Prognostic value of 18F-fluorodeoxyglucose positron emission tomography using Deauville criteria in diffuse large B cell lymphoma treated with autologous hematopoietic stem cell transplantation
Zhitao Ying, Lan Mi, Nina Zhou, Xuejuan Wang, Zhi Yang, Yuqin Song, Xiaopei Wang,Wen Zheng, Ningjing Lin, Meifeng Tu, Yan Xie, Lingyan Ping, Chen Zhang, Weiping Liu,Lijuan Deng, Jun Zhu
1Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Department of Lymphoma, Peking University Cancer Hospital & Institute, Beijing 100142, China; 2Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Peking University Cancer Hospital & Institute, Beijing 100142, China; 3Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Department of Nuclear Medicine, Peking University Cancer Hospital & Institute, Beijing 100142, China
Correspondence to: Jun Zhu, MD. Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Department of Lymphoma, Peking University Cancer Hospital & Institute, Beijing 100142, China. Email: zhu-jun2017@outlook.com.
Abstract Objective: High-dose chemotherapy (HDC) followed by autologous hematopoietic stem cell transplantation(auto-HSCT) plays an important role in improving outcomes of diffuse large B cell lymphoma (DLBCL) patients.18F-fluorodeoxyglucose (18F-FDG) positron emission tomography (PET)/computed tomography (CT) has been widely accepted in response assessment and prediction of prognosis in DLBCL. Here, we report the value of 18FFDG PET/CT pre- and post-HSCT in predicting outcomes of patients with DLBCL.Methods: DLBCL patients who had PET/CT scan before and after HSCT were included. PET results were interpreted based upon Deauville criteria. The prognostic value of 18F-FDG PET/CT in auto-HSCT was evaluated.Results: Eighty-four patients were enrolled. In univariate analysis, pre- and post-HSCT PET findings were correlated with 3-year progression-free survival (PFS) [hazard ratio (HR)=4.391, P=0.001; HR=7.607, P<0.001] and overall survival (OS) (HR=4.792, P=0.008; HR=26.138, P<0.001). Patients receiving upfront auto-HSCT after firstline treatment had better outcomes than relapsed/refractory DLBCL patients (3-year PFS, P<0.001; 3-year OS,P<0.001). In the relapsed/refractory patients, pre- and post-HSCT PET findings were also associated with 3-year PFS (P=0.003 vs. P<0.001) and OS (P=0.027 vs. P<0.001). A significant correlation was observed between clinical response to chemotherapy before auto-HSCT and outcomes of patients in the entire cohort (3-year PFS, P<0.001;3-year OS, P<0.001) and in the subgroup of 21 patients with positive pre-HSCT PET (3-year PFS, P=0.084; 3-year OS, P=0.240). A significant association between survival and post-HSCT PET findings was observed in multivariate analysis (HR=5.168, P<0.001).Conclusions: PET results before and after HSCT are useful prognostic factors for DLBCL patients receiving HSCT. Patients who responded to chemotherapy, even those with positive pre-HSCT PET, are appropriate candidates for auto-HSCT.
Keywords: Positron emission tomography; computed tomography; autologous hematopoietic stem cell transplantation; high-dose chemotherapy; diffuse large B cell lymphoma
Introduction
Diffuse large B cell lymphoma (DLBCL) is the most common lymphoid neoplasm in adults, accounting for approximately 32.5% of non-Hodgkin's lymphomas diagnosed annually in America (1). The combination of rituximab with chemotherapy has led to a significant improvement in survival (2,3). However, approximately 40% of DLBCL patients are refractory to or relapse after standard first-line treatment (2,3). High-dose chemotherapy (HDC) followed by autologous hematopoietic stem cell transplantation (auto-HSCT) has been proven to be an important strategy for improving outcomes of DLBCL patients (4,5).18F-fluorodeoxyglucose(18F-FDG) positron emission tomography (PET)/computed tomography (CT) plays a key role in staging,response assessment and prediction of prognosis in DLBCL (6). However, the prognostic value of18F-FDG PET/CT in patients with DLBCL receiving HDC followed by auto-HSCT is still controversial (7). Our previous studies showed that post-HSCT PET/CT assessment was the main predictor of outcomes in DLBCL patients (8,9). Here, we report an updated analysis of the study on the value of18F-FDG PET/CT pre- and post-HSCT in predicting outcomes of patients with DLBCL.
Materials and methods
Patient selection
This study has been approved by the Medical Ethics Committee of Peking University Cancer Hospital, and has therefore been performed in accordance with the Declaration of Helsinki. From November 2010 to December 2017, a total of 169 patients with DLBCL received auto-HSCT. All patients gave their informed consent before inclusion in the study. One-hundred and twenty-six patients examined by PET before and after auto-HSCT were preliminarily selected. Seventeen patients with primary lymphoma of the central nervous system, 10 patients undergoing PET >3 months before or after auto-HSCT, and 15 patients who lost to follow-up were excluded. Finally, 84 patients were included and the data on these patients were analyzed.
Staging
Disease staging was determined based upon the Ann Arbor staging algorithm. Eastern Cooperative Oncology Group Performance Status (ECOG PS) score was recorded.Scores for the secondary age-adjusted International Prognostic Index (sAA-IPI) were also determined (10). One point was assigned to each of the following parameters:LDH elevation, Ann Arbor stage III/IV and ECOG PS≥2.Patients were classified into four risk groups: low, lowintermediate, high-intermediate and high, depending on the presence of 0, 1, 2, or all 3 risk factors. Bulky disease was defined as the presence of a mediastinal lesion greater than 1/3 of the transthoracic diameter or an extranodal lesion ≥7.5 cm. PET was acquired both before and after auto-HSCT.
PET acquisition and response evaluation
Patients were instructed to fast for at least 6 h before injection of 3.7 MBq/kg18F-FDG intravenously.Approximately 60±10 min post-injection, a whole-body acquisition commenced in 6-8 bed positions (1 min/bed)using a hybrid system (Gemini TF 16 PET/CT, Philips,Netherlands), and covered from the base of the skull to the upper thigh. Non-contrast enhanced CT was conducted using the following parameters: modulated 100 mAs, 120 kV,and slice thickness 3 mm for attenuation correction and anatomical localization.
PET findings were interpreted based upon Deauville criteria (5-point scale). A score of ≤3 was interpreted as negative, and a score of >3 was interpreted as positive (11).Clinical efficacy of complete response (CR), partial response (PR), stable disease (SD), or progressive disease(PD) was defined according to the Lugano classification (11).
Statistical analysis
Survival functions that were recorded by progression-free survival (PFS) and overall survival (OS) were estimated by Kaplan-Meier method and compared using the log-rank test. Prognostic factor analysis was performed by the Cox regression model. The limit of statistical significance for all analysis was defined as a P value of less than 0.05. All statistical analyses were performed using the IBM SPSS Statistics (Version 22.0; IBM Corp., New York, USA). The α-error was defined as 0.05, and all tests were two-sided.
Results
A total of 84 patients (46 males and 38 females) with DLBCL examined with PET before and after auto-HSCT were enrolled. Two patients did not undergo PET scan after HSCT. Their mean age was 40.23±12.57 years.Forty-two patients underwent upfront auto-HSCT and 42 underwent auto-HSCT after salvage treatment. The sAAIPI for DLBCL was determined (Table 1).
Kaplan-Meier analysis of PFS and OS
The 3-year PFS rate for pre-HSCT PET-negative and positive cohort was significantly different (83.8% vs.46.8%, P<0.001). The 3-year OS rate was 90.9% for pre-HSCT PET-negative cohort versus 63.4% for PET-positive cohort (P=0.003). The 3-year PFS rate in post-HSCT PET-negative cohort was higher than that in PET-positive cohort (86.0% vs. 35.3%. P<0.001). The 3-year OS rate for post-HSCT PET-negative and positive cohort was 96.7% and 36.2% (P<0.001), respectively (Figure 1).
Kaplan-Meier analysis showed that the number of previous regimens administered prior to HSCT was significantly associated with the 3-year PFS and OS.Patients who underwent upfront auto-HSCT had superior outcomes compared with relapsed/refractory DLBCL patients (3-year PFS, 97.6% vs. 51.1%, P<0.001; 3-year OS, 100% vs. 62.6%, P<0.001) (Figure 2A, B). Clinical response to chemotherapy (CR, PR, or SD+PD) before auto-HSCT was also identified as a prognostic factor for 3-year PFS (82.8%, 66.7%, 26.7%, P<0.001) and OS (91.3%,64.8%, 60.0%, P<0.001) (Figure 3A, B).
In the relapsed/refractory setting (n=42), patients with negative pre-HSCT PET had significantly superior 3-year PFS (63.0% vs. 25.7%, P=0.003) and OS (77.7% vs. 40.8%,P=0.027) compared to patients with positive pre-HSCT PET (Figure 4A, B). Similarly, the post-HSCT PET finding was also found as a statistically significant prognostic factor for 3-year PFS (67.2% vs. 23.1%,P<0.001) and OS (92.0% vs. 0%, P<0.001) (Figure 4C, D).In the upfront setting (n=42), pre- and post-HSCT PET findings were also prognostic factors for 3-year PFS (100%vs. 87.7%, P=0.025; 100% vs. 75.0%, P=0.002). However,there was no difference for patients with different pre- and post-HSCT PET results regarding 3-year OS.
In the subgroup analysis of 21 patients with positive PET scan before auto-HSCT, responders (CR+PR, n=11) had superior 3-year PFS (63.6% vs. 26.7%, P=0.084) and OS(71.6% vs. 60.0%, P=0.240) compared to non-responders(SD+PD, n=10).
Univariate and multivariate analysis of PFS and OS
Factors significantly associated with PFS or OS in univariate analysis (Table 2) were analyzed by multivariate analysis (Table 3). Post-HSCT PET finding was significantly associated with 3-year PFS [hazard ratio (HR),5.168; 95% confidence interval (95% CI), 2.055-12.999;P<0.001] and OS (HR, 26.138; 95% CI, 5.607-121.855;P<0.001), respectively. The number of previous regimens administered prior to HSCT was associated with PFS(P=0.005; HR, 18.065; 95% CI, 2.380-137.105).
Discussion
Unlike clinical prognostic scores,18F-FDG PET/CT can assess chemosensitivity, which is a significantly prognostic factor in lymphoma patients following auto-HSCT.Numerous groups have evaluated the role of pre-HSCT PET in predicting the outcomes of DLBCL patients treated with salvage chemotherapy and auto-HSCT (12-14). The prognostic value of pre-HSCT PET in DLBCL patients who underwent auto-HSCT was evaluated in a retrospective study. Pre-HSCT PET-negative patients had higher 3-year PFS and OS rates (77% and 86%,respectively) than pre-HSCT PET-positive patients (49%and 54%, respectively) (15). However, none of these studies used the Deauville criteria to interpret PET results, which have been recommended as the preferred interpretation method for interim response evaluation (11,16,17).Therefore, there is no consensus in terms of the use of the Deauville criteria in the auto-HSCT setting. The Deauville criteria were used to interpret PET results in our study.These findings are in accordance with the results from previous studies. The pre-HSCT PET was identified as a significant prognostic factor in univariate analysis in terms of 3-year PFS and OS rates. However, in the multivariate analysis, pre-HSCT PET did not provide prognostic information.
The prognostic role of post-HSCT PET was also evaluated in the present study. Univariate analysis indicated that the 3-year PFS and OS rates were significantly higher in post-HSCT PET-negative patients than in post-HSCT PET-positive patients. Multivariate analysis showed post-HSCT PET was also a prognostic factor for 3-year PFS and OS rates.
There is still no consensus regarding the role of interim PET for DLBCL in the frontline setting (18-21). If frontline or salvage treatment followed by auto-HSCT was considered as a whole, pre-HSCT PET can be taken as an interim response assessment. The importance of pre-HSCT PET could be explained in this setting. However,the present study did confirm the prognostic value of post-HSCT PET as an end-of-treatment assessment.
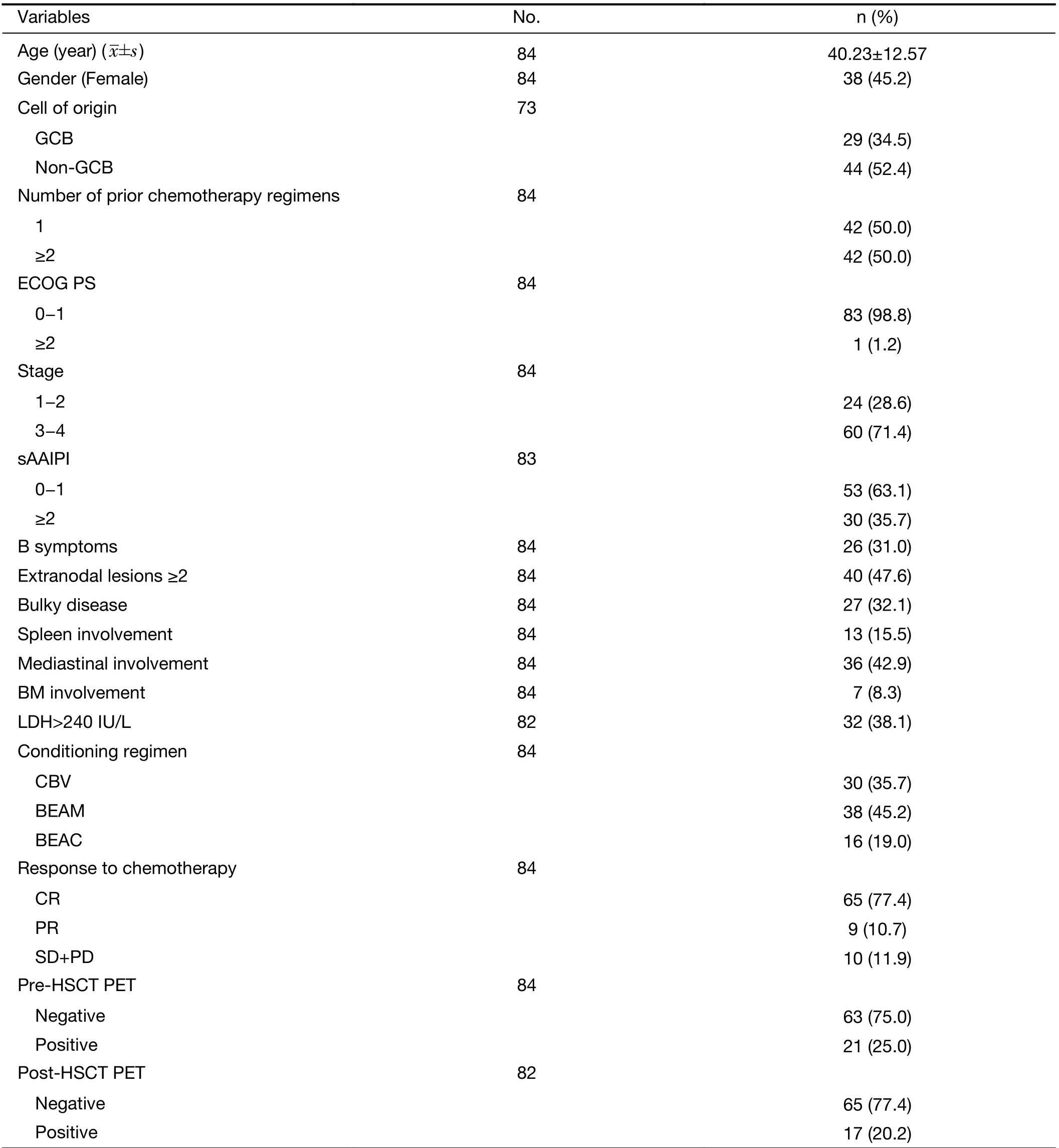
Table 1 Patients' characteristics
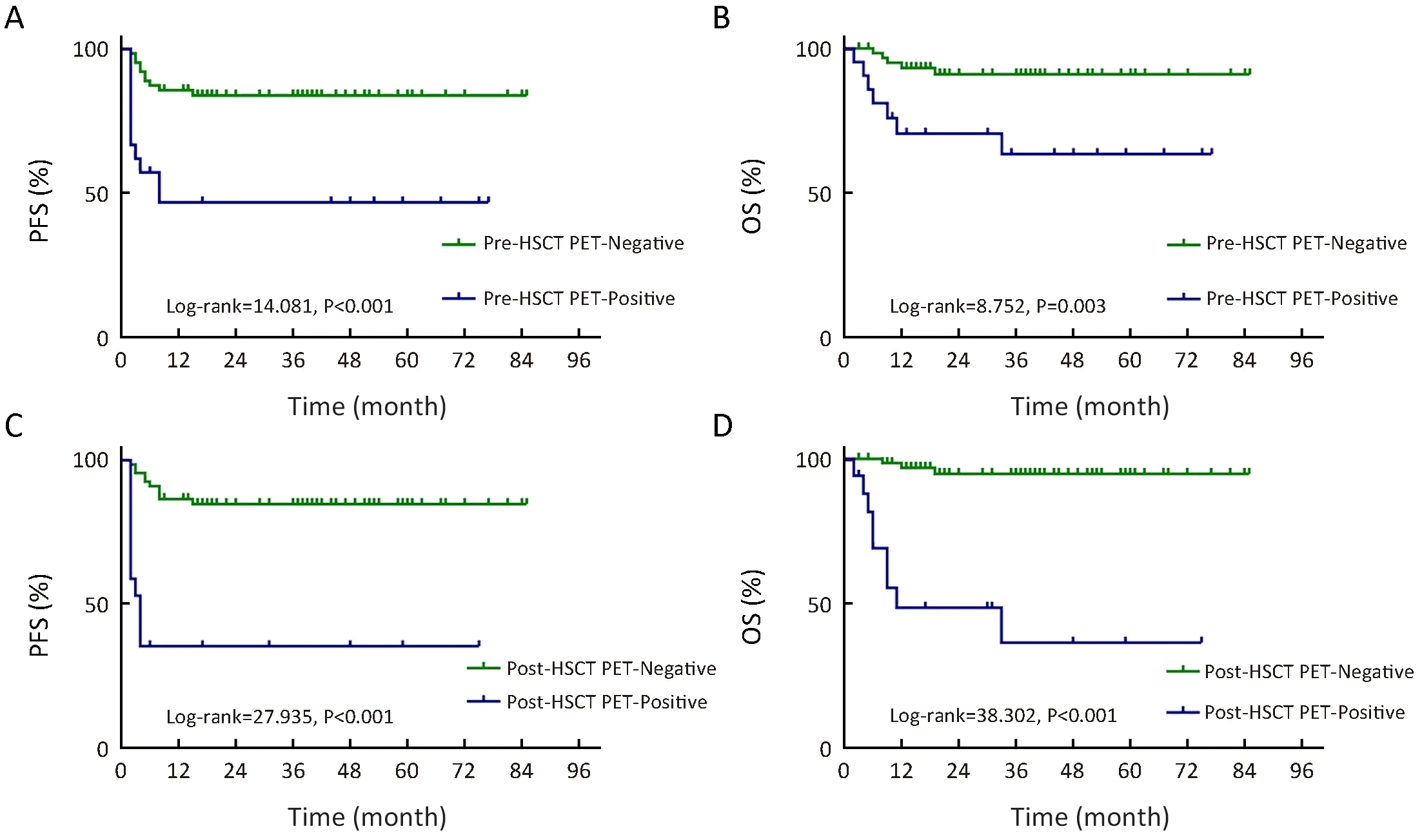
Figure 1 Kaplan-Meier analysis of progression-free survival (PFS) and overall survival (OS) for patients with pre- (A, B) and post- (C, D)autologous hematopoietic stem cell transplantation (auto-HSCT) positron emission tomography (PET) findings. (A) P<0.001; (B) P=0.003;(C) P<0.001; (D) P<0.001.
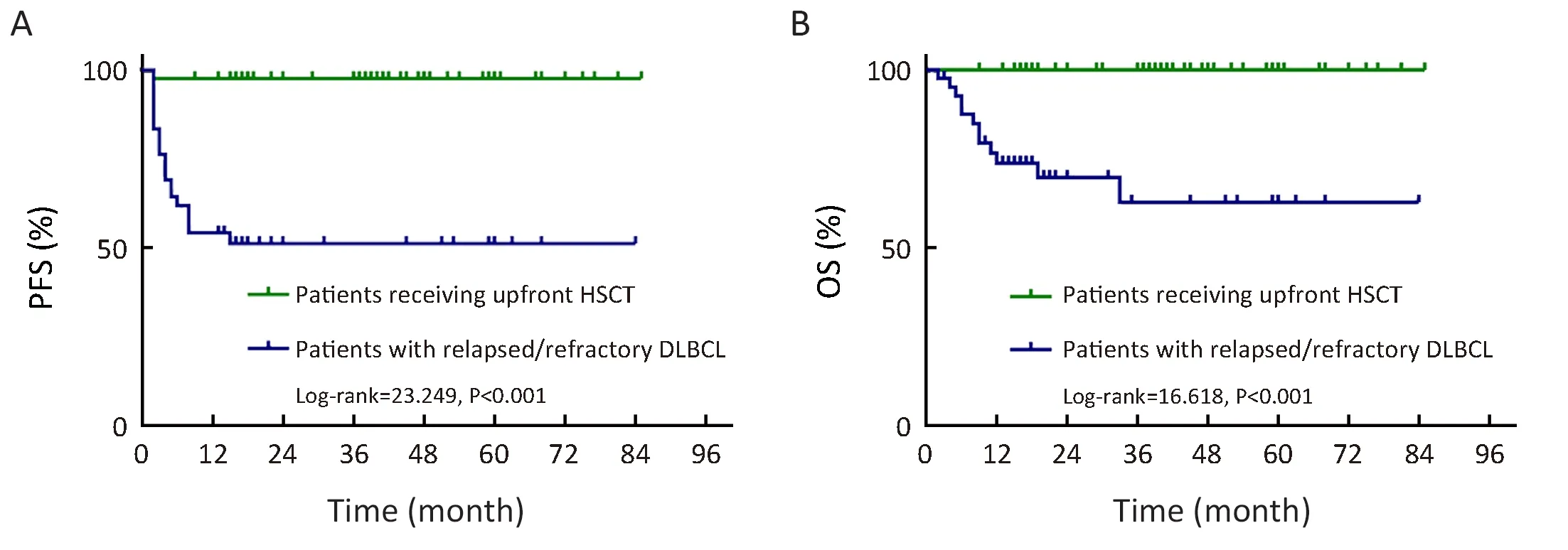
Figure 2 Kaplan-Meier analysis of progression-free survival (PFS) (A) and overall survival (OS) (B) for patients receiving upfront autologous hematopoietic stem cell transplantation (auto-HSCT) and patients with relapsed/refractory diffuse large B cell lymphoma(DLBCL). (A) P<0.001; (B) P<0.001.
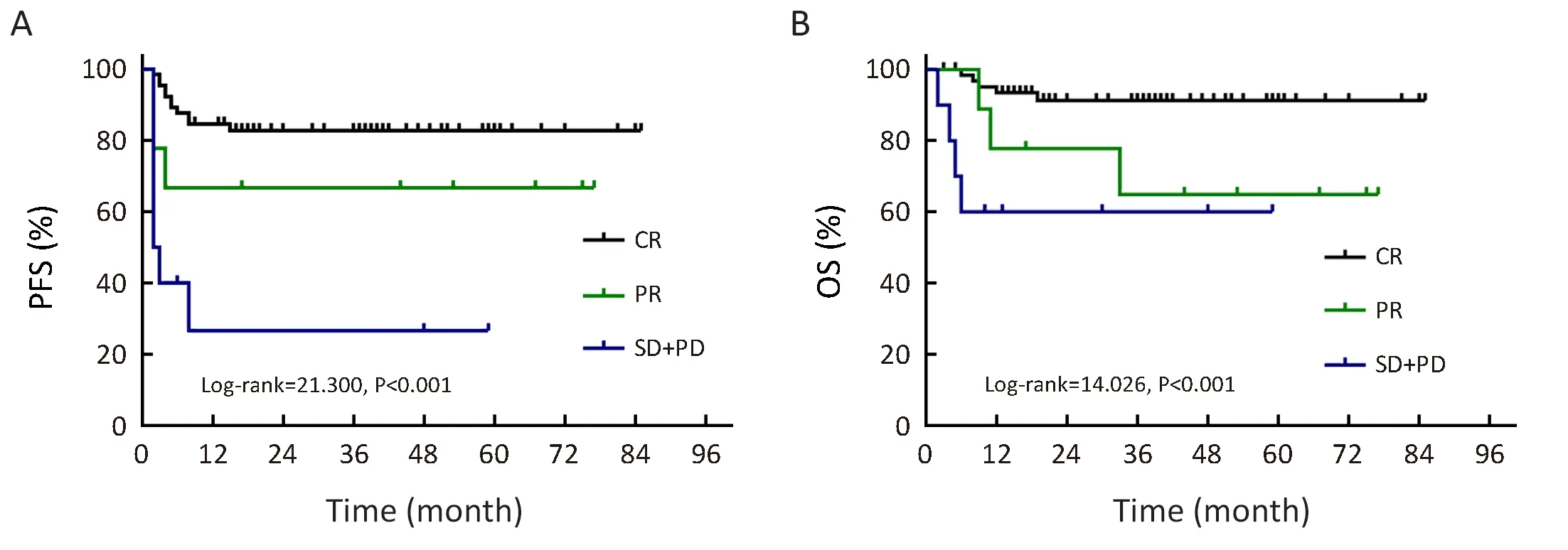
Figure 3 Kaplan-Meier analysis of progression-free survival (PFS) (A) and overall survival (OS) (B) regarding clinical response to chemotherapy. (A) P<0.001; (B) P<0.001. CR, complete response; PR, partial response; SD, stable disease; PD, progressive disease.
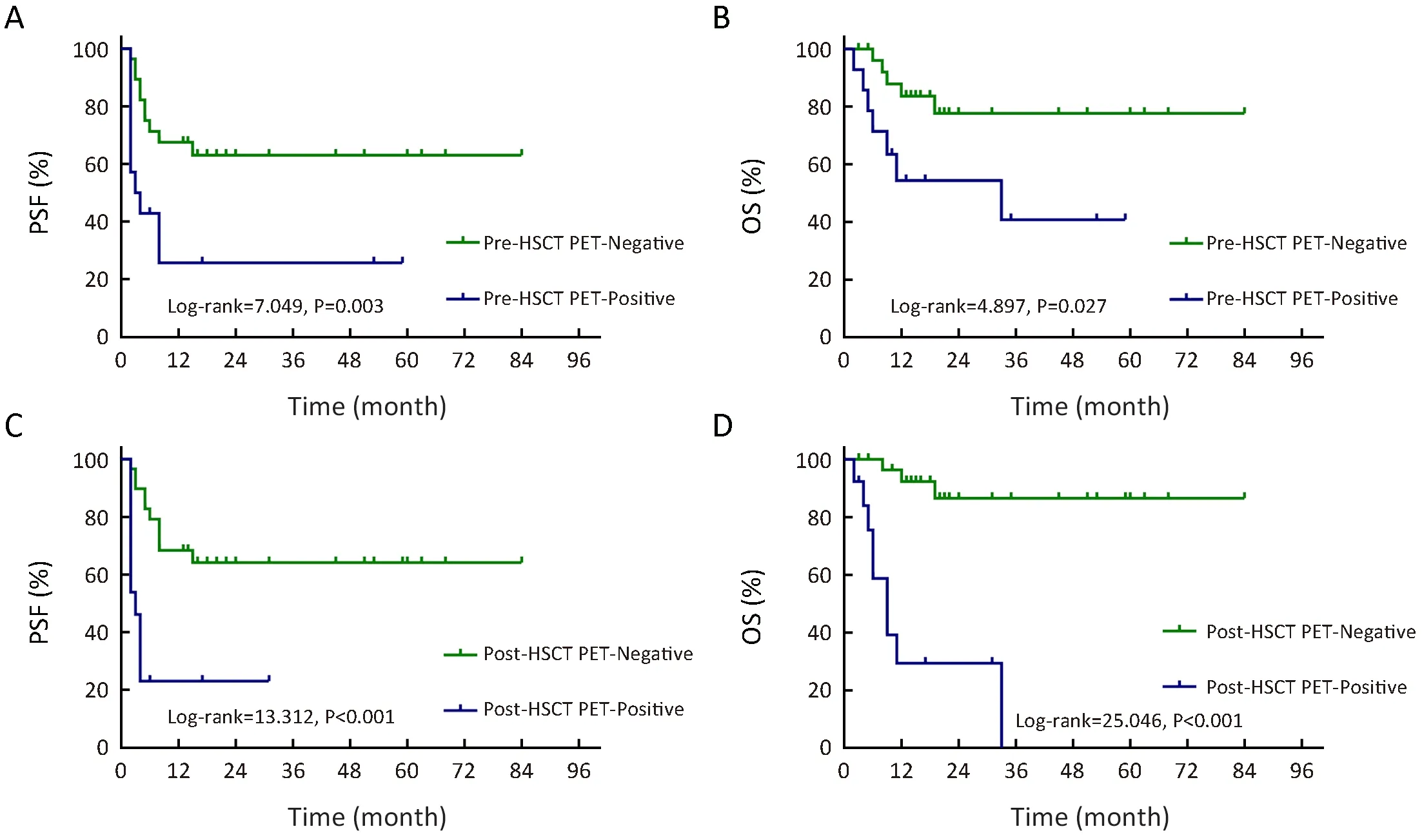
Figure 4 Kaplan-Meier analysis of progression-free survival (PFS) and overall survival (OS) for pre- (A, B) and post- (C, D) autologous hematopoietic stem cell transplantation (auto-HSCT) positron emission tomography (PET) in the relapsed/refractory setting. (A) P=0.003;(B) P=0.027; (C) P<0.001; (D) P<0.001.
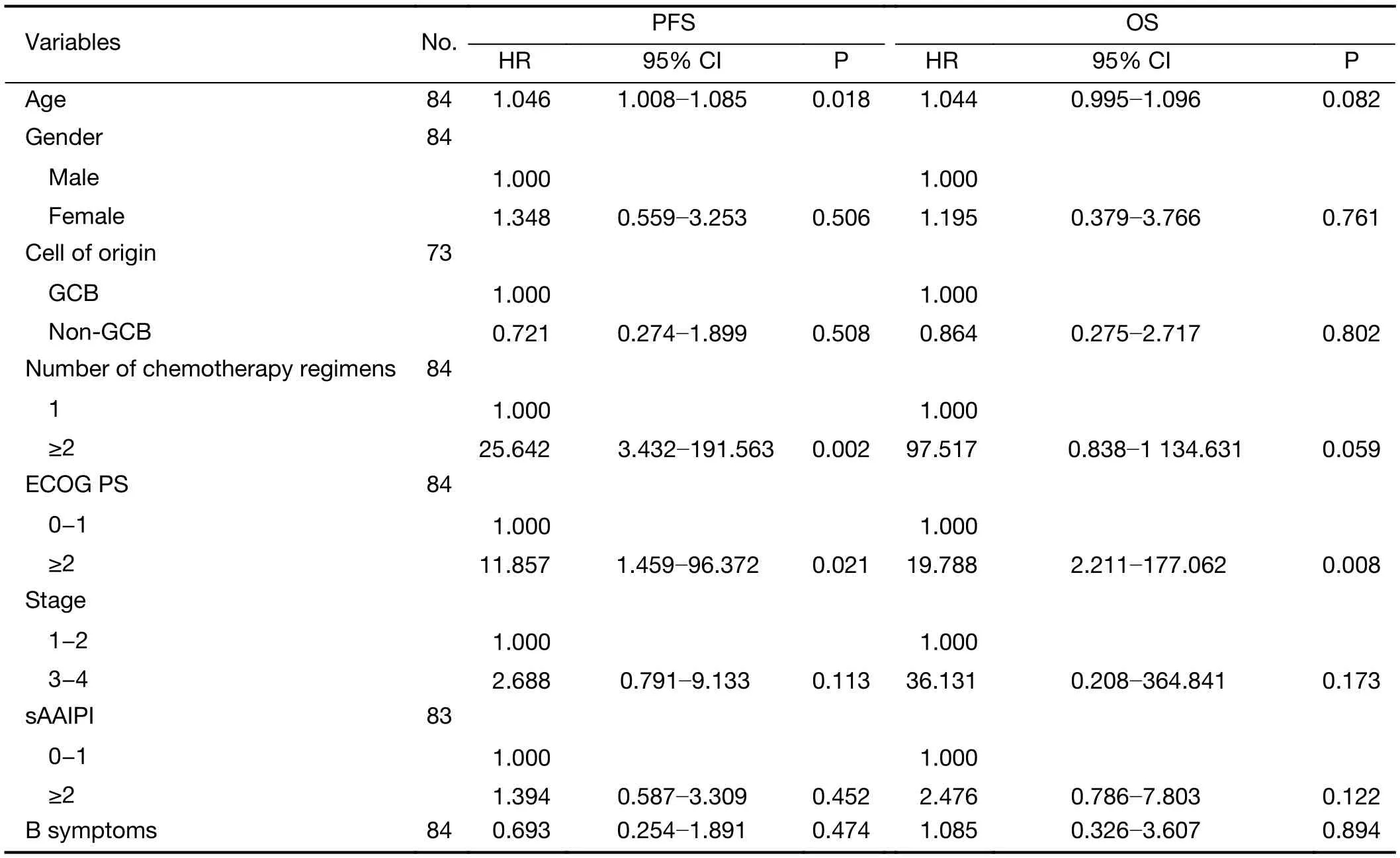
Table 2 Univariate Cox hazard analysis of risk factors for PFS and OS
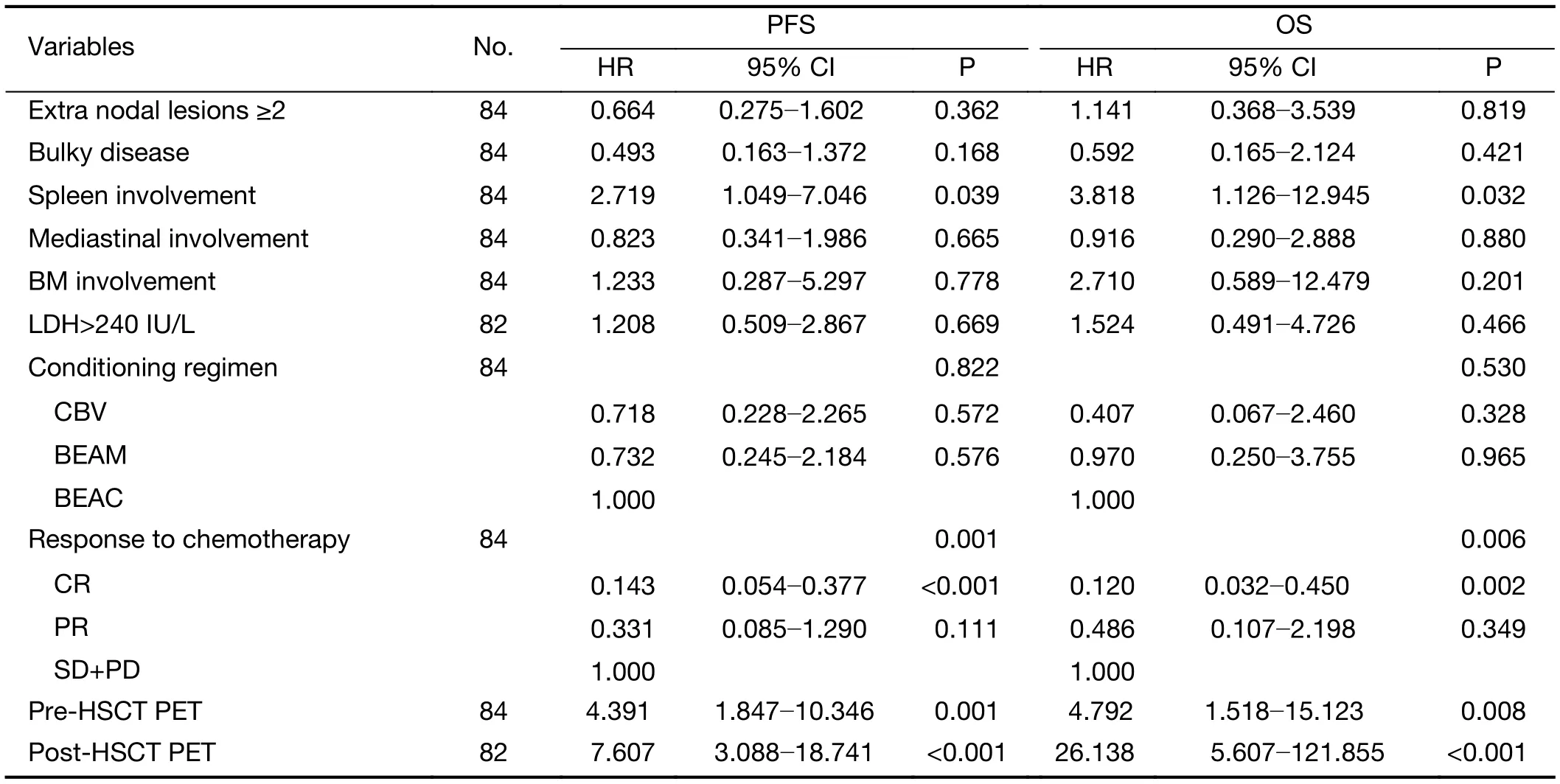
Table 2 (continued)
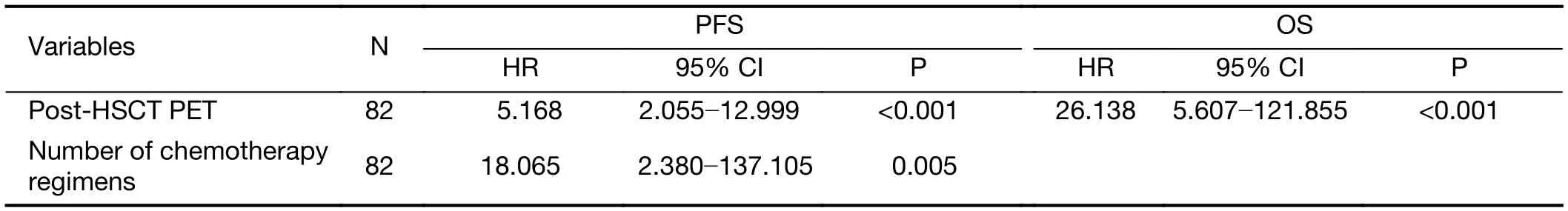
Table 3 Multivariate analysis of risks factors for PFS and OS
Univariate analysis showed that the number of prior regimens significantly affected the outcomes. Patients who received consolidative auto-HSCT after first-line treatment had superior 3-year PFS and OS rates compared to those with relapsed/refractory DLBCL. The number of prior chemotherapy regimens was found to be associated with 3-year PFS in the multivariate analysis. The role of PET scanning was also assessed in different settings.Salvage chemotherapy followed by HDC-HSCT is the standard treatment for relapsed DLBCL (5,22-24). In our study, pre- and post-HSCT PET was found to be correlated with the prognosis of relapsed/refractory DLBCL patients in terms of 3-year PFS and OS rates.However, the value of upfront auto-HSCT in DLBCL remains a matter of debate (4,25,26). Our study showed that pre- and post-HSCT PET were only associated with 3-year PFS in the upfront setting.
It has been demonstrated by a number of studies that chemosensitivity before auto-HSCT is a significant prognostic factor (4,5,22-24). We defined clinical response based on the Lugano criteria. In our study, patients who responded to chemotherapy before auto-HSCT had significantly better 3-year PFS and OS in the entire cohort and in the subgroup of patients with positive pre-HSCT PET.
Conclusions
The challenge in clinical practice is to identify the patients who can benefit from auto-HSCT. Multiple studies have reported the prognostic importance of pre-HSCT PET in DLBCL. The findings in our study are in accordance with previous results. The importance of pre-HSCT PET and clinical response before auto-HSCT was also validated in our study, especially in the relapsed/refractory setting,although post-HSCT PET provided more prognostic value in the multivariate setting. The Deauville criteria should be used to interpret PET scans in the transplantation setting.Based on the findings from our study, patients who responded to chemotherapy, even those with positive pre-HSCT PET are appropriate candidates for auto-HSCT.
Acknowledgements
This study was supported by the National Natural Science Foundation of China (No. 81600164).
Footnote
Conflicts of Interest: The authors have no conflicts of interests to declare.
 Chinese Journal of Cancer Research2019年1期
Chinese Journal of Cancer Research2019年1期
- Chinese Journal of Cancer Research的其它文章
- STIM1 expression is associated with osteosarcoma cell survival
- Prognostic implications of epidermal growth factor receptor variant III expression and nuclear translocation in Chinese human gliomas
- Risk-stratification model to select conversion surgery for advanced gastric cancer patients
- Metastatic patterns and surgical methods for lymph nodes No. 5 and No. 6 in proximal gastric cancer
- Clinical features and outcomes of diffuse large B-cell lymphoma based on nodal or extranodal primary sites of origin: Analysis of 1,085 WHO classified cases in a single institution in China
- Incidence and mortality of thyroid cancer in China, 2008-2012
