Blunt abdominal injury with rupture of giant hepatic cavernous hemangioma and laceration of the spleen
Kaohsiung, Taiwan, China
Blunt abdominal injury with rupture of giant hepatic cavernous hemangioma and laceration of the spleen
Lung-Yun Kang, Fong-Dee Huang and Yuan-Yuarn Liu
Kaohsiung, Taiwan, China
A 41-year-old woman with blunt abdominal trauma due to a motor vehicle accident presented to our emergency department. The patient had a history of a giant hepatic cavernous hemangioma. Emergency exploratory laparotomy was performed for suspected intra-abdominal bleeding with abdominal compartment syndrome, and more than 4 liters of blood and blood clots were removed. An active bleeding laceration (5 cm) of a hepatic cavernous hemangioma was detected in segment III of the liver. The bleeding was controlled by sutures, Tefon patches and tamponade. The abdomen was closed temporarily using the vacuum-assisted method. Because of the presence of persistent fresh blood through abdominal drainage at a rate of >1 L/h, splenectomy was performed to control the bleeding again by sutures and Tefon patches. Finally, the abdomen was closed using a biologic mesh. The patient was discharged home 30 days after trauma. Bleeding of trauma-caused hepatic hemangioma is rare, but splenic injury due to blunt abdominal trauma is common. An in-depth investigation is necessary to avoid second intervention.
trauma; giant hepatic cavernous hemangioma; laceration of spleen
Introduction
Hepatic hemangioma is the most frequent benign tumor of the liver.[1]Rupture of hepatic hemangioma is rare and the rate of its non-spontaneous rupture is 53% (52/98).[2,3]Giant hepatic heman-gioma (GHH) is defned to have a diameter >4 cm and likely to be symptomatic.[1]Intervention is indicated only for symptomatic or complicated hemangiomas, not for size. The management of these hemangiomas includes resection, transcatheter arterial embolization, radiation and transplantation.[4]The indications for these procedures are inability to exclude malignancy, severe symptoms, rupture with hemoperitoneum, intratumoral hemorrhage and consumptive coagulopathy (Kasabach-Merritt syndrome).[3]We reported a patient who had a GHH with multiple intra-abdominal injuries.
Clinical images
A 41-year-old woman with blunt abdominal trauma caused by a motor vehicle accident presented to our emergency department. The patient had a history of GHH manifested as abdominal distention and fullness for a long time, for which she had refused surgical resection (Fig. 1). At admission, the patient complained of abdominal distention and shortness of breath. On physical examination, her blood pressure was 60/30 mmHg, pulse rate 89 beats/minute, and respiratory rate 34 breaths/ minute. Ultrasonography showed massive fuid collection within Morison's pouch. The patient became unresponsive and required endotracheal intubation. Because of a rapid deterioration of patient's condition, computed tomography was deferred.
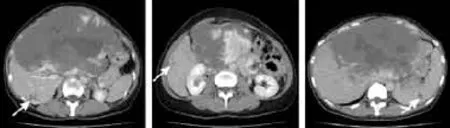
Fig. 1.Multiple hemangiomas of bilateral liver lobes and spleen, with the largest one at left lobe, measured as 20×15×10 cm in size.

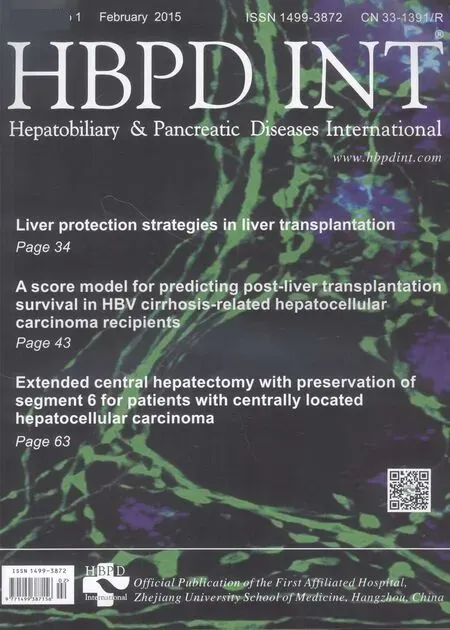
Fig. 2.Laceration of spleen, grade II.
Emergency laparotomy was performed for suspected intra-abdominal bleeding associated with abdominal compartment syndrome. During the operation, more than 4 liters of blood and blood clots were removed. An active bleeding, 5-cm, laceration of a hepatic hemangioma was detected in segment III of the liver. The bleeding was controlled by sutures, Tefon patches and tamponade. The estimated intraoperative blood loss was 8 liters. Temporary abdominal closure was achieved using a vacuum-assisted method. The patient was transferred to the intensive care unit (ICU) because of persistent shock and hypothermia. After 4-hour treatment in the ICU, the core temperature of the patient increased to >35 ℃. However, in the presence of persistent fresh blood through abdominal drainage at a rate of >1 L/h, she underwent another operation. Her blood pressure was 92/63 mmHg, pulse rate 123 beats/minute and respiratory rate 16 breaths/minute. At that time, a grade II laceration of the spleen (Fig. 2) and another laceration of the hepatic hemangioma were detected in segment II. Splenectomy was performed and the bleeding was controlled again by sutures and Tefon patches. Finally, the abdomen was closed with a biologic mesh. However, her in-hospital course was complicated by a subcutaneous hematoma which was removed later. In addition, she could not be weaned off of assisted ventilation (although 2 attempts were made) and required a percutaneous tracheostomy that resulted in infection postoperatively. Neither intra-abdominal abscess nor biloma was noted. The patient was discharged home 30 days after trauma.
Discussion
Since the mortality of rupture of GHH is high, many patients may die before any surgical intervention. In patients with spontaneous or traumatic rupture of GHH, the mortality rate is 36%-39%.[5,6]If the condition of the patient is stable, transarterial embolization prior to surgery may decrease the amount of intraoperative bleeding.[7]When resection is contraindicated for the limited amount of remaining functional hepatic tissue, transplantation may be feasible.[7,8]
Trauma patients with massive bleeding are at risk of metabolic acidosis, hypothermia and coagulopathy.[9]For these patients, fuid resuscitation, blood transfusion, coagulopathy correction, and hypothermia prevention are necessary. Damage control surgery involves sutures and tamponades to control bleeding, and resuscitation increases the survival rate of patients although the mortality remains high. A study[1]reported a mortality rate of 56% (5/9 patients). In a patient with persistent shock, complicated with traumatic injury should be considered, particularly the laceration of the spleen.
In conclusion, following an abdominal trauma, the bleeding of hepatic hemangioma is rare, but splenic injury is common. An in-depth investigation is necessary to avoid second intervention.
Contributors:LYY proposed the study. KLY performed the research and wrote the frst draft. HFD collected and analyzed the data. All authors contributed to the design and interpretation of the study and to further drafts. LYY is the guarantor.
Funding:None.
Ethical approval:Not needed.
Competing interest:No benefts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Adam YG, Huvos AG, Fortner JG. Giant hemangiomas of the liver. Ann Surg 1970;172:239-245.
2 Donati M, Stavrou GA, Donati A, Oldhafer KJ. The risk of spontaneous rupture of liver hemangiomas: a critical review of the literature. J Hepatobiliary Pancreat Sci 2011;18:797-805.
3 Beatty JS, Mitchell JW, Holsten SB, Ferdinand CH. Traumatic rupture of a previously undiagnosed giant hepatic hemangioma. Am Surg 2013;79:e314-315.
4 Farges O, Daradkeh S, Bismuth H. Cavernous hemangiomas of the liver: are there any indications for resection? World J Surg 1995;19:19-24.
5 Corigliano N, Mercantini P, Amodio PM, Balducci G, Caterino S, Ramacciato G, et al. Hemoperitoneum from a spontaneous rupture of a giant hemangioma of the liver: report of a case. Surg Today 2003;33:459-463.
6 Hoekstra LT, Bieze M, Erdogan D, Roelofs JJ, Beuers UH, van Gulik TM. Management of giant liver hemangiomas: an update. Expert Rev Gastroenterol Hepatol 2013;7:263-268.
7 Vagef PA, Klein I, Gelb B, Hameed B, Moff SL, Simko JP, et al. Emergent orthotopic liver transplantation for hemorrhage from a giant cavernous hepatic hemangioma: case report and review. J Gastrointest Surg 2011;15:209-214.
8 Kumashiro Y, Kasahara M, Nomoto K, Kawai M, Sasaki K, Kiuchi T, et al. Living donor liver transplantation for giant hepatic hemangioma with Kasabach-Merritt syndrome with a posterior segment graft. Liver Transpl 2002;8:721-724.
9 Cirocchi R, Montedori A, Farinella E, Bonacini I, Tagliabue L, Abraha I. Damage control surgery for abdominal trauma. Cochrane Database Syst Rev 2013;3:CD007438.
Received April 1, 2014
Accepted after revision July 31, 2014
(Hepatobiliary Pancreat Dis Int 2015;14:109-110)
AuthorAffliations:Department of Emergency Medicine, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan, China (Kang LY, Huang FD and Liu YY)
Yuan-Yuarn Liu, MD, Department of Emergency Medicine, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan, China (Tel: +886-7-3422121ext8342; Fax: +886-7-3455064; Email: conroy0615@ yahoo.com.tw)
? 2015, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(14)60310-6
Published online November 14, 2014.
 Hepatobiliary & Pancreatic Diseases International2015年1期
Hepatobiliary & Pancreatic Diseases International2015年1期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Meetings and Courses
- Enlarged pancreas: not always a cancer
- p38 MAPK inhibition alleviates experimental acute pancreatitis in mice
- Predictors of incidental gallbladder cancer in elderly patients
- Liver, biliary and pancreatic injuries in pancreaticobiliary maljunction model in cats
- Development of hybrid-type modifed chitosan derivative nanoparticles for the intracellular delivery of midkine-siRNA in hepatocellular carcinoma cells
