Implementation and evaluation of a pain management core competency education program for surgical nurses
Xuelin Liu ,Li Li ,* ,Lingxio Wng ,Keel Herr ,Qiuchn Chen
a Department of Nursing,Zhujiang Hospital,Southern Medical University,Guangzhou,China
b College of Nursing,The University of Iowa,Iowa City,IA,United States
Keywords:Education Nurses Pain management Surgery department
ABSTRACT Objective:To investigate the effect of a pain management core competency education program on surgical nurses’ pain knowledge and pain management nursing practice behaviors.Methods:An 8-h education program focused on pain management core competency was provided twice in two weeks including the multidimensional nature of pain,pain assessment,pharmacological and nonpharmacological management,and knowledge application was developed and implemented for surgical nurses by a multidisciplinary team.Multimodal teaching approaches such as didactic teaching and vignettes of cases for nurses to discuss were used.The Clinical Pain Knowledge Test(CPKT)was completed by 135 and 107 nurses from 17 surgical wards pre and post-program,respectively.Two hundred and three patients’ medical records were randomly sampled according to the number of operations in each ward one week before and in the fifth week after the intervention,respectively.Documentation of patients’ postoperative pain management nursing practice behaviors and pain intensity scores were collected.Results:After the intervention,the CPKT scores of nurses significantly increased from 45.6% ± 12.3% to 54.2%±10.2%(t=5.786,P<0.001).Nurses’postoperative pain management nursing practice improved,with proportion of pain assessment documentation increased from 59.6% (121/203) to 74.9% (152/203)(χ2=10.746,P=0.001),those using pain intensity assessment tools increased from 81.8% (99/121) to 95.4%(145/152)(χ2=13.079,P<0.001),and intramuscular injection of nonopioids decreased from 12.6%(13/103) to 2.7% (3/111) (χ2=7.598,P=0.006).Patients’ average worst pain score on the operation day significantly decreased (Z=-2.486,P=0.013),and scores from the first to the third postoperative day also decreased (Z=-2.172,P=0.030).Conclusions:Implementation of a pain management core competency education program for surgical nurses can increase their knowledge of core competencies of pain management,improve selected pain management practices,and decrease patients’ postoperative pain intensity.
What is known?
·Undertreated acute postoperative pain leads to several adverse effects and pain assessment is a key to effective pain management.
·Surgical nurses play an important role in postoperative pain management.However,there were obvious deficits in knowledge and competencies related to pain management in nurses in China.
·Little is known about the implementation of pain management core competency education for surgical nurses to improve the quality of postoperative pain care.
What is new?
·An educational intervention focused on pain management core competency that includes didactic content teaching and case vignette application activities can help nurses recognize and manage pain more effectively in surgery patients.
·Continued gaps in outcomes such as the low scores on knowledge still evident suggest more improvement is needed.
1.Introduction
Postoperative pain is acute pain that occurs immediately after surgery,including body pain and visceral pain,usually lasting 3-7 days[1].Over 80%of patients experience acute postoperative pain after surgery,and approximately 75% reported the severity as moderate,severe,or extreme [2].Millions of surgeries are performed in China annually.In a survey in Beijing,China,up to 96%of patients reported they experienced mild to severe pain after orthopaedic surgery [3].In another survey with 4370 patients in Guangdong province in China,those with moderate and severe pain on the first day and the second day after surgery were 33.6%and 16.3%,respectively [4].Undertreated acute postoperative pain leads to several adverse effects such as the increased risk of maintaining or transitioning to chronic pain,poor sleep,higher complication rates,and costly burdens [5-7].Thus improving postoperative pain management in China is important.
Patient factors including gender,age,etc.as well as surgical factors including surgical site,operation instruments,etc.could influence patient’s pain levels after surgery[8,9].Pain management skills and knowledge of health professionals are also a substantial component of general professional competencies that impact good pain care[10].Nurses are important members of multidisciplinary pain management teams,and surgical nurses are the primary caregivers for perioperative patients and play an important role in postoperative pain management [11].It is well established that accurate pain assessment is essential to effective postoperative pain relief.In order to effectively manage the pain of postoperative patients,surgical nurses need good knowledge and skills of pain assessment and management,and to implement pain assessments,provide analgesic and nonpharmacologic interventions,and monitor analgesic effects and adverse reactions [12].Although nurses have some educational opportunities for pain management,studies indicate there were obvious deficits in knowledge and competencies related to pain management in nurses in China[13-15].
Some studies have shown that it may be possible to assist nurses to deal with pain in surgery patients by implementing educational programs [16,17].There are gaps in the pain education curriculum and training program for nurses in China.Nurses have very limited pain education in school,very few have an elective course on pain.After graduation,pain-related training is mostly in the form of continuing education.Even though there are education programs for improving pain knowledge,learner’s practice skills have not been improved [16,18].This is an important reason for the lack of quality pain management for patients.Therefore,determining strategies to effectively improve clinical pain knowledge to promote the skills and practice of surgical nurses is imperative.
How to effectively carry out pain education programs for nurses and improve their skills of postoperative pain management is the current challenge,and pain competencies as a component of entryto-practice requirements are needed [19].Competency-based education (CBE) is a framework for designing and implementing education that focuses on the desired performance characteristics of health care professionals,by establishing observable and measurable performance metrics that learners must attain to be deemed competent [20].Unlike traditional education,the critical issue of CBE is that learners meet the specified level of performance in terms of a competency [20].After an interprofessional consensus summit,core competencies for pain management were established[21].The International Association for the Study of Pain(IASP) has endorsed the importance of interprofessional pain education and competencies through the development of an interprofessional pain curriculum,which aligns closely with the published competencies [22].These competencies can serve as a foundation for developing,defining,and revising pain curricula.Incorporation of the core competencies for pain management in nursing education is critical to ensure that nurses have the essential knowledge and skills to effectively manage pain and to serve as a foundation on which clinical practice skills can be honed[23].At present,there is no research on the conduct of pain education program for surgical nurses focused on the expert consensus developed pain core competencies.
The purpose of this study was to evaluate the effectiveness of a pain management core competency education program on pain knowledge and pain management nursing practice of surgical nurses.
2.Methods
2.1.Participants
The study was conducted in a university-affiliated Grade-III Level A(the highest level of hospitals in China)general hospital in Guangzhou,China,from October 2017 to January 2018.The participants included nurses working in 17 surgical wards and their inpatients undergoing scheduled surgery.Nurses’inclusion criteria were:registered nurses working for at least three months on the surgical ward and informed consents were obtained to participate in the study.Student nurses,advanced training nurses,and nurses on vacation or in further training outside the hospital during the time of the study were excluded.
Medical records inclusion criteria were:patients undergoing scheduled surgery during the study period in the above 17 surgical wards,an expected hospital stay of at least one day after surgery.Those patients who were not back in the surgical ward after their operation were excluded.The sample of medical records of patients undergoing scheduled surgery was obtained one week before and the fifth week after the didactic content teaching was selected.The total number of elective surgery patients who were hospitalized in the surgical ward before the intervention was 405 per week.According to the sample size calculated by sampling from the population,we use this formula n ≥[24],in which N represents a finite population,α represents the significance level,κ represents the normal distribution quantile.To get the most reliable sample size,P was set as 0.5.The confidence level is 1-α,α=0.05,κ=1.96,and n=405/{(0.05/1.96)2× [(405-1)/(0.5 × 0.5)]+1}=197.40 ≈197.Considering that the total number of patients undergoing elective surgery within a week after the intervention fluctuates by 3%,the sample was set as 203 cases.
2.2.Instruments
2.2.1.Clinical Pain Knowledge Test (CPKT)
Developed by Bernhofer and St.Marie in 2017 [25],the CPKT could be used to determine gaps in education and to evaluate knowledge changes after pain management education activities.It includes 23 items and four pain management core competency aspects:the multidimensional aspect of pain,pain assessment and measurement,management of pain,and knowledge application in clinical conditions.
The total score was calculated as a percentage of the total number of questions answered correctly.A determination was made that a passing score was 75%or greater correct.Permission to translate the CPKT into Chinese was obtained from the authors.The Chinese version of the CPKT was used in a sample of clinical nurses with split-half reliability of 0.74,and a Pearson correlation coefficient of 0.71 for repeated measures [26].
2.2.2.Checklist for pain management nursing documentations
Developed by the authors according to the hospital’s pain management nursing documentation sheet,the checklist for pain management nursing documentation includes surgical patients’demographic and operation information,time returning to the ward after surgery,time interval of the first postoperative pain assessment,use of pain intensity assessment tools,day and time of pain assessment,pain intensity scores,pharmacological and nonpharmacological interventions,etc.The time interval of the first postoperative pain assessment refers to the time between the patient’s returning to the ward after surgery and nurses’ first pain assessment for patients.
2.3.Intervention
Based on the interprofessional consensus of core competencies for pain management,IASP interprofessional pain curriculum outline,and the 2017 IASP Global Year Against Pain After Surgery documents that cover specific topics related to postsurgical pain,a pain management core competency education program was developed for surgical nurses tailored to our previous survey results of knowledge gaps [26].The curriculum included the multidimensional nature of pain,pain assessment,pharmacological and non-pharmacological management,and knowledge application.It was reviewed and delivered by a multidisciplinary pain management team including six experts from anesthesiology,oncology,orthopedics,and nursing with rich experience in pain management to ensure its relevance,adequacy,and appropriateness (Table 1).Each department was provided a book entitled Pain Management Nursing[27]for supplementary learning materials.To enhance the delivery of content and application of new knowledge,multimodal teaching approaches such as didactic teaching,interactive teaching,and vignettes of cases for nurses to discuss were used by a multidisciplinary team.Support and advice from the faculty and pain experts were available.Through online video learning and WeChat,a mobile phone text and voice messaging communication service,knowledge and information were shared,discussed,and disseminated.
To standardize the quality of education intervention,an 8-h didactic content teaching was provided twice in two weeks.Considering the infeasibility of engaging all nurses in the education program due to shift schedule and workload challenges,at least ten percent of nurses including the pain management nursing team member in each department were required to participate.The participants were required to attend two 4-h education sessions.One of them was designated to train the nurses in their department at their convenient time using the same course PowerPoint and materials in one week.
The participants were required to implement the pain management nursing protocol issued by the Department of Nursing with adaptation to the types of surgery.The protocol focused on general aspects of comprehensive pain assessment,principles of intervention based on pain intensity and documentation of assessment and intervention of pain on the ward,e.g.the patient was assessed for pain every 4 h on the operation day,at least twice a day from the 1st to the 3rd postoperative day,and at least once a day from the 4th to the 7th postoperative day.
2.4.Data collection
Before and after the didactic content teaching,the CPKT was distributed to surgical nurses and returned immediately after completion.The nurses were required to independently complete and submit the questionnaires including the CPKT and demographic survey immediately after the education sessions.
Medical records of patients undergoing elective surgery one week before and in the fifth week after the education were randomly sampled according to the number of operations in each ward.Patients’postoperative pain treatment and documented pain intensity scores,and nurses’ pain assessment and management practice behaviors were collected.
2.5.Ethical considerations
The study was approved by the ethical review board of the hospital (ZJYY-2018-HLB-001).Informed consents of the eligible nurses were obtained.To ensure confidentiality,all the data documents were kept in a secure place only accessible to the researchers.
2.6.Data analysis
The IBM SPSS18.0 software was used for statistical analysis of data.In the descriptive analysis,the enumeration data were described through frequency and percentage,and the measurement data were represented by M (P25,P75) or Mean ± SD.The statistical inference was conducted through two independentsample t-test,non-parametric Mann-Whitney U test,Chi-square test,and Fisher’s exact test.P < 0.05 was considered statistically significant.
3.Results
3.1.Nurses’ scores of clinical pain knowledge
Before the education program,135 surgical nurses completed the CPKT.Among them,107 completed the post-test.There was no significant difference in the demographic information of nurses before and after the education program(Table 2).The CPKT scores of the nurses increased significantly after intervention(45.6% ± 12.3% vs.54.2% ± 10.2%,t=5.786,P < 0.001).After the program,the scores for each of the four knowledge domains ofnurses’pain management core competence significantly improved(Table 3).
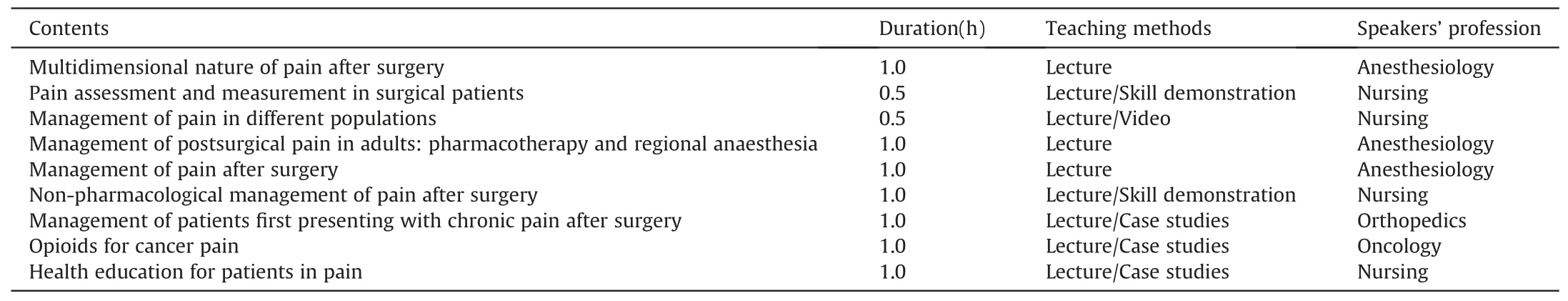
Table 1 Curriculum for pain management core competencies training for surgical nurses.
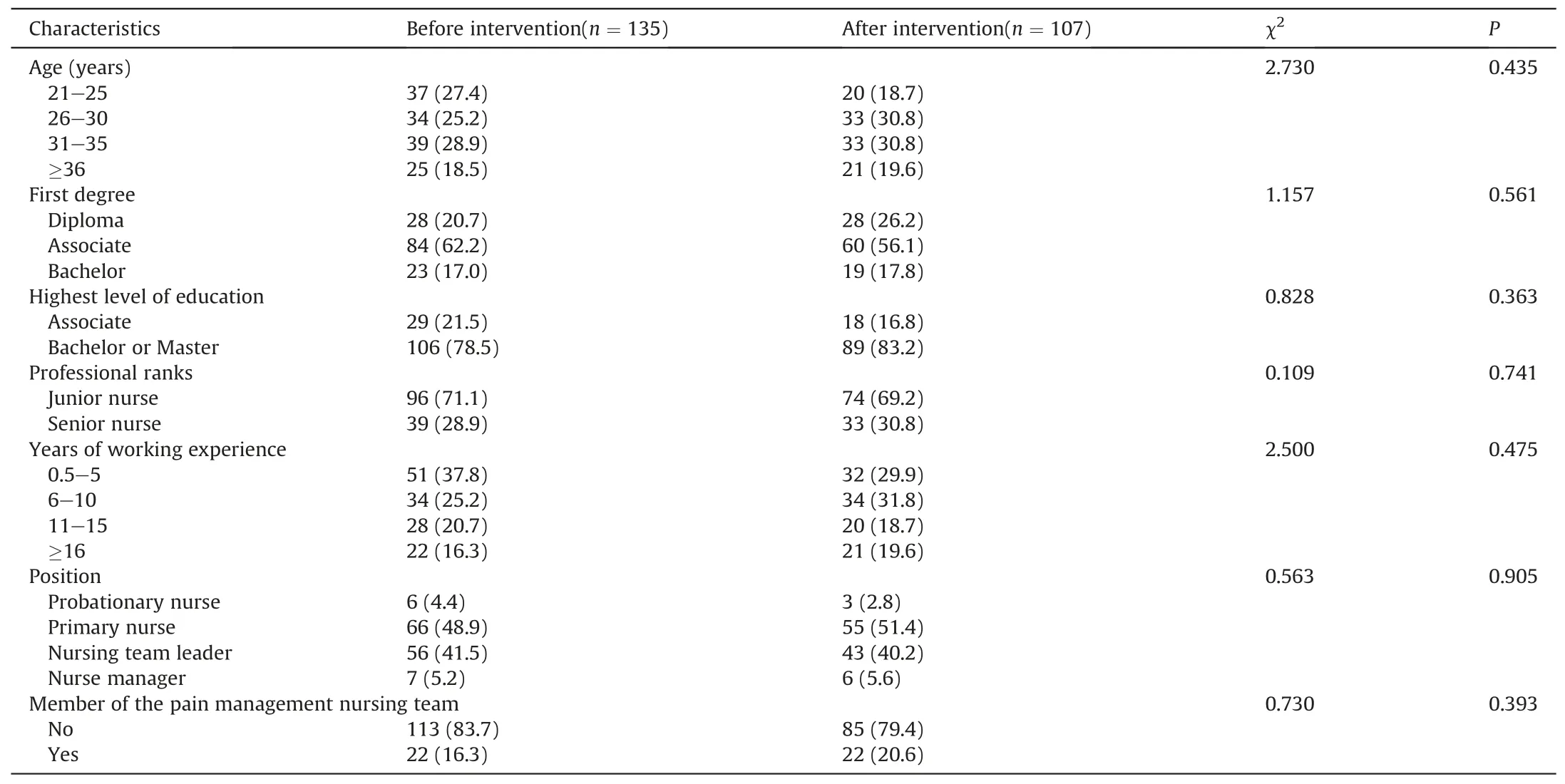
Table 2 Surgical nurses’ demographic information [n(%)].
3.2.Nurses’ pain assessment and management practice behaviors
Two hundred and three patients’medical records were audited before and after the intervention,respectively.
3.2.1.Pain assessment
Nurses’practice behaviors of postoperative pain assessment and management improved,with the proportion of pain assessment documentation increased from 59.6%(121/203)to 74.9%(152/203)(χ2=10.746,P=0.001).The time interval of the first postoperative pain assessment was substantially shortened (Z=-3.495,P < 0.001).The use of pain intensity assessment tools increased from 81.8%(99/121)to 95.4%(145/152)(χ2=13.079,P<0.001).The number of days with pain assessment documentation increased(Z=-3.307,P=0.001),pain assessment times increased(Z=-3.086,P=0.002),and pain assessment times during activity increased (Z=-2.282,P=0.022) (Table 4).
3.2.2.Pharmacological and non-pharmacological interventions
Before and after the program,there was no significant difference in the proportion of those with patient-controlled analgesia(41.9%vs.44.8%,χ2=0.251,P=0.617),and using analgesic types that includes nonopioids(50.7%vs.54.7%,χ2=0.632,P=0.426),opioids(25.6% vs.30.0%,χ2=0.993,P=0.319),and analgesic adjuvants(9.4%vs.8.4%,χ2=0.122,P=0.727)postoperatively.Proportion of intramuscular injection of nonopioids decreased from 12.6% (13/103) to 2.7% (3/111) (χ2=7.598,P=0.006).Among the nonopioid drugs used in this hospital,the intramuscular injection of drugs included parecoxib sodium for injection and rotundine sulfate injection.There was no significant difference in the proportion of nurses using non-pharmacological intervention measures(P > 0.05).
3.3.Postoperative documented pain scores of patients
Before and after the intervention,except for Body Mass Index(BMI),there was no significant difference in the demographic and clinical information between the two patient groups (P > 0.05)(Table 5).After the intervention,patients’ average worst postoperative pain score significantly decreased on the operation day(Z=-2.486,P=0.013),and from the 1st to the 3rd postoperative day also decreased (Z=-2.172,P=0.030) (Table 6).
4.Discussion
This study developed a pain management core competency education program based on the interprofessional consensus oncore competencies in pain education,pain curriculum outline of the IASP,and concerning the previous CPKT survey results by the authors [26].Moreover,the program was developed by a multidisciplinary pain management team,which was more systematic,comprehensive,and applicable.The use of case-based vignettes required application of knowledge obtained from the didactic teaching and may have contributed to pain assessment and management practices observed.

Table 3 Surgical nurses’ scores of CPKT pre-and post-intervention [ %,M(P25, P75)].
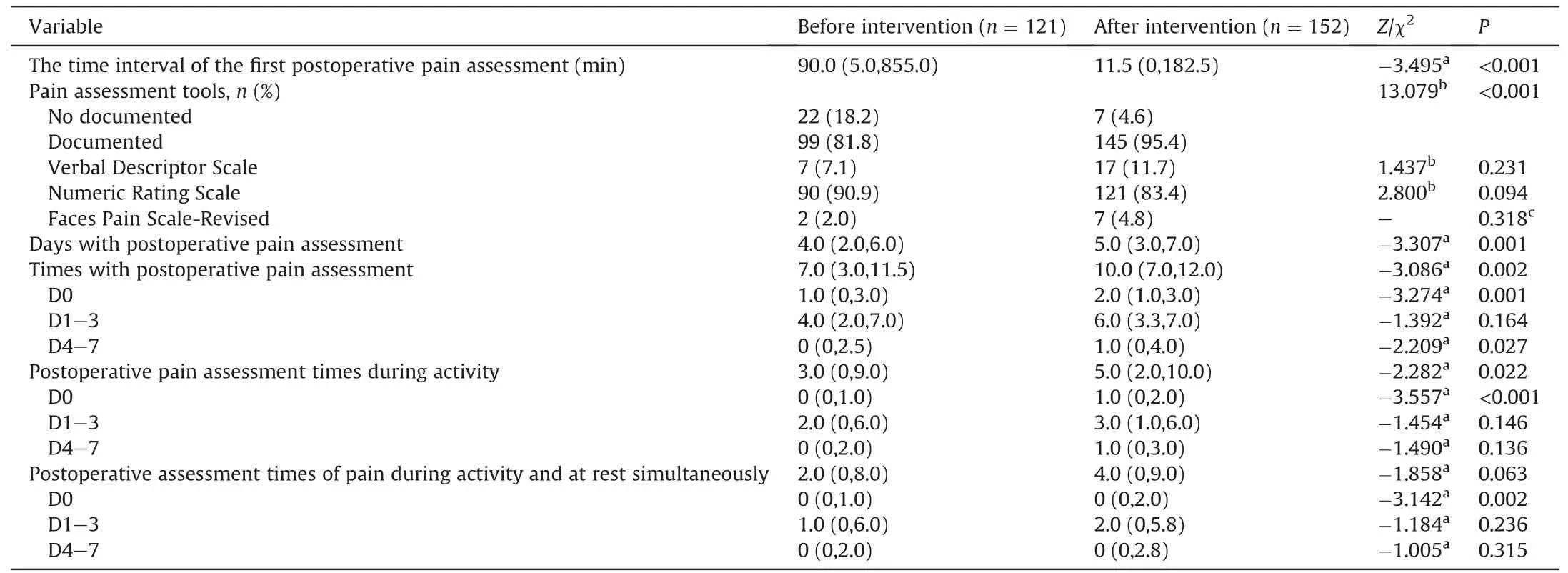
Table 4 Postoperative pain assessment documentation of patients pre-and post-intervention[M(P25,P75)].
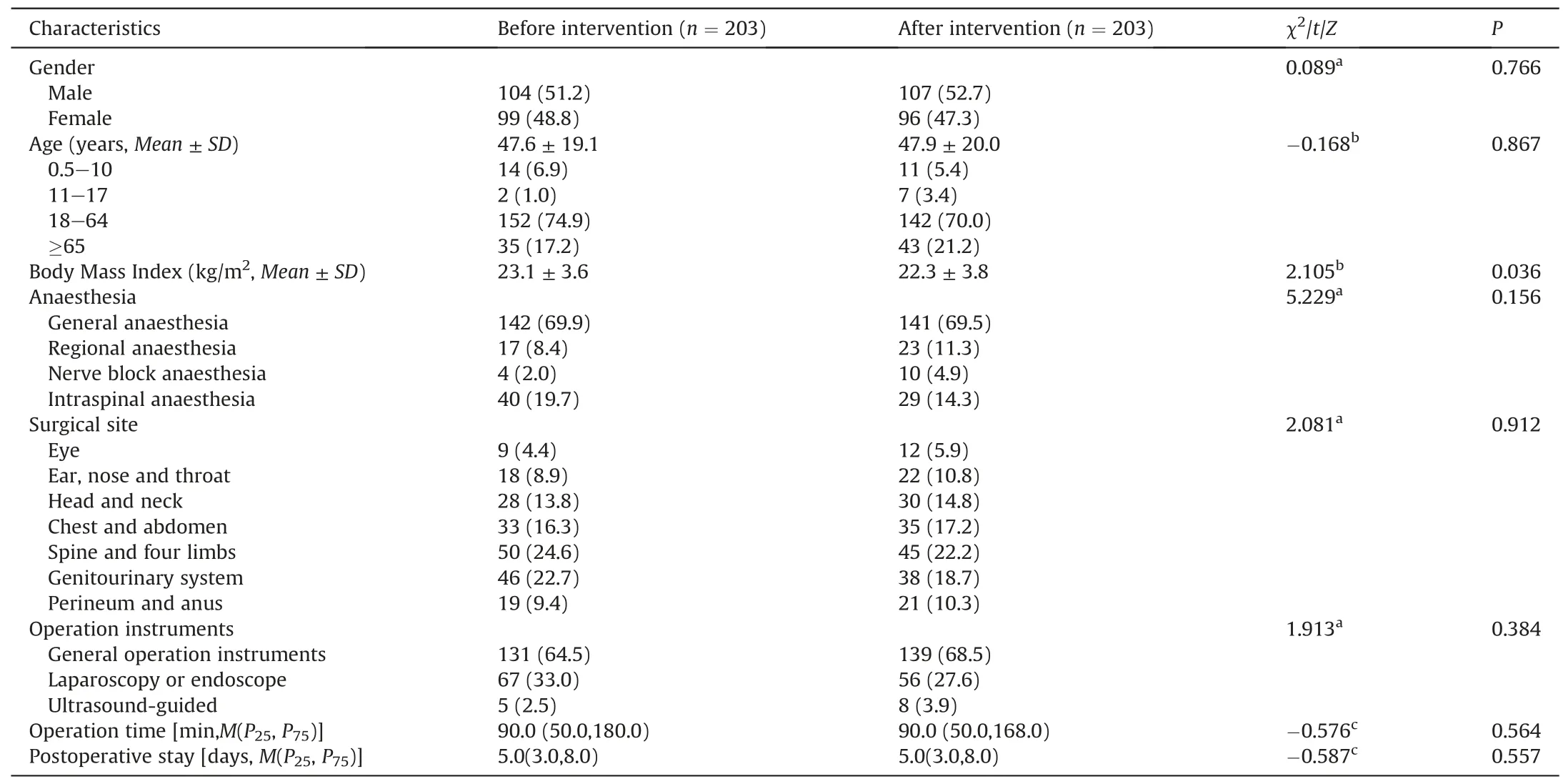
Table 5 Patients’ demographic and clinical information [n(%)].
However,the knowledge level of nurses regarding pain management was still too low,with the average percent correct of the CPKT was only 54.2% post-intervention,which failed to reach a commonly accepted passing level of 75%.The knowledge level of nurses regarding pain management was so low that improvements were needed.Before the education program,scores of the multidimensional aspect of pain,pain assessment and measurement,and management of pain were relatively low.This was consistent with our previous survey that clinical nurses’knowledge of the core competencies of pain management is inadequate,and pain education and clinical practice need to be strengthened to improve clinical nurses’ competencies of pain management [26].After education,scores of these three domains were still low and although improved,do not suggest strong knowledge of pain competencies.The application domain was better,which is good to see they could apply content to clinical situations.
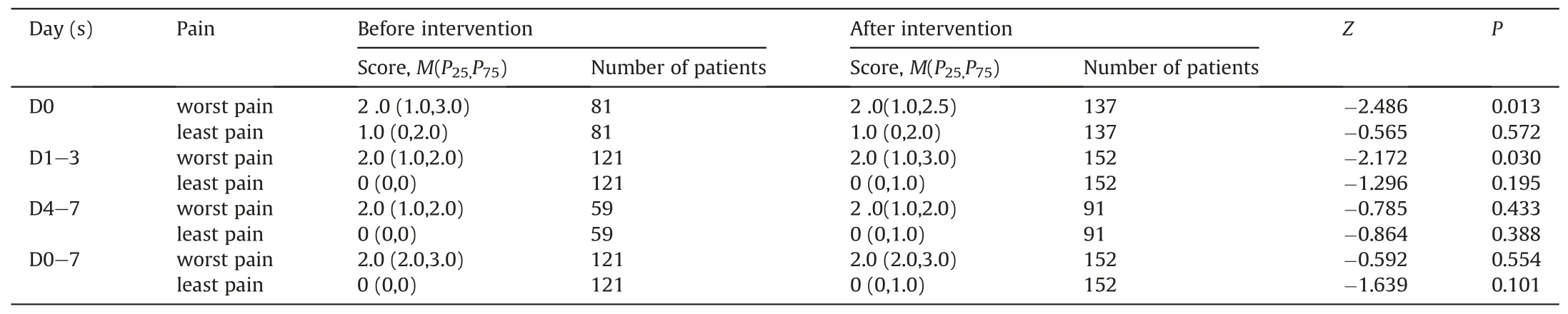
Table 6 Postoperative documented pain scores of patients pre-and post-intervention.
Score on the multidimensional aspect of pain,which mainly covered the neurobiological mechanisms of pain and basic theory of pain,was the lowest domain regardless of the intervention.The reason may be that few nurses had a formal course on pain during school and the pain content in this domain is complex with limited prior knowledge and not easy for the nurses in this study to comprehend.
Selected practice behaviors of nurses’ postoperative pain assessment and management also improved.The intervention taught nurses to be more active and standardized in postoperative pain management documentation.The proportion of nurses using pain assessment tools increased,and the time interval of the first postoperative pain assessment significantly shortened.Although the proportion of records with documentation of pain assessments significantly improved on the operation day and from the 4th to the 7th postoperative day,the average daily assessment times still does not meet best practices of assessing pain.
A significant increase in times of postoperative pain assessment during activity within 8 days after surgery,indicates that nurses paid more attention to pain assessment during activity.However,the number of pain assessment times significantly increased only on the operation day,there was no improvement from the 1st to the 7th postoperative day.The practice of nurses in this study assessing pain both during activity and at rest is insufficient.According to the guidelines for postoperative pain management [2,28,29],the intensity of pain at rest and during activity should be included in postoperative pain assessment.Strengthening postoperative pain management nursing practices during activity and using effective pain assessment methods are needed.It is important to promote the application of knowledge transformation and standardize postoperative pain care practices.
The patients’documented pain intensity significantly decreased within 3 days after surgery.However,there was no significant difference in the proportion of non-pharmacological interventions used by nurses before and after the intervention,which may be related to the relatively high use of non-pharmacological interventions initially.There was no significant difference in the types of analgesic drugs received by patients,but the proportion of patients receiving nonopioids by intramuscular injection decreased after the intervention.The route of administration of parecoxib sodium for injection could be intravenous or intramuscular injection.According to the recommendations from the Clinical Practice Guideline on the Management of Postoperative Pain endorsed by the American Pain Society,using the intramuscular route in the administration of analgesics for the management of postoperative pain should be avoided [2].It is possible that improved nurses’knowledge of pain management led to improved communication with the physician and a change in prescribing practices.Patients’average worst postoperative pain score on the operation day,and from the first to the third postoperative day decreased.Nurses’knowledge and skills about pain assessment and management may be a contributing factor to the changes in pain scores.
Important practice changes and improved patient outcomes were noted in this study.An educational intervention focused on pain management core competency that includes didactic content teaching and case vignette application activities can help nurses recognize and manage pain more effectively in surgery patients.To further improve the pain education effect,we should continue to strengthen weak areas of the nurses’ pain management core competency.
5.Limitations
There were potential limitations to this study.First,the pain intensity scores in this study were obtained from documentation in the medical and nursing records,the frequency of documentation may not accurately reflect the assessments nurses completed.More pain-related patient-reported outcomes are needed to better evaluate the impact of an intervention to improve knowledge and practice.Second,nurses’ pain management practices were examined for only one month after the intervention.The long-term effects of the intervention are unknown and establishing lasting effects is needed.Third,although patient outcomes are related to practices of every clinician,student nurses,advanced training nurses,and nurses on vacation or in further training outside the hospital were excluded.Further studies could examine the impact of this group and also physicians in impacting postoperative pain practices and outcomes.
6.Conclusions
Implementation of a pain management core competency training program for surgical nurses can increase their knowledge of core competencies of pain management,improve selected pain management practices,and decrease patients’ postoperative pain intensity.Continued gaps in outcomes,such as the low scores on knowledge still evident,suggest more improvement is needed.The feasibility of the education program,such as time invested,ability to engage the nurses,and barriers,etc.,deserves further investigation.
Funding
This education project is supported by the IASP Developing Countries Project:Initiative for Improving Pain Education.
CRediT authorship contribution statement
Xuelian Liu:Conceptualization,Methodology,Investigation,Formal analysis,Writing -original draft.Li Li:Conceptualization,Methodology,Supervision,Writing -review & editing.Lingxiao Wang:Methodology,Resources,Writing -review &editing.Keela Herr:Methodology,Supervision,Writing -review & editing.Qiuchan Chen:Investigation,Formal analysis.
Declaration of competing interest
The authors declared that they have no conflicts of interest to this work.
Acknowledgment
The authors thank Dr.Esther I.Bernhofer,from Case Western Reserve University,Frances Payne Bolton School of Nursing,Cleveland,Ohio,USA,and Dr.Barbara St.Marie,College of Nursing,from the University of Iowa,Iowa,USA,for their permission to use and translate the Clinical Pain Knowledge Test from English to Chinese.We would also like to thank Drs.Shiyuan Xu,Rui Xu,Lijun Lin,and Gang Wu,and Head Nurse Ms.Lijuan Hu,for their participation in the implementation of the program.The authors are grateful to Dr.Daguo Xu,Ms.Fang Yuan,Mr.Xibing Yang,and all the nursing staff from the surgical wards,for their kind assistance with data collection.To those patients who participated in the study,the authors extend special thanks.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2020.09.008.
 International Journal of Nursing Sciences2021年1期
International Journal of Nursing Sciences2021年1期
- International Journal of Nursing Sciences的其它文章
- Focuses and trends of the studies on pediatric palliative care:A bibliometric analysis from 2004 to 2018
- Relationship between negative emotions and perceived support among parents of hospitalized,critically ill children
- The effect of digital health technologies on managing symptoms across pediatric cancer continuum:A systematic review
- Effectiveness of animal-assisted therapy on pain in children:A systematic review and meta-analysis
- Effects of creative expression program on the event-related potential and task reaction time of elderly with mild cognitive impairment
- Struggling to live a new normal life among Chinese women after losing an only child:A qualitative study
