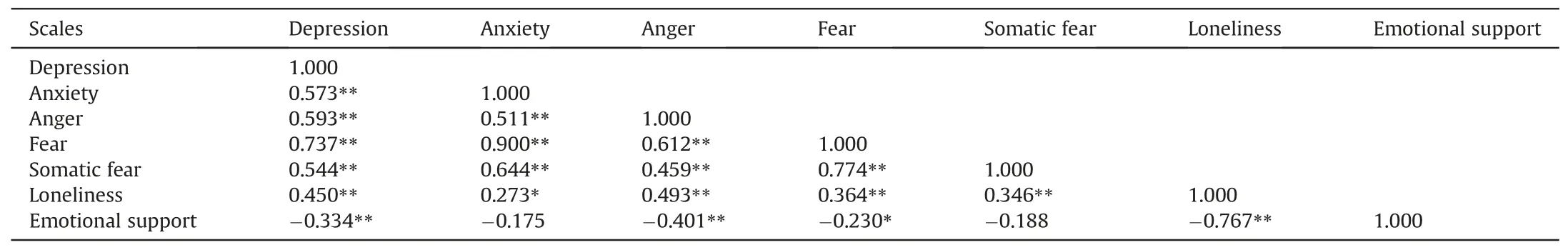
Table 2 Correlations of psychological variable(r).
3.3.Relationships between psychological variables
Table 2 reports on correlations between psychological variables.Hypothesis 1b was supported as loneliness positively correlated with depression(r=0.450,P<0.01)and anxiety(r=-0.273,P<0.05).Hypothesis 1c was partially supported as perceived emotional support was significantly inversely correlated with fear (r=-0.230,P < 0.05),but not somatic fear.In addition,higher levels of perceived emotional support were significantly inversely correlated with depression (r=-0.334,P < 0.01),anger (r=-0.401,P < 0.01),and loneliness (r=-0.767,P < 0.01).
3.4.Feasibility and acceptability outcomes
Benchmark 2a was not met as the timeframe for recruitment was 12 months which was longer than the expected 120 days.It was discovered that parents had interest in participating but would not proactively contact the research team based on flyers.The recruitment plan was altered to include rounding once a week,at minimum,in the PICU to recruit participants.This took additional time and extended the timeline of the study but allowed for successful recruitment.Benchmarks 2b and 2c were achieved as an adequate sample size was recruited for the study based on eligibility criteria.The majority (65/80) of study participants did not perceive feeling burdened by participating.Seventy-six participants were satisfied with the study method of recruitment,79 participants reported that they received a clear explanation of the study,78 participants reported that the research team was sensitive to parent time commitments,73 parents reported that they were able to remain focused during data collection,and all participants reported that the questions were easy to understand.Parents expressed a desire for continued interaction with the study team after the interviews were complete and over half of the participants provided contact information for future study involvement.Benchmark 2d was achieved with 73 parents reporting that the interview environment was quiet and private.Seventy-seven parents agreed that their privacy was protected,and 76 parents felt supported during the research process.Seventy parents reported believing that through participating,they would be helping others.The study team regularly reported that parents viewed completion of the study surveys as somewhat therapeutic and validating of their current emotions.The study team identified the importance of being flexible when interviewing parents as many parents requested to complete the interview process in their child’s hospital room,experienced brief interruptions and distractions from monitors and members of the healthcare team,yet still successfully completed all surveys.
4.Discussion
The findings from this study begin to shed light on the cluster of negative emotions that parents experience while having a critically ill child in the PICU.Knowing that parents of both genders experience anger,fear,loneliness and symptoms of anxiety and depression is important as nurses work with these parents.This storm of emotions is linked to stress responses and is associated with altered memory,low-attentiveness,and ineffective verbal fluency[24].This means that nurses may anticipate needing to give information frequently,repeat information,and assess parental knowledge of the critical situation as it evolves.Nurses may need to validate the parental emotional experience as a way of helping parents to deescalate overwhelming emotions.
The discovered relationships among emotional support and anxiety are relevant to family-centered-care.It is known that parents require extensive training when children with complex medical conditions are to be discharged home.Training programs that enhance knowledge of care can diminish parental stress and LOS[25].Based on study findings,it is likely that parents are experiencing symptoms of anxiety in tandem with unmet needs for emotional and social support.It has been found that increased social support can decrease levels of anxiety findings as far as 24 months post-discharge [26].This suggests that nurses should continue to incorporate parents in their child’s care,provide continuous education regarding each aspect of care,and allow early opportunities for parents to complete medical tasks that may have to be performed at home.
The findings from this study that associate depressive symptoms with less perceived support are congruent with the literature[3]and warrant further attention.It is likely that parents of critically ill children are worrying extensively about the health of their child.It is known that loneliness is a major predictor of depression in adults,and is related to ruminating thoughts,something that is likely when a parent is worried about the health state of their child[27].Parental support interventions that aim to assess and diminish loneliness in this parent population have the potential to prevent the development of depressive symptoms.
It is possible that enhanced emotional support delivered in wellplanned interventions would also allay fears,and potentially diminish loneliness and anger through enhanced human connection.Prior interventions studies of adults with fear[28],loneliness[29],and anger [30]suggest that practices that offer therapeutic support such as increasing social contact and techniques for relaxation have been successful in reducing symptoms of negative emotions.
Since both men and women reported significant symptoms and negative emotions,it will be important to further explore how these emotions are expressed in gender specific ways.These findings are congruent with reports from recent literature which described that mothers and fathers reported no significant differences in negative psychological outcomes [2,3].It is important for nurses to acknowledge implicit bias to avoid stereotyping or stigmatizing based on gender.For example,male stigma includes assumptions that men may have inadequacies related to childcare ability and be more likely to have violent behavior [31].Nurses should be cognizant of their biases regarding both male and female stigmas to reduce any disparities in family-centered care.
It is apparent that there is significant link between sociodemographics and psychological symptoms in parents of critically ill children,particularly for those reporting increased loneliness and low perceived emotional support.It is important that nurses be cognizant on parental social determinants of health and the impact that it may have on psychological status.Particular attention should be given to young,single,low-income parents who have not pursued post-secondary education.Additional supportive inpatient resources such as social work or case management may need to be provided.
It was evident that parents have significant needs that warrant intervention.During this study,parents were very perceptive and eager to complete the study,but they did not proactively reach out to the research team.Perhaps this is because parents are so engulfed in the care of their child and experiencing the identified cluster of emotions.In this setting,having the nurses initiate conversations that reflect awareness of common emotions experienced by parents might open a door for expression.With many participants seeking involvement in future studies,it indicates that parents may seek opportunities for expression of thoughts and feelings about their PICU experience.
5.Limitations and future implications for practice and research
5.1.Limitations
The study design is based on a convenience sample of parents of children from a single PICU site,which limits the generalizability of the findings.Parental responses were recorded at various stages in their child’s disease progression,and responses may have varied if collected at a different point during admission.Further,the crosssectional data collection provided a one point in time assessment of the data collected and does not reflect changes in psychological variables or tracking changes over time.Parents independently self-reported survey data which has a potential for respondent bias and the sample was weighted in female participants which could limit the findings in male participants.
5.2.Future implications for practice and research
One major implication for nursing practice for families of children in the PICU is the appropriate recognition and validation of parental emotions.Knowing the status of parental emotions is a key to a more precise family-centered approach.This type of approach will need to include a network of professionals that is interdisciplinary and includes members from social work,psychology,faith ministries,and care management specialists.
A gap remains when seeking an intervention that targets the specific psychological or emotional responses of parents whose child is admitted to an intensive care unit.Future studies will need to include the development and testing of novel interventions that could enhance support and diminish negative emotions for parents of critically ill children.
6.Conclusion
The findings of this study provide foundational information for this unique population.Understanding the emotional states of parents who are caring for critically ill children is essential to knowing how to provide family-centered care.In addition,this study reveals that parents experience a cluster of negative emotions concurrently with symptoms of depression and anxiety,offering new insight for clinicians.The impact of this interrelated cluster of emotions may have longer term consequences for parents as it may impact parental ability to learn about and fully comprehend the complexity of their child’s healthcare needs,or be psychologically available to provide the potential long-term care that is often required for children who have been hospitalized in the PICU.
CRediT authorship contribution statement
Brad E.Phillips:Conceptualization,Methodology,Investigation,Data curation,Writing-original draft,Writing -review &editing.Laurie A.Theeke:Supervision,Conceptualization,Methodology,Data curation,Writing-original draft,Writing -review &editing.Katie M.Sarosi:Investigation,Data curation,Writing -reviewing &editing.
Funding
This work was supported by the West Virginia University School of Nursing Research Investment Fund.
Declaration of competing interest
The authors declare that there are no conflicts of interest.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2020.10.001.
 International Journal of Nursing Sciences2021年1期
International Journal of Nursing Sciences2021年1期
- International Journal of Nursing Sciences的其它文章
- Focuses and trends of the studies on pediatric palliative care:A bibliometric analysis from 2004 to 2018
- The effect of digital health technologies on managing symptoms across pediatric cancer continuum:A systematic review
- Effectiveness of animal-assisted therapy on pain in children:A systematic review and meta-analysis
- Effects of creative expression program on the event-related potential and task reaction time of elderly with mild cognitive impairment
- Struggling to live a new normal life among Chinese women after losing an only child:A qualitative study
- Implementation and evaluation of a pain management core competency education program for surgical nurses
