Sheathless and fluoroscopy-free retrograde intrarenal surgery: An attractive way of renal stone management in high-volume stone centers
Sarwar Noori Mahmood *, Hewa Toffeq , Saman Fakhralddin
a University of Sulaimani College of Medicine, Kurdistan, Iraq
b Sulaimania General Teaching Hospital, Sulaimania, Iraq
KEYWORDS Renal stone;Retrograde intrarenal surgery;Sheathless flexible ureterorenoscopy;Fluoroless retrograde intrarenal surgery
Abstract Objective: To evaluate the efficacy and safety of sheathless and fluoroscopy-free flexible ureterorenoscopic laser lithotripsy (FURSL) for treating renal stones.Methods: Between May 2015 and May 2017,135 patients with renal stones treated with sheathless and fluoroscopy-free FURSL were prospectively evaluated.Our technique involved a semirigid ureteroscopic assessment of the ureter,and the guidewire was left in situ to railroad the flexible ureteroscope. A holmium laser was used to fragment and dust the stones; fragments were neither grasped nor collected.Results: The study population consisted of 135 patients including 85 males(62.96%)and 50 females(37.04%)with a mean age of 40.65 years(range:3-70 years)were evaluated.The mean stone size was 17.23 mm (range: 8-41 mm). Complete stone-free status was achieved in 122(90.37%)patients and clinically insignificant residual fragments(CIRF)in two(1.48%),while residual stones were still present in 11(8.15%)patients.Postoperative complications occurred in 23 (17.4%) cases and were mostly minor, including fever in 17 (12.6%), pyelonephritis in four(3.0%), subcapsular hematoma in one (0.7%) and steinstrasse in one (0.7%). These complications were Clavien I-II, GI in 17 (12.6%) patients, GII in five (3.7%), and Clavien IIIb in one(0.7%). No major complications were observed. Stone size ≥2 cm, operative time ≥30 min,and lasing time ≥20 min were significantly associated with a higher rate of complications and lower stone-free rates upon univariate analysis (p<0.05).Conclusion: Sheathless and fluoroscopy-free FURSL are effective and safe for renal stone management, especially for stones under 2 cm in diameter. This process is a feasible option for avoiding sheath complications, which can protect surgeons from the negative effects of radiation.
1. Introduction
Treatments for renal stones have changed dramatically over recent years, with shockwave lithotripsy (SWL), flexible ureterorenoscopy (URS), and percutaneous nephrolithotomy (PCNL) being the most common minimally invasive treatment techniques with the highest stone-free rates (SFR) and minimal morbidity [1,2].
The development of holmium laser technology and advancement in flexible URS has improved renal stone treatment by getting smaller in diameter, greater working channels, higher qualified imaging modalities, improved deflection mechanisms, and smaller stone baskets. Retrograde intrarenal surgery (RIRS) indications have been expanded and are now a common endourologic procedure used for treating renal stones with high success rates and are considered a safe,optimal treatment modality for renal stones of different sizes [1,3-8].
Despite the advantage of fluoroscopy, which assists the placement of wires, stents, and the ureteral access sheath and in reaching the stones, the radiation exposure of patients, surgeons, and operating room staff during the procedure has become a clinical concern [9]. The effects of fluoroscopy-induced ionizing radiation may be dangerous in the long term, with a potential risk of genetic mutation and secondary malignancies [10].
The ureteral access sheath (UAS) allows fast, safe, and rapid repeated entrance into the collecting system, lowers the intrarenal pressure, improves visibility, and increases the ureteroscope lifespan. However, the safety of its routine use remains controversial; there are concerns related to UAS use about damage to the ureteric wall,ranging from urothelial abrasion to wall ischemia and ureteric avulsion [11-15].
The objective of this study was to conduct a modification of the RIRS technique, reduce the cost, and decrease radiation exposure, especially for the surgeon and intraoperative staff involved in a high-volume stone center.
2. Patients and methods
Between May 2015 and May 2017, 135 patients with renal stones treated with sheathless and fluoroscopy-free flexible reterorenoscopic laser lithotripsy (FURSL), performed by the same experienced endourologist, were prospectively evaluated. This study was approved by the local ethical committee of the University of Sulaymaniyah. The patients were counseled regarding treatment options, procedure,potential complications, possible need for a staged procedure to obtain satisfactory stone clearance, auxiliary procedures, and failed procedures. Following this counseling session, informed consent were obtained.
The stone size and location within the renal collecting system were not used as exclusion criteria; however, patients with a diagnosis of tumor, ureteral stricture, or very tight ureter vesical junction, or those who require fluoroscopy to navigate the stones, were excluded.
Laboratory tests included complete blood count, blood biochemistry, coagulation parameters, urine tests, and culture analyses, which were evaluated preoperatively in all patients. Those found to have urinary tract infections(UTI) were treated with a culture-specific antibiotic, and surgery was planned once their urine became sterile.
Renal stone size and location were assessed preoperatively by a non-contrast spiral CT (NCCT). In cases of a radiopaque stone, the assessment was conducted with a combination of radiography of the kidneys, ureters, and bladder (KUB) and renal ultrasonography. The stone size was defined by the greatest diameter of the largest single renal stone.
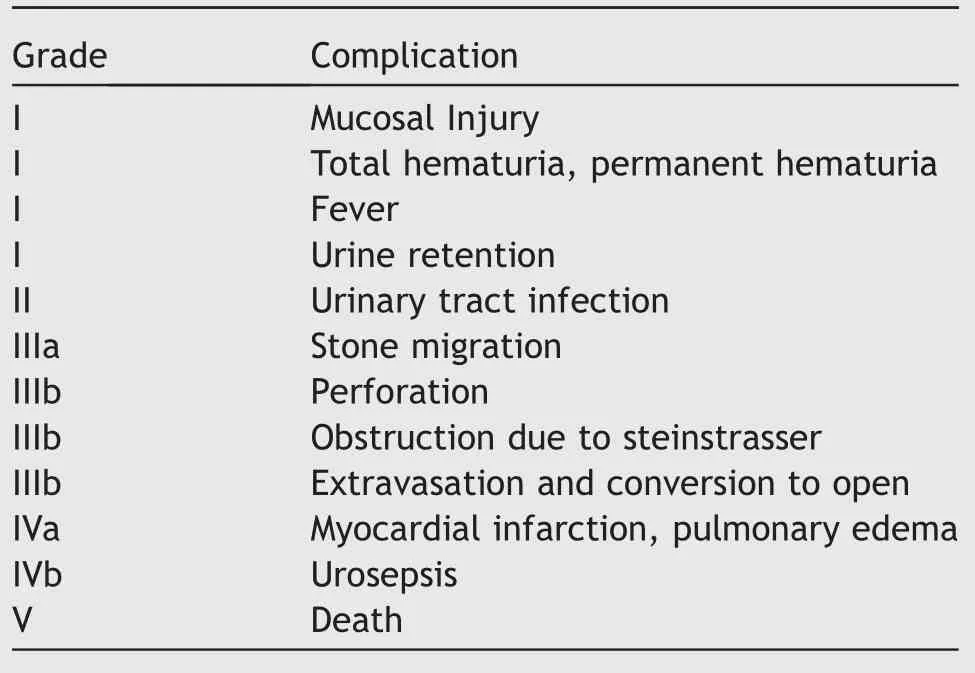
The recorded clinical parameters were gender,age,and evaluated stone parameters, such as laterality, stone location, number of stones, stone size, and previous treatment for stone removal. Other evaluated parameters included preoperative stent placement, operation time(excluding anesthetic time), lasing time, stone-free rate,hospital stay, and additional complications. Complications were assessed according to the Clavien classification system [16] (Appendix 1).
The first follow-up evaluation was performed at 10-14 days after the operation(at the time scheduled for double-J removal). Subsequent evaluations were performed at 6 weeks and 3 months with a series of abdominal radiographs of KUB and ultrasonography(US).
Immediate stone-free status was checked at the end of the endoscopic procedure when stone treatment was completed.
Results were classified as completely stone-free, clinically insignificant residual fragments (CIRFs)-defined as≤4 mm non-obstructing, non-infectious-and asymptomatic residual fragments [17]; the residual stones were defined to be >4 mm or symptomatic stones.
2.1. Technique
All patients received prophylactic antibiotics preoperatively with preoperative and intraoperative forced diuresis(fluid and diuretics) as a renoprotective measure against pyeloparenchymal reflux. A fluoroscope and UAS were not intended to be used in any case.
FURSL was performed under general or spinal anesthesia; patients were placed in a lithotomy position, prepared, and draped. Before FURSL, a semi-rigid ureteroscope 8.0-9.5 Fr (Karl Storz Endoscopy, Tuttlingen,Germany) was routinely used in all patients, allowing the ureter to be passively dilated and assessing the presence of coexisting ureteral stones or strictures.
A 0.032/0.035-inch 150 cm zebra nitinol guidewire with a flexible tip (5-7 cm) with a stiff body (Boston Scientific,Marlborough,Massachusetts,USA)was inserted through the ureteroscope up to the ureteropelvic junction (UPJ) to ensure that the flexible tip of the guidewire was stable in the renal pelvis; thereafter, the semi-rigid ureteroscope was withdrawn and the guidewire was left inside the renal collecting system.
Subsequently, a 7.5 Fr flexible URS (Storz Flex-X2, X2S Tuttlingen, Germany) was passed over the guidewire in a monorail fashion.
The urethra was straightened to avoid kinking,advancing the scope with the direct tip using the thumb and index finger of the left hand; the assistant kept the wire under slight tension.An 8 Fr feeding tube was inserted into the bladder to maintain drainage and avoid the bladder filling during the procedure.
Once the flexible ureteroscope was advanced through the UPJ, the guidewire was removed. After improving the endoscopic vision and clearing the system, the pelvicalyceal system was systematically inspected, using manual irrigation. For multiple stones or lower pole stones, irrigation was used to gather stones into the more accessible renal calyx.
Once the stone was identified, a 230 μm laser fiber was gently advanced to contact the stone; lithotripsy was performed using the Calculase II Holmium:YAG Laser Generator(Storz, Tuttlingen, Germany).
The dusting technique was used during the procedure;this approach implies the fragmenting of stones into tiny pieces or a fine powder to eliminate the necessity for stone retrieval. Basket extraction of the residual fragments was not performed. With a laser setting of 0.6-0.8 J at 10 Hz,the calculus comminuted completely, and stone fragments were deemed small enough to pass spontaneously.
After the completion of lithotripsy, the laser fiber was withdrawn; the calyx was flushed with saline using a manual irrigating pump to clear the fragments, and a close inspection of all calices allowed the determination of an endoscopic stone-free status.We placed the guidewire into the renal pelvis or collecting system under direct endoscopic vision; the flexible ureteroscope was withdrawn slowly under vision,inspecting the ureter in its entirety for larger calculi or fragments and significant ureteral trauma.
At the end of the procedure, we routinely placed a 5-6 Fr double-J stent for 10-14 days alongside an indwelling Foley catheter for about 6-12 h.
A double-J stent was placed over the guidewire under direct endoscopic vision, and the semi-rigid ureteroscope was replaced into the bladder. After that, the stent was passed under direct vision until the distal tip of the stent was 1-2 cm outside the ureteric orifice; following this observation, the guidewire was removed. Observation of the full coil of the double-J stent in the urinary bladder marked the procedure’s completion.
Data were analyzed using the Statistical Package for Social Sciences(SPSS,version 19,IBM Corporation,Armonk,New York, USA). The Chi-square test of association was used to compare between proportions. When the expected count of more than 20% of cells of the table was under 5,Fisher’s exact test was used. Student’st-test was used to compare the means of the two groups. Ap-value of <0.05 was considered as statistically significant.
3. Results
The present study population comprised 135 patients with a mean age of 40.65±12.96(range:3-70)years,including 85(62.96%) males and 50 (37.04%) females who underwent sheathless and fluoroscopy-free FURLS for the treatment of renal stones between May 2015 and May 2017.
The mean stone size was 17.23±6.69 mm (range:8-41 mm). Of the study population, 92 (68.15%) patients had a single stone, while 43 (31.85%) had multiple stones.
Stones in the renal pelvis were found in 76 patients(58.30%), while 29 (21.48%) and 30 (22.22%) patients had stones at the lower and upper/middle calyx, respectively.
Preoperative stents were present in eight(5.9%)patients when referred for FURLS, and 37 patients (27.4%) had a history of previous stone-related interventions, which included URS(10.37%),SWL(7.4%),PCNL(5.92%),and open renal stone surgery (3.7%).
Nine(6.67%)patients had renal anomalies,including two cases with pelvic kidney,two with malrotated kidneys,one with a horseshoe kidney, one with a double moiety, and three cases with pelviureteric obstruction.
Comorbidities included hypertension in 33 patients(24.44%), diabetes mellitus in 22 (16.30%), and chronic renal disease in 10 (7.41%) patients. Additionally, five(3.70%) patients were operated upon while still receiving anticoagulant therapy in the form of clopidogrel. The demographic data of patients and stone characteristics were summarized in Table 1.
The mean operative time was 32.47±10.09 min (range:13-60 min); the mean lasing time was 22.15±8.68 min(range:6-45 min).All patients without complications were discharged on the first day,whereas others were discharged on the second postoperative day with a mean hospital stay of 19.29±8.83 h (range: 10-48 h). Double-J stents were placed in all 135 patients at the end of the operation.
The complete final stone-free rate was achieved in 90.37%of patients while in two patients (1.48%), clinically insignificant residual stones measuring ≤4 mm in diameters were detected.Eleven(8.15%)patients had residual stones >4 mm.
The immediate endoscopic stone-free rate was achieved at 32.59%, while after 2 weeks, 6 weeks, and 3 months,these rates were 73.33%,90.37%,and 90.37%,respectively.Patients with residual stones were treated with SWL and only one patient developed steinstrasse post-SWL, which necessitates semi-rigid URS and FURLS for stone clearance.
Better clearance of stones was achieved in the renal pelvis (93.42%) compared to upper/middle calyx stones(86.66%) and lower calyx stones (86.20%). However, the difference was not statistically significant (p=0.39).
The final stone-free rate of 94.79% was achieved in patients with renal stones <2 cm, while SFR of 80.00% was achieved for stones ≥2 cm. Fig. 1 shows the SFR according to the stone size.
Perioperative complications occurred in 23 patients(17.04%). These complications were largely minor-12.5%were Clavien I,4.3%were Clavien II,and 0.7%were Clavien IIIb. No serious or major complications (higher Clavien grade) were observed. Neither ureteral injury when the flexible ureteroscope was withdrawn after lithotripsy nor malposition of the double-J stent was identified with plain radiography on the first scheduled visit after 10-14 days.
Complications were fever (temperature above 38.2°C)(Clavien I)in 17(12.6%)patients,pyelonephritis(Clavien II)in four (2.9%), subcapsular hematoma (Clavien II) in one(0.7%),and steinstrasse(Clavien IIIb)in one(0.7%).All were treated conservatively except the patient with steinstrasse, who needed surgical intervention (semi-rigid URS and FURLS). Patients with UTIs were admitted to the hospital for intravenous antibiotics and discharged after 48 h;they fully recovered in 10 days.
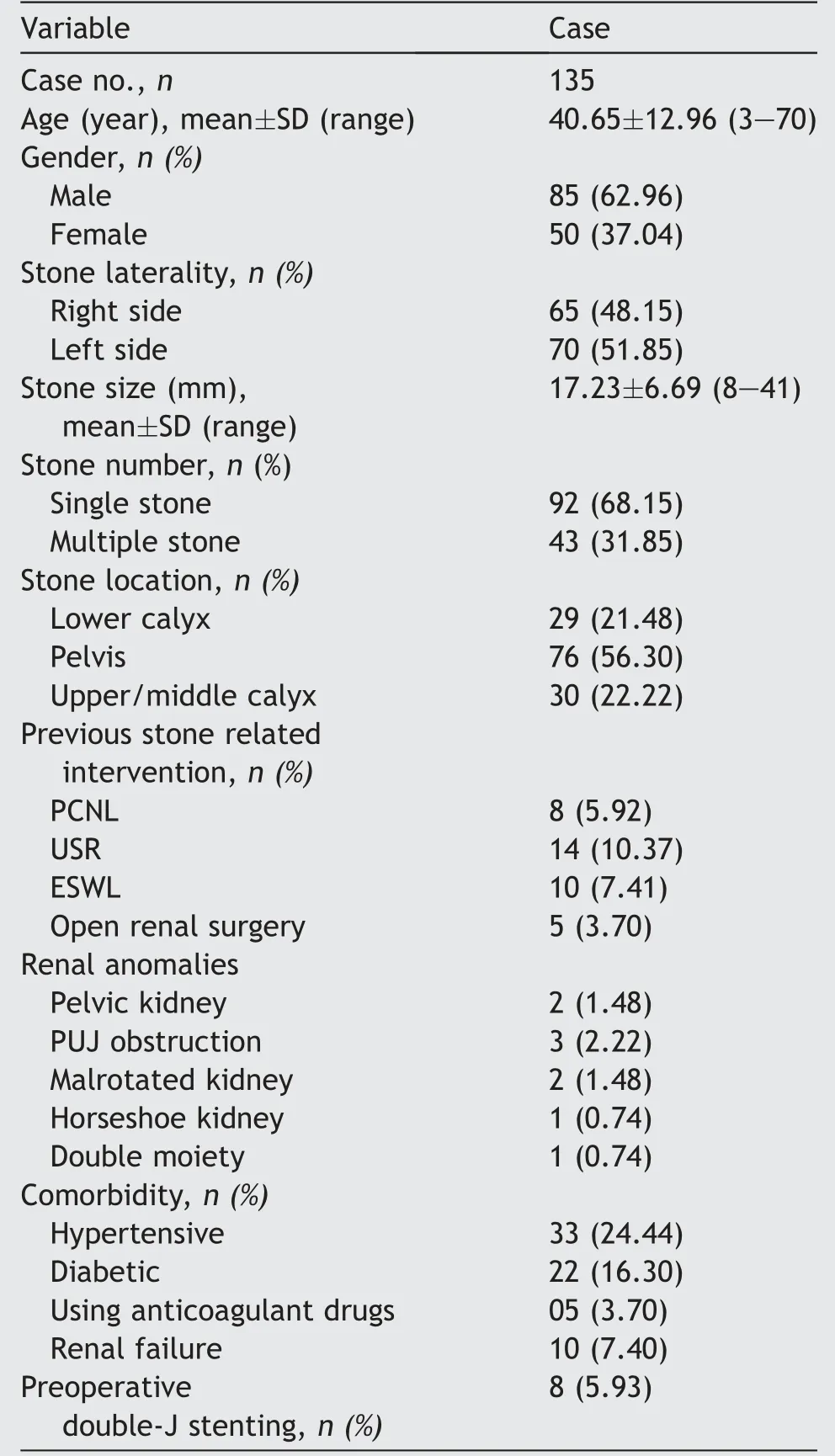
Table 1 The demographic data of patients and stone characteristics.
A female patient with subcapsular hematoma had a single pelvic stone of 2 cm in the kidney.We first used semirigid URS and completed the procedure with flexible URS,which was accidentally diagnosed after 2 weeks at the time of double-J removal when we performed ultrasonography routinely. Her condition resolved after 3 months without sequelae.
Of the study participants, 8.7% of patients with stone size <2 cm developed complications, while 30.76% of patients with stone size ≥2 cm developed complications(Fig.2).The distributions of complications according to the stones’ location were as follows: Renal pelvis, 21.05%;lower calyx,20.68%;and upper/middle calyces, 13%(these were not statistically significant). Further perioperative outcomes were described in Table 2.
Stone size ≥2 cm, operative time ≥30 min, and lasing time ≥20 min were significantly associated with higher complication rates and lower SFR upon univariate logistic regression analysis (p<0.05). In contrast, the location and number of stones did not affect SFR and complications(p>0.05) (Table 3).
4. Discussion
FURSL has grown into the most interesting endourologic procedure alternative to PCNL for the treatment of renal stones of various sizes [1,3-8]. FURSL is well endorsed by patients since the affliction is minimal and usually does not require a longer hospital stay or extended absence from work.In addition to the minimal opportunity for blood loss,renal parenchyma damage and renal impairment are also mitigated [18-24].
Despite the several advantages of fluoroscopy, which increases procedural safety, through assisting the placement of wires,stents,and UAS and in the navigation of the stones[9,10,25-28],the exposure to radiation for patients,surgeons, and operating room staff during the procedure has become a clinical concern since the effects of fluoroscopy-induced ionizing radiation may be dangerous in the long term,with a potential risk of genetic mutation and secondary malignancies [9,10,30,31].
Technological advances in flexible URS, such as the ability to get smaller and higher image quality, facilitate navigation of the ureter, renal pelvis, and calyces with excellent visualization and increase the experience of the urologist positively,have made flexible URS safer and more effective, allowing the achievability of radiation-free URS[27,32-36]. Several studies have demonstrated that reduced radiation and fluoroless protocol during flexible URS can be done safely, including UAS insertion, balloon dilation, and the placement of double-J stents, with no impact on the operation’s success, time, or complication rates; thus, this process does not increase technical difficulty [27,30-41].
In our study, flexible URS without a fluoroscopic guide was successfully performed in all patients. The initial guidewire was inserted under visual guidance using a semirigid ureteroscope, thus omitting the use of fluoroscopy in this step. Subsequently, a 7.5 Fr flexible URS was passed over the guidewire in a monorail fashion; after that, the stones were reached, and fragmentation was conducted under direct vision.
From these results,we conclude that fluoroless FURSL is a safe and feasible procedure with high SFR and low morbidity compared to other studies [39-41].
UASs can significantly expedite RIRS and increase the likelihood of stone-free status by granting multiple reentries into the kidney;furthermore,UAS lowers intrarenal pressure, perhaps improving vision during the procedure and saving the scope from damage.
Since the UAS is placed in a fragile luminal organ, the ureter,there is a potential to cause damage to the ureteral wall in different grades, ranging from simple urothelial abrasion to wall ischemia and ureteric avulsion [11-15].Accordingly, the safety and reliability of UAS-inflicted acute and long-term damage should be explored, which makes routine use of UAS a matter of debate and thus is controversial [42-45].
We used a dusting mode during the procedure, where stones were fragmented into tiny pieces or a fine powder to opt out of stone retrieval. The calculus was completely comminuted, and stone fragments were deemed small enough to pass spontaneously. This technique rebuts the main advantage of using UAS (multiple re-entries into the collecting system) and hence the risk of ureteral injuries is greatly reduced.
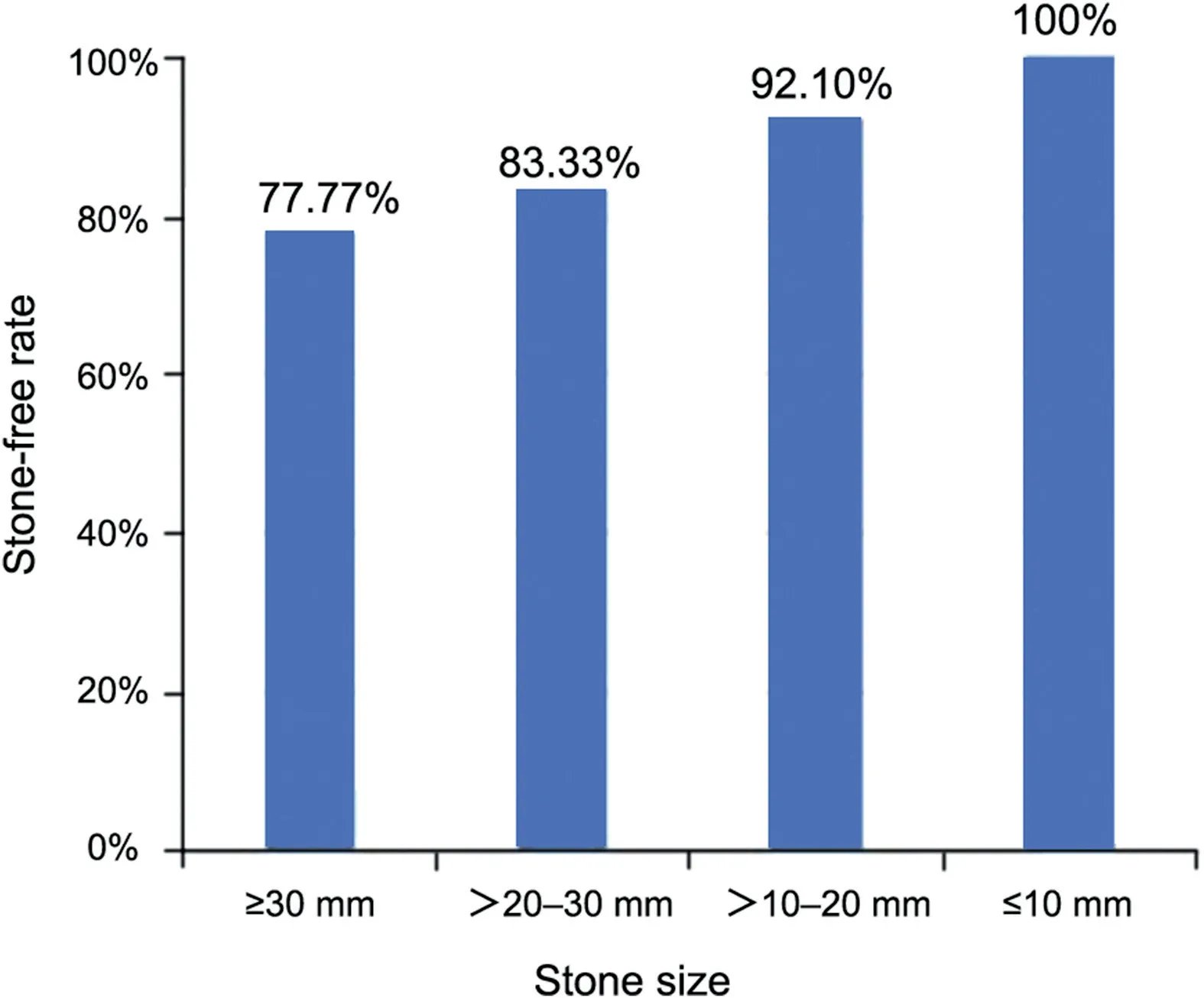
Figure 1 Stone-free rate according to the stone size.

Figure 2 Incidence of complication according to the stone size.
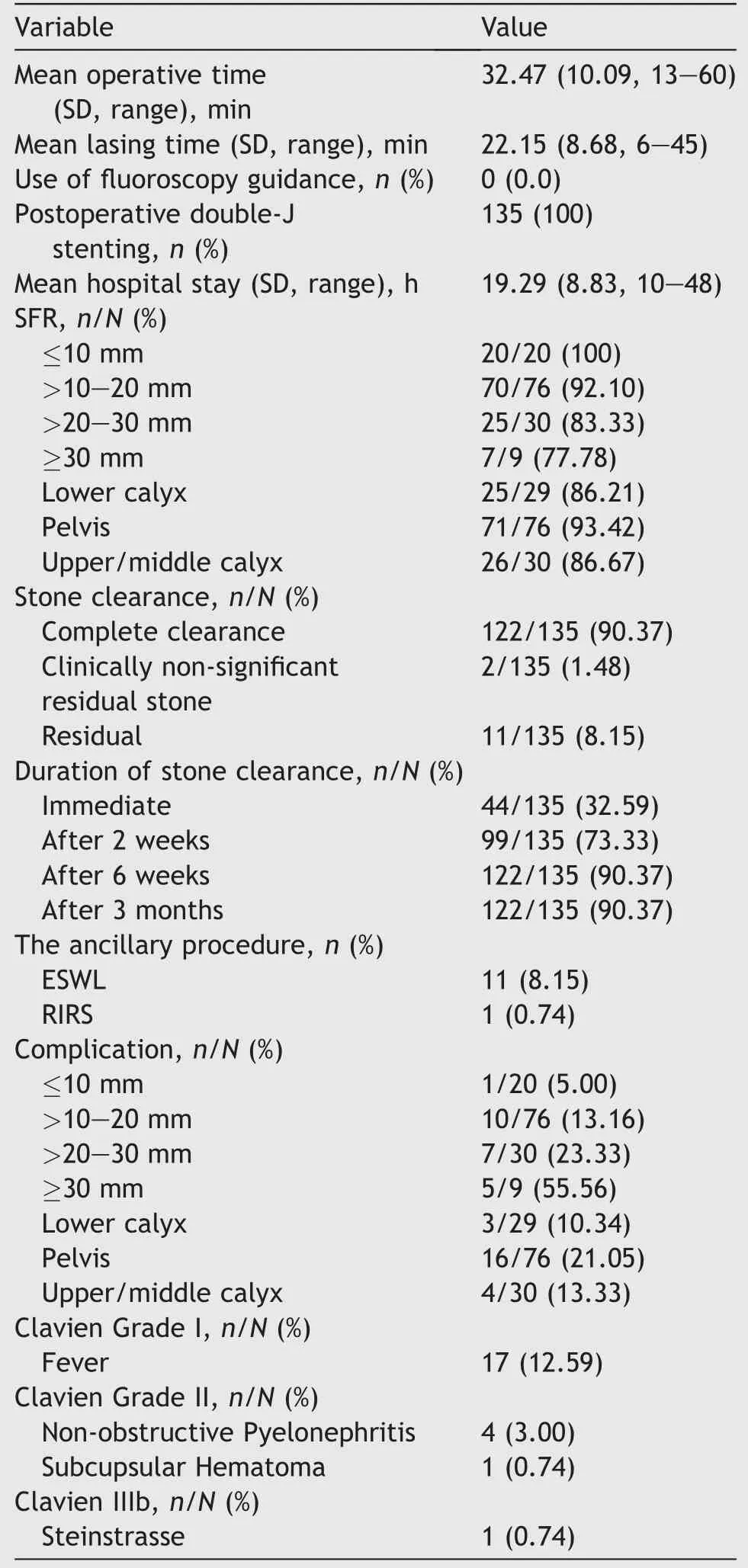
Table 2 Perioperative outcomes.
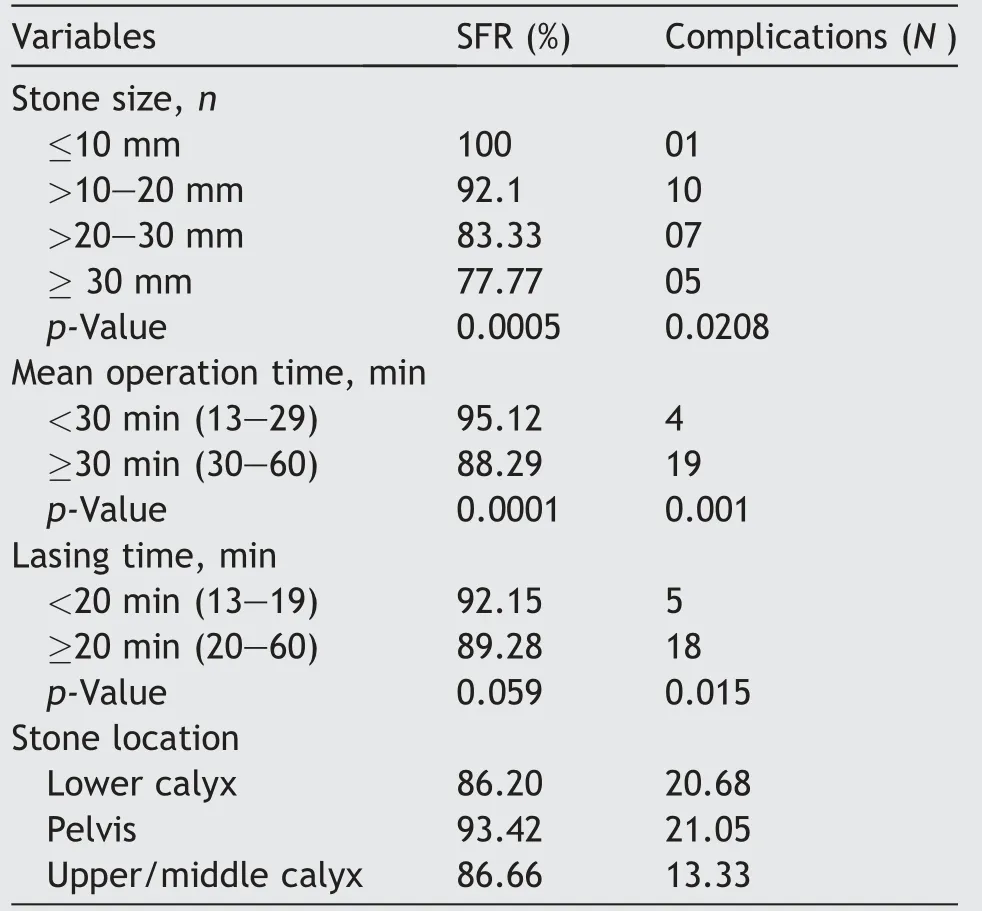
Table 3 Univariate logistic regression analysis for SFR and complication.
In the present study,the SFR was 90.37%after 6 weeks of intervention. This finding is proportionate to comparable studies that determined the SFR of 65%-92%[2,39-42,47-50]. Moreover, the results were related to stone size; the highest SFR (100%) was achieved in stones<10 mm, and the lowest SFR (77.7%) in stones >30 mm(p=0.0005).However,we noted that the finer clearance of stones was achieved in the renal pelvis (93.42%) compared to the upper/middle calyx stones (86.66%) and lower calyx stones (86.20%), but the difference was not statistically significant (p=0.393).
Stone size ≥2 cm, operative time ≥30 min, and lasing time ≥20 min were significantly associated with higher rates of complications and lower SFR on univariate analysis (p<0.05). In contrast, the location and number of stones did not affect SFR nor complications (p>0.05).
Our findings are consistent with those reported in the literature, which conclude that SFR is influenced by multiple factors, including stone size, location, number of stones, stone composition, renal anomaly, lower poleinfundibulopelvic angle, gender, use of UAS, and operator experience [50-55].
The comprehensive complication rate in this study was 17.03%, which is comparable with the prospective multicenter European study on flexible URS for the management of renal stones [57] and the data from EAU guidelines on urolithiasis that reports a global complication rate between 9% and 25% [57].
The main complication observed was a postoperative fever in 17 patients (12.59%); 78% had a stone >20 mm in size, and more than half had a stone >30 mm. All were treated with intravenous fluids and antipyretics. Only four patients developed postoperative UTI; all four had stones>30 mm, and improved following administration of antibiotics and conservative management. It was obvious that longer operative time and larger stone size were important factors in the development of such fever.
Continuous irrigation was required to facilitate good vision for the surgeon during the operation. However,irrigation-induced increase in intrarenal pressure remains a concern, since it may cause systemic inflammatory response syndrome (SIRS) due to increased pyelovenous and pyelolymphatic absorption. Besides bacteria, bacterial endotoxins can enter the bloodstream along with perfusion fluid absorption and thus cause fever or SIRS[58-61].
Stone size,operative duration,and the rate of irrigation are crucial risk factors for post-RIRS fever and SIRS. These complications may be caused by an increase in the opportunity to injure the mucosa of the renal pelvis with the holmium laser and prolong operative time in the management of large renal stones [60,62,63].
In this study, we observed that stone size and operative duration were independently associated with the development of post-RIRS fever.
The present study shows a significantly lower SFR and a higher risk of fever and UTIs for stones >20 mm compared to smaller ones.It was concluded that sheathless FURLS is a safe and feasible procedure with high SFR and low morbidity, especially for stones <2 cm. Furthermore, the use of UAS when performing ureteroscopy was not consistently fundamental when treating kidney stones. The findings agree with those reported in the reviewed literature. The Clinical Research Office of the Endourological Society’s (CROES) URS Global Study by Traxer et al. [64]showed no difference in SFR, regardless of the use of UAS. However, the use of UAS did not increase the possibility of ureteral damage or bleeding, although postoperative infectious complications were reduced.
In another CROES study by Skolarikos et al. [65] for solitary renal stones, UAS was used in most cases. The SFR negatively correlated with stone size; there was no distinction in the overall complication rate owed to stone size. However, patients with a stone >20 mm showed a higher probability of fever after flexible URS than those with a smaller stone.
Hyams et al. [15] and Geraghty et al. [66] reported a multi-institutional series of URS/laser lithotripsy for renal stone sizes between 2 and 3 cm. They found no difference in the SFR, complications rate, or the average number of procedures per patient, regardless of applying UAS in stones >2 cm.Both studies concluded that the use of UAS is not constantly crucial when treating large renal stones since there was no significant difference in the outcome with its use.
The drawbacks of our study include the imaging methods used to assess SFR. Although CT is the most precise method for determining residual fragments,logistical reason and high cost may restrict its conventional use [67,68]. Ultrasonography and KUB were used as a postoperative imaging test based on their low value,ready accessibility, and low dose of radiation. This may have caused an inaccurate measurement of the residual stones,due to the difference in the accuracy between the imaging methods.
Furthermore, all operations were conducted by a single experienced endourologist due to the high price of a flexible ureteroscope to minimize the damage of scope, which is an intrinsic bias. Hence, the generalizability of the techniques may be limited.
Moreover, this technique may be helpful in decreasing operative time due to the free mobility of the intraoperative team, preventing the movement of the fluoroscope in and out of the operating table.This process would be more comfortable for the surgeon since using aprons and protective shields can thus be avoided.
5. Conclusion
Sheathless and fluoroscopy-free FURSL are effective and safe for renal stone management, especially for stones under 2 cm in diameter. FURSL is thus a feasible option for avoiding sheath complications, which can protect surgeons from the negative effects of radiation.
Author contributions
Study concept and design: Sarwar Noori Mahmood.
Data acquisition: Hewa Toffeq.
Data analysis: Hewa Toffeq.
Drafting of manuscript: Saman Fakhraldin.
Critical revision of the manuscript:Sarwar Noori Mahmood.
Conflicts of interest
The authors declare no conflict of interest.
Appendix 1. Modified Clavien grading system
 Asian Journal of Urology2020年3期
Asian Journal of Urology2020年3期
- Asian Journal of Urology的其它文章
- Androgen receptor: Functional roles and facets of regulation in urology
- Mesenteric metastases from mature teratoma of the testis: A case report
- Intractable hematuria due to giant prostatic hyperplasia effectively treated with prostatic artery embolization
- Efficacy and safety of degarelix in patients with prostate cancer:Results from a phase III study in China
- Survival after radical cystectomy for bladder cancer: Multicenter comparison between minimally invasive and open approaches
- Androgen receptor in bladder cancer: A promising therapeutic target
