The clinical efficacy analysis of radiofrequency ablation combined with chemotherapy in treating late non-small cell lung cancer
Ying-Ying Liu, Feng Xu
Ying-Ying Liu1, Feng Xu2,*
1Chengde Medical University, Chengde, 067000, China.2Department of Respiratory and critical Medicine, Cangzhou people¢s Hospital, Cangzhou, 061000, China.
: To study the short-term efficacy and improvement effect on the quality of life of CT guided radiofrequency ablation(RFA) in treating late non-small cell lung cancer.: 317 patients with non-small cell lung cancer (87 cases in the observation group and 230 cases in the control group) were selected for propensity score matching, with a matching tolerance of 0.05, and 42 pairs were successfully paired. The changes in chest enhanced CT before and 3 months after treatment and the quality of life measurement scale EORTC QLQ-C30 in Chinese version were evaluated.: The disease control rate of the observation group was 88.09%, which was significantly higher than that of the control group (61.91%). The functional and symptom scores of the two groups after treatment were significantly better than those before treatment, and the indicators of the observation group after treatment were better than those of the control group (< 0.05).: CT-guided radiofrequency ablation combined with chemotherapy is safe and effective in the treatment of NSCLC, which can control local tumor progression, reduce tumor burden, and improve the quality of life of patients with advanced NSCLC.
CT guided, Radiofrequency ablation, Non-small cell lung cancer, QLQ-C30
CT-guided radiofrequency ablation combined with chemotherapy may be one effective method for the treatment of advanced non-small cell lung cancer (NSCLC).
Radiofrequency ablation is a precise treatment, which may improve disease control rate and the life quality of patients with NSCLC.
Introduction
The incidence and mortality of lung cancer rank first in malignant tumors in China [1]. There are many methods for the treatment of non-small cell lung cancer (NSCLC), including systemic therapy and topical therapy. Systemic therapy includes chemotherapy, radiotherapy, targeted therapy, and immune cell therapy. Local treatment includes surgery, radiofrequency ablation, 125I radioactive particle implantation, local perfusion chemotherapy,., and each method has its advantages and disadvantages. The combination of these methods to treat advanced NSCLC requires more research, especially for patients with NSCLC who have lost their chance of surgery in the late stage. The proportion of elderly patients with lung cancer increases year by year in China. Although surgery is the first choice for the treatment of lung cancer, most patients have lost the chance of surgery at the time of initial diagnosis. Only 20-30% of patients with lung cancer are suitable for radical surgery [2]. Radio Frequency Ablation (RFA), as a precise, minimally invasive, and reproducible treatment, has been widely used in clinical practice in recent years, providing a local treatment opportunity for patients with advanced lung cancer who cannot undergo surgery [3]. Since 2000, domestic and foreign scholars have reported radiofrequency ablation for lung tumors [4]. This technique is widely used in the treatment of lung cancer [5]. Radiofrequency ablation can be performed by CT, ultrasound, magnetic resonance, C-arm CT, PET- CT, CT-fiber bronchoscopy, magnetic navigation bronchoscopy, and other platform operations [6-8]. Until now, the most common and most accurate way is CT guidance. Percutaneously puncture the tumor under CT guidance, open the sub-electrode needle, and emit the AC frequency conversion high-frequency current with the frequency of 460~480kHZ, so that the ions in the tumor cells oscillate at high speed, energy is converted, and a large amount of heat energy is generated. When the temperature reaches 60~100°C, the tumor cells are necrotic, and the blood vessels and lymphatic vessels around the tumor undergo coagulation and necrosis in a high-heat environment, which can block the blood supply of the tumor and the metastasis pathway of the tumor cells.
Materials and Methods
Clinical data
A total of 317 patients with advanced (IIIB~IV) non-small cell lung cancer who were hospitalized in the Department of Respiratory and Critical Care Medicine of Cangzhou People's Hospital from October 2017 to October 2018 were included in our study. The patient’s cohort was subdivided to two groups, which including 87 patients in the observation group and 230 patients in the control group. The observation group received first-line chemotherapy combined with radiofrequency ablation, and the control group received first-line chemotherapy. In this observational study, because of the imbalance between the groups, in order to reduce the bias, propensity score match (PSM) was used to deal with the imbalance between the two groups. The principle of PSM was to calculate each patient's disease by logistic regression. The relevant baseline covariates are used to derive their respective scores, and then the two individuals with similar scores are paired. We included gender, age, tumor diameter, stage, classification into matching variables, and the matching tolerance was set to 0.05. As a result, 42 pairs of patients were successfully matched. Results showed that the average age was 64.21 ± 9.19, the gender composition was 16 males and 25 females, the tumor type composition was 32 cases of adenocarcinoma and 10 cases of squamous cell carcinoma, the tumor stage composition was 30 cases of stage IIIB and 12 cases of stage IV, and the tumor size was 30 cases of tumor diameter ≤ 3cm and 12 cases of tumor diameter > 3cm. As in the control group, the average age was 64.83 ± 9.24, the gender composition was 17 males and 26 females, the tumor type composition was 33 cases of adenocarcinoma and 9 cases of squamous cell carcinoma, the tumor stage composition was 31 cases of stage IIIB, 11 cases of stage IV, and the tumor size was 31 cases of tumor diameter ≤ 3cm, and 11 cases of tumor diameter > 3cm. There were no significant differences in gender, age, tumor diameter, stage, and type between the two groups (> 0.05) (Table 1).
Radiofrequency ablation and CT equipment
The WE7568II radiofrequency tumor ablation instrument produced by Beijing Erfu Electronics Co., Ltd. was used. The treatment temperature was set to 90 °C. The single-pole radiofrequency ablation motor needle was used to form a high-temperature coagulation zone with a diameter of 5 cm. The high-temperature treatment of the multi-site target area was implemented, and the electrocoagulation mode was turned on when the needle was withdrawn to prevent the needle cell metastasis and bleeding of the tumor cells. This equipment was used by Neusoft medical X-ray computed tomography equipment NeuViz128 CT, radiofrequency ablation treatment, and postoperative follow-up.
Treatment methods
One day before radiofrequency ablation, the patient was trained to breathe at rest, and the water was fasted 2 hours before surgery. According to the location of the patient's tumor, choose the supine position, prone position or lateral position. Select the appropriate puncture point by CT positioning, measure the distance and angle between the lesion and the puncture point. Disinfecting with puncture point as the center, disinfection radius > 15cm, localized 2% lidocaine infiltration anesthesia after puncture point, puncture the electrode needle to the distal end of the tumor, radiofrequency ablation of the tumor when CT confirms that the electrode needle is in the predetermined position , each target ablation time 10~15min, temperature setting 90°C. For tumors with diameter > 5cm, repeated CT positioning, multiple ablations from far to near, superimposed ablation of the target to ensure coverage of the entire tumor, complete sub-electrode recovery after ablation, electrocoagulation of the needle to prevent needle implants and to bleed. After the electrode needle was pulled out, CT was scanned to observe whether there was pneumothorax or hemothorax. If the pneumothorax occurred during the operation, the closed thoracic drainage was immediately performed. After returning to the ward, the patient was closely observed for fever, hemoptysis, chest pain, and delayed pneumothorax, preventing the occurrence of concurrent certificates and promptly processes the concurrent certificates that have occurred.
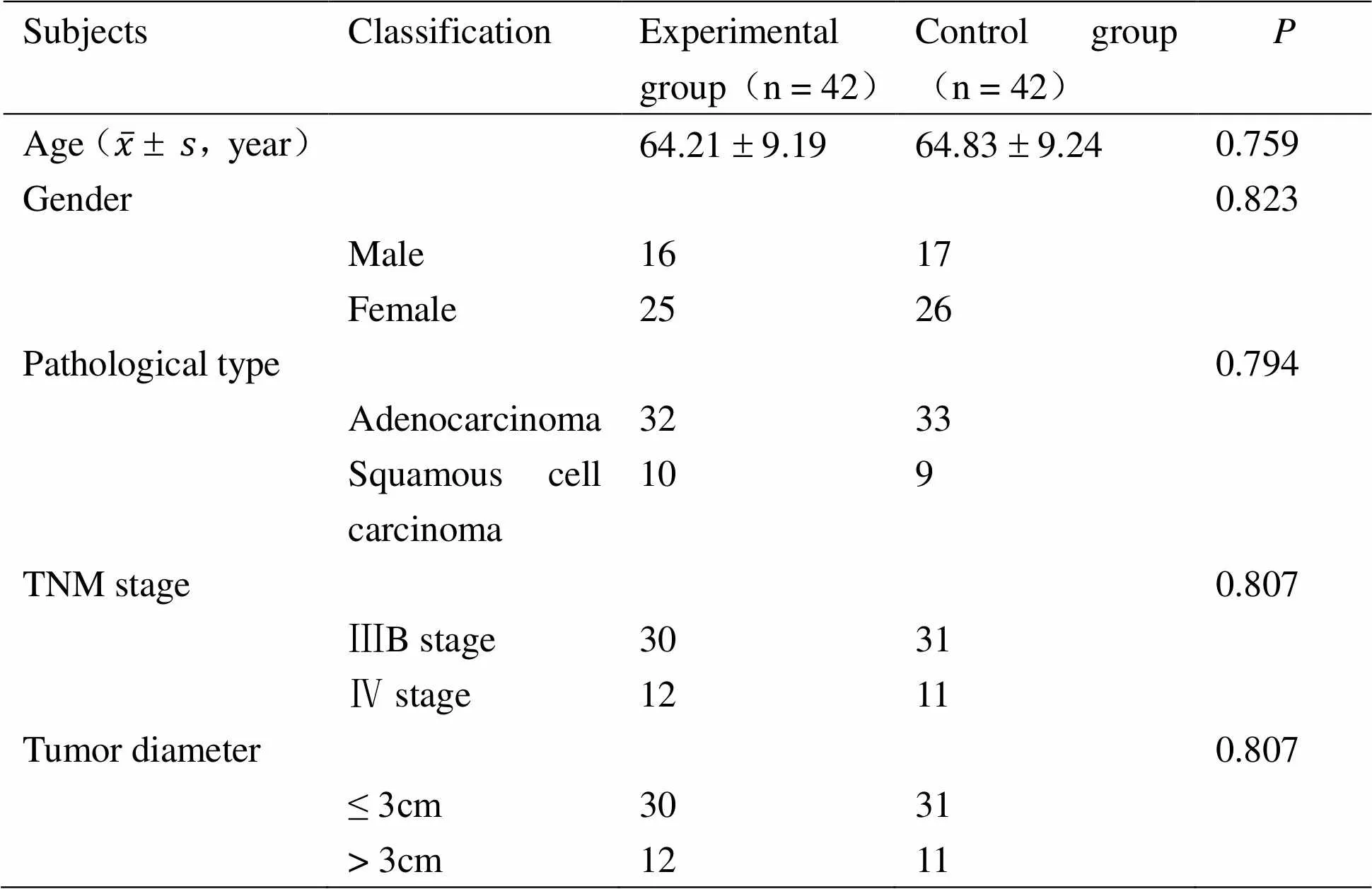
Table 1 Baseline comparison of two groups of patients
Efficacy evaluation
CT examination was performed every month after operation to observe the tumor size and blood supply. The therapeutic effect was evaluated using the RECIST version 1.1 efficacy evaluation criteria. Complete remission (CR): All target lesions disappeared completely, and no new lesions appeared at least 4 weeks. Partial remission (PR): the maximum diameter of target lesions after treatment decreased by ≥ 30%, at least maintained 1 week. Stabilization of disease (SD): the maximum diameter of the target lesion shrinks less than PR or increases not reached progression disease (PD). PD: the sum of the maximum diameter of the target lesion increases by at least ≥ 20 %, or new lesions appear disease control rate (DCR): cases including CR, PR, and SD.
Quality of Life Assessment
The quality of life assessment scale is based on the “Quality of Life Questionnaire 30 (QLQ-C30)” recommended by the European Cancer Research and Treatment Organization (E0RTC). QLQ-C30 is suitable for all tumor patients and is an important tool for quality of life assessment of patients with various types of cancer [9]. The questionnaire contains 30 questions, divided into functional areas, symptom areas, and total health status. Functional proportion includes: physical function, role function, emotional function, cognitive function, and society. Function 5 items. The symptoms proportion contains fatigue, nausea and vomiting, pain, shortness of breath, insomnia, loss of appetite, constipation, diarrhea, and other items. In order to facilitate the comparison of scores in various fields, the differential transformation method is applied to perform the linear transformation, and the score is converted into a standardized score within 0-100.
Statistical methods
SPSS25.0 software was used for data analysis. The two groups of patients were paired with the method of preference score matching analysis to reduce the mixed factors of gender, age, tumor diameter, stage, and typing in the two groups. The chi-square test is applied to the count data, and the measurement data in the QLQ-C30 Chinese version questionnaire is expressed by (`x ± s). The paired sample t-test was used before and after treatment in the group, and for two independent samples, student t test was used for comparison between groups.< 0.05 was treated a statistical difference.
Results
Comparison of disease control rate between the two groups
The study showed that 11 patients in the observation group reached CR 3 months after radiofrequency ablation, 13 patients had PR, 13 patients had no change, and 5 patients showed PD and the disease control rate was 88.09%. In the control group, 7 patients reached CR, and 9 patients were PR, 10 cases did not change, and 16 cases showed PD and the disease control rate was 61.91%. The disease control rate of the observation group was significantly higher than that of the control group, and the difference was statistically significant (< 0.05) (Table 2).

Table 2 Comparison of disease control rates between the two groups of patients/case (%)
Note: CR, complete remission; PR, partial remission; SD, stabilization of disease; PD, progression disease; DCR, disease control rate.
Comparison of quality of life between the two groups
The quality of life of the two groups before and after treatment improved. The functional field scores of the observation group were significantly higher than those of the control group (Table 3), and the symptom scores were significantly lower than the control group (Table 4), the difference was statistically significant (< 0.05).
Complications and adverse reactions
Results showed that 3 patients with pneumothorax, 3 cases of pulmonary infection, 2 cases of atelectasis, and 2 cases of lower extremity venous thrombosis was observed in the control group, the incidence of complications was 23.81% (10/42). However, only 2 cases of pneumothorax, 1 case of pulmonary infection, and 1 case of atelectasis occurred in the experimental group, and the complication rate was 9.52% (4/42). The incidence of complications in the two groups was statistically significant (< 0.05). There were no allergic reactions in the two groups. The main adverse reactions were nausea, vomiting, and bone marrow suppression after chemotherapy. There was no significant difference between the two groups (> 0.05). There were no radiofrequency ablation-related deaths in the observation group. The main adverse reactions after operation were cough, fever, chest pain, hemoptysis,., which improved after symptomatic treatment.
Discussion
At present, the research on the combined treatment of NSCLC is still limited, and the treatment effect is not clear. Liu Baodong and other studies have shown that for NSCLC patients with epidermal growth factor receptor mutations, the use of epidermal growth factor receptor tyrosine kinase inhibitor-treatment can significantly inhibit the progression of primary lesions, and then radiofrequency ablation can significantly reduce the role of tumor burden [10]. This study shows that systemic plus local treatment is significantly better than simple systemic therapy. In our current study, we found that radiotherapy combined with chemotherapy for NSCLC can improve the patient's response rate on the one hand, and reduce the patient's treatment-related side effects on the other. It is indicated that radiofrequency ablation combined with chemotherapy for NSCLC has a significant effect on local control rate. These results may indicate that the combination treatment is more effective than chemotherapy only.
Further, we examined the effect of combination therapy on patient-related syndromes. Results showed that the QLQ-C30 questionnaire scores in the observation group after treatment were higher than the control group, which contains 5 functional areas such as body, role, emotion, cognition, and society, and total health status scores. The scores of fatigue, nausea and vomiting, pain, shortness of breath, insomnia, loss of appetite, constipation, diarrhea, and other symptoms were lower in the experimental group than those in the control group. Although the difference in function and symptom improvement between the two groups after treatment was statistically significant, the combination treatment group had an advantage in improving the quality of life. It is suggested that the application of radiofrequency ablation combined with chemotherapy in patients with advanced NSCLC may effectively control tumor progression and significantly improve the quality of life of patients. Domestic reports on the use of KPS scores to evaluate radiofrequency combined with radiotherapy and chemotherapy are consistent with the findings of this study [11]. Besides, studies have shown that radiofrequency ablation combined with targeted therapy QLQ-C30 questionnaire is better than the systemic treatment group in the evaluation of the quality of life in patients with advanced NSCLC [12]. Moreover, after reviewing the relevant literature, no literature on the quality of life assessment of patients with advanced lung cancer after radiofrequency ablation combined with chemotherapy was found.
Conclusion
In summary, radiofrequency ablation as a precise, minimally invasive, and reproducible treatment combined with systemic therapy for advanced NSCLC that cannot be treated surgically may improve the patient's disease control rate and improve the quality of life of patients. Although there have been many reports confirming the effectiveness and advantages of radiofrequency ablation for lung cancer, there is still a lack of large-sample, multi-center studies.
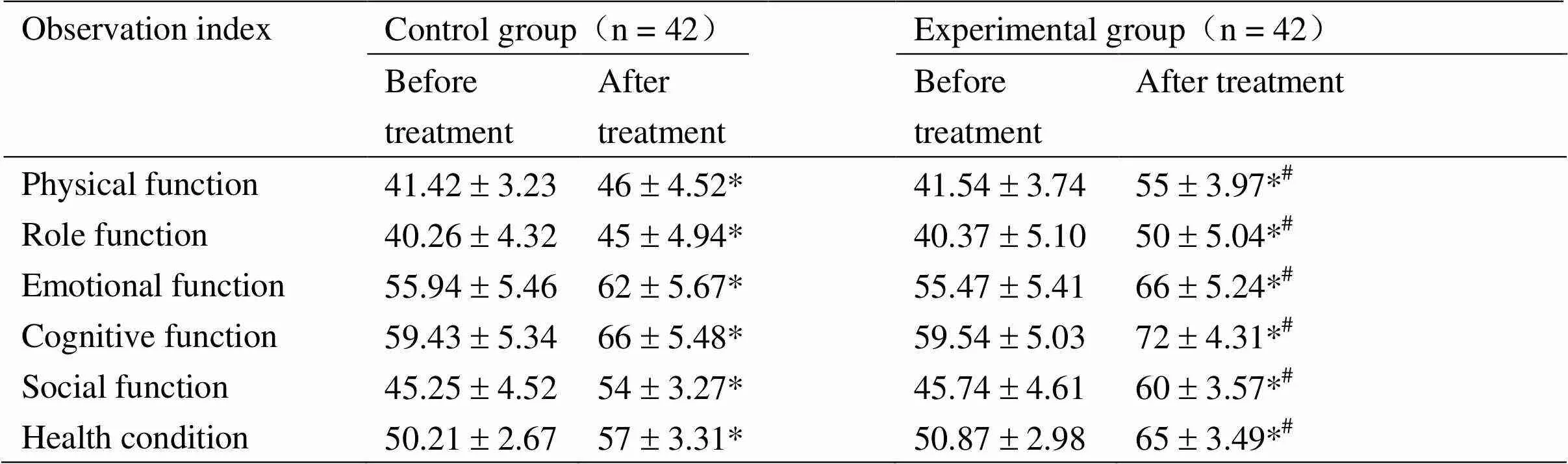
Table 3 The functional areas and total health status scores of the QLQ-C30 questionnaire before and after treatment in both groups (x ± s)
Note: * Comparison within the group: before treatment and after treatment,< 0.05; #Between groups: after treatment, the observation group compared with the control group,< 0.05.

Table 4 QLQ-C30 questionnaire symptom score before and after treatment in two groups of patients
Note: * Comparison within the group: before treatment and after treatment,< 0.05; #Between groups: after treatment, the observation group compared with the control group,< 0.05.
1. Bray F, Ferlay J, Soer JR,. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality wordwide for 36cancers in 185 countries. CA Cancer J Clin 2018, 68(6): 394-424.
2. Barthelme S, Gedert H, Boitze C,. Solitary fibroustumors/hemangiopericytomas with different vaiants of the NAB2-STAT6 gene fusion is characterized by specific histomorphology and distinct clinicopathological featureas. Am J Pathol 2014, 184(4): 1209-1218.
3. Liu Baodong, Ye Xin, Fan Weijun,. Image-guided radiofrequency ablation for the treatment of lung cancer experts (2018 edition). Chin J Lung Cancer 2018, 21(2): 76-88, 86.
4. Dupuy DE, Zagoria RJ, Akerley W,. Percutaneousradiofrequency ablation of malignancies in the lung. AJR Am J Roentgenol 2000, 174(1): S7-59.
5. Ng CS, Gonzalez-Rivas D, Damico TA,. Uniportal VATS-a new era in lung cancer surgery. J THorac Dis 2015, 7(8): 1489-1491.
6. Li XQ, Zhang Y, Huang DB,. Value of C-arm computed tomography in radiofrequency ablation of small lung lesions. Genetics Molecular Res 2014, 13(3): 6027-6036.
7. Kato K, Abe H, Ika M,. C-Arm cone beam computed tomography guidance for radiofrequency ablation in hepatocellular carcinoma. Oncol 2017, 92(3): 142-152.
8. Xie F, Zheng X, Xiao B,. Navigation bronchoscopy-guided radiofrequency ablation for nonsurgical peripheral pulmonary tumors. Respiration 2017, 94(3): 293-298.
9. Wan CH, Chen MQ, Zhang CZ,. Review of EORTC QLQ-C30 Chinese version of cancer patient quality of life measurement scale. J Practical Oncol 2005, (4).
10. Liu BD, Li YH, Hu M,. Preliminary clinical application of radiofrequency ablation in the local progression of EGFR-TKIs in the treatment of non-small cell lung cancer. Chin J Lung Cancer 2016, 19(12): 859-863.
11. Zheng QC, Zhang QH, Zhai YZ,. Clinical observation of CT-guided radiofrequency ablation combined with concurrent chemoradiotherapy for locally advanced non-small cell lung cancer. Chin Medl innovation 2015, 16: 78- 80.
12. Chen XL, Fu JG, Zhang M,Effects of radiofrequency ablation combined with targeted therapy on quality of life in patients with non-small cell lung cancer. J Clin Pulmon Med 2015, 20(3): 398-401.
30 March 2019,
11 August 2019,
17 August 2019. .
Authors declare that they have no competing interests.
Hebei Province Key R&D Program (1827778ID)
?2019 TMR Publishing Group Limited. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License.
At present, the research on the combined treatment of NSCLC is still limited, and the treatment effect is not clear. At present, the therapeutic effect of combination therapy on NSCLC requires further clinical validation evidence. This article provides clinical evidence for the role of radiotherapy combined with chemotherapy in the treatment of advanced NSCLC.
Feng Xu, Department of Respiratory and critical Medicine, Cangzhou peoples’ Hospital, Cangzhou, 061000, China.E-mail: 13582711659@163.com
- Cancer Advances的其它文章
- Combination of Chinese and Western medicine in the treatment of aggressive angiomyxoma: a case report
- Treatment of undifferentiated thyroid carcinoma with darafini and trametinib: a case report and literature review
- The differences and similarities between regional ethnic medicine and traditional Chinese medicine in the prevention and treatment of cancer pain
- Research progress in the treatment of colorectal cancer in classical prescriptions