Blood Lead Levels During Pregnancy and Its Influencing Factors in Nanjing,China
Kang-sheng Liu,Jia-hu Hao,Juan Shi,Chun-fang Dai,and Xi-rong Guo*
1State Key Laboratory of Reproductive Medicine,Department of Clinical Laboratory,Nanjing Maternity and Child Health Care Hospital Affiliated to Nanjing Medical University,Nanjing 210029,China
2 Department of Maternity Child Health Care,School of Public Health,Anhui Medical University,Hefei 230032,China
3Child Health Care Department,4Department of Obstetrics,5Director’s Office,Nanjing Maternity and Child Health Care Hospital,Nanjing 210004,China
LEAD is a cumulative toxicant that adversely affects various organs and systems of human body.It can readily transfer into the fetus through the placenta,1and in the absence of efficient placental barrier,the fetus could be exposed to lead at a concentration very close to that in the mother’s body.Fetal vulnerability may occur even if the mother’s exposure had ceased many years earlier.2,3Lead interferes with signal transmission at the synapse and cellular adhesion molecules,causing disruption in cell migration during critical times in the nervous system development.4Other adverse effects related to prenatal lead exposure include reproductive effects,conduct disorder in children,cardiovascular functioning,and genomic methylation of DNA.5-8Prenatal lead exposure forms a plumbeous environment for the fetus and newborns and may affect the fetus in a number of detrimental ways.9,10Elevated blood lead level (BLL) during pregnancy are associated with an increased risk of preterm births,spontaneous abortion,and other anomalies.11-13Therefore,it is particularly important to reduce lead exposure in pregnant women for aristogenesis.
The BLL and the susceptibility to lead toxicity of pregnant women can be influenced by many factors such as environmental exposure,life styles,diet habits,and nutritional status.14The living standards of pregnant women may vary largely along with geographical locations and uneven economic development.Similarly,lead exposure and the influencing factors may also differ greatly among women living in different areas and even among those in the same area but with different economic status.It is therefore essential to monitor the BLL and the influencing factors across or within different areas.China has been challenged with severe lead pollution.15A previous research has found that the BLL in children in Chengdu,a city in southwest China,is different from the levels in other areas.16To assess the level of lead poisoning in children in a given area,American Center for Disease Control divided the prevalence into three groups∶(1) higher than 12% as high epidemic area;(2) 6%-12% as moderate epidemic area;(3) lower than 5.9% as low epidemic area.Chengdu is a moderate epidemic according to the criterion.16To identify the BLL in pregnant women and its change during the whole gestation,we designed this prospective,longitudinal study,and investigated the influencing factors of BLL in pregnant women living in Nanjing at their early pregnancy (10-14 weeks) with a questionnaire.
MATERIALS AND METHODS
Study subjects recruitment
Pregnant women were recruited from September 2009 to February 2010 atNanjing Maternity and Child Health Care Hospital prenatal clinic.Of the 288 women assessed for eligibility,18 did not meet the study criteria (at 10-14th gestation weeks;singleton pregnancy;well-developed fetus shown by ultrasonic examination).Of the remaining 270 eligible women,250 (92.6%) agreed to participate in the study.
Then we excluded 31 women based on the following exclusion criteria∶(1) body mass index (BMI) >30 kg/m2or<18 kg/m2;(2) having a history of malignant tumor,systemic lupus erythematosus,diabetes mellitus,hypertension,pancreatitis,liver disease,kidney disease,or disease of the hematologic or metabolic system;(3) not living in Nanjing.A total of 219 blood specimens and questionnaires were obtained at early pregnancy of the included women.They were followed up at mid-pregnancy (20-24 weeks),late pregnancy (30-34 weeks),and 6-12 weeks after delivery.Seventeen participants withdrew due to abortion (n=6),transferred to another hospital (n=10),or withdrew voluntarily (n=1).After the 3-stage follow-up,we excluded the women who had obstetric complications or fetal abnormality and another 28 participants were excluded∶20 for obstetric complications,3 for premature delivery,2 for prolonged pregnancy,1 for low birth weight,and 2 withdrew voluntarily.Finally 174 healthy pregnant women were included in the gravida group.Figure 1 outlines the screening process.
As controls,120 healthy non-pregnant women were included after matching for age,BMI,and residence area.The women in the control group did not take any nutrients supplements.We also excluded those who were actresses or performers because they tended to use more cosmetics than those in other occupations.The study was carried out according to the principles of the Declaration of Helsinki.All the participants received a detailed explanation of the study objective,research procedure,and information on how to reduce environmental lead exposure.
Data collection
A screening questionnaire was employed to gather socioeconomic and demographic information,medical and reproductive histories,influencing factors for lead exposure of the women in the gravida group during pregnancy at first trimester.Those factors included occupations (such as painting workers,traffic policewomen,workers in irons,steel,and lead production,soldering,or smeltery,radiator repairwomen,battery manufacturers,welders of old painted metals,barbers,etc.),lifestyle(active/passive smoking,drinking),hair dyeing,cosmetics use,floor level of residence,time of house/apartment painted,distance from residence to street,kitchen fuel,distance from a factory,existence of wall paint desquamating,and time of staying in the street.The dietary information focused on consumption of canned food,preserved eggs,milk,and Chinese herbal medicine.We also queried whether the pregnant women took Fe,Zn,or Ca supplements during gestation.Fasting blood samples were obtained from the antecubital vein in each pregnancy trimester and at the same period from the non-pregnant controls after a 30-minute rest in a sitting position.These blood samples were drawn into vacuum tubes (Becton-Dickinson,Franklin Lakes,NJ,USA) containing heparin lithium and sent to detect blood lead concentration by flame atomic absorption spectroscopy (BH-2100 atomic absorption spectrometer,Bo Hui Company,Beijing,China)within 1 hour.Internal quality controls were taken both before and after the detection.
Statistical analysis
Data analysis was performed using SPSS version 13.0(SPSS,Chicago,IL,USA).The BLLs were presented as means±SD as Kolmogorov-Smirnov test showed normal distributions (P>0.05).The least significant differencettest of analysis of variance was used for the three trimesters and the postpartum in the gravida and the control group.The logistic regression was used for analyzing the possible influencing factors of BLLs at early pregnancy.P<0.05 was considered statistically significant.
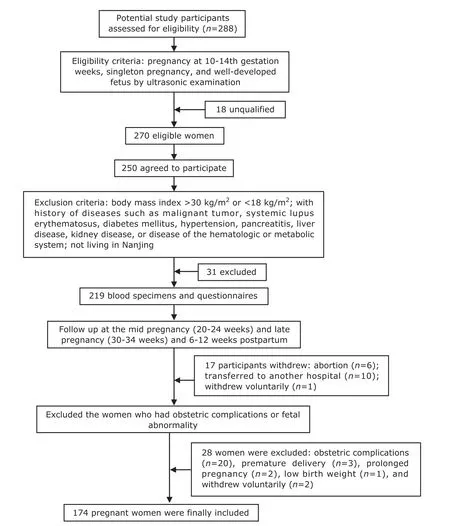
Figure 1.The flowchart of the screening of healthy pregnant women (gravida group)
RESULTS
The age of the recruited pregnant women ranged from 20 to 41 years with a mean age of 29±3 years.There was no statistical difference between the gravida group and the control group in age,race,educational level,economic status,and living condition.The BLLs in all the pregnant women in the first trimester ranged from 17.4 to 120.0 μg/L,and in the control group ranged from 20.0 to 110.0 μg/L,there were 4 in the gravida group in the first trimester and 4 in the control group whose BLLs were greater than 100 μg/L (Table 1).The mean lead concentrations in three trimesters in the gravida group were 59.8±24.3,55.4±20.1,and 55.9±19.7 μg/ L,respectively,but rose to 67.6±17.4 μg/L in 6-12 weeks after delivery.The lead concentration of the control group was 67.5±21.3 μg/L.
The BLLs in all the three trimesters were lower than those in the control group (P=0.043,0.021,and 0.028),but no statistical significance was found between each two trimesters (F=9.55,8.74,8.89;P>0.05).After delivery,the BLLs of the pregnant women returned to the level in the control group.Logistic regression showed that age,active/passive smoking,hair dyeing,floor level of residence,distance from residence to street,kitchen fuel,distance from a factory,existence of wall paint desquamating,time of staying in street,consumption of canned food and preserved eggs,and use of Chinese herbal medicine had no correlations with BLLs in pregnant women (P>0.05,Table 2).The related occupations (including painting workers,traffic policewomen,radiator repairwomen,welders of old painted metals,barbers),of living in a house/apartment painted less than 1 year before,and cosmetics use were shown as risk factors of high BLLs in pregnant women,while consuming milk and Fe,Zn,or Ca supplements were protective factors (Table 3).
DISCUSSION
The possibility of intra-uterine lead exposure began to be addressed in the late 1970s.Correlations between maternal and umbilical cord BLLs confirmed the transfer of lead from the mother to the fetus.17Elevated BLLs during pregnancy were also mentioned by Lagerkvist et al,18while some other researchers found that BLLs dropped during pregnancy.19Another study demonstrated a clear U-shaped curve of BLLs during pregnancy,with the lowest concentration at 20th gestation week.20The difference in BLLs in the duration of pregnancy may depend on various factors such as the time of sampling (different periods ofpregnancy),the method of sampling (venous blood or finger blood),maternal factors (parity and maternal lead burden),as well as environmental factors (place of residence,exposure level,and exposure duration).Several other factors (methods of analysis,contamination of the samples) might also interfere with the final results.21In comparison to previous studies,the present study detected lower BLLs in different periods of pregnancy.In this study,BLLs in all the three trimesters in the gravida group were lower than that in the healthy control group and then returned to the control group level in 6-12 weeks after delivery.Because the concentration of red blood cells may decrease during pregnancy due to the increase of plasma volume,and the majority of blood lead is bound to red blood cells,a lower BLL is expected during pregnancy.15That may be a possible explanation for the abovementioned finding.Another influencing factor of BLLs in the present study was the interventions to evacuate lead from women who had high BLLs before conception.
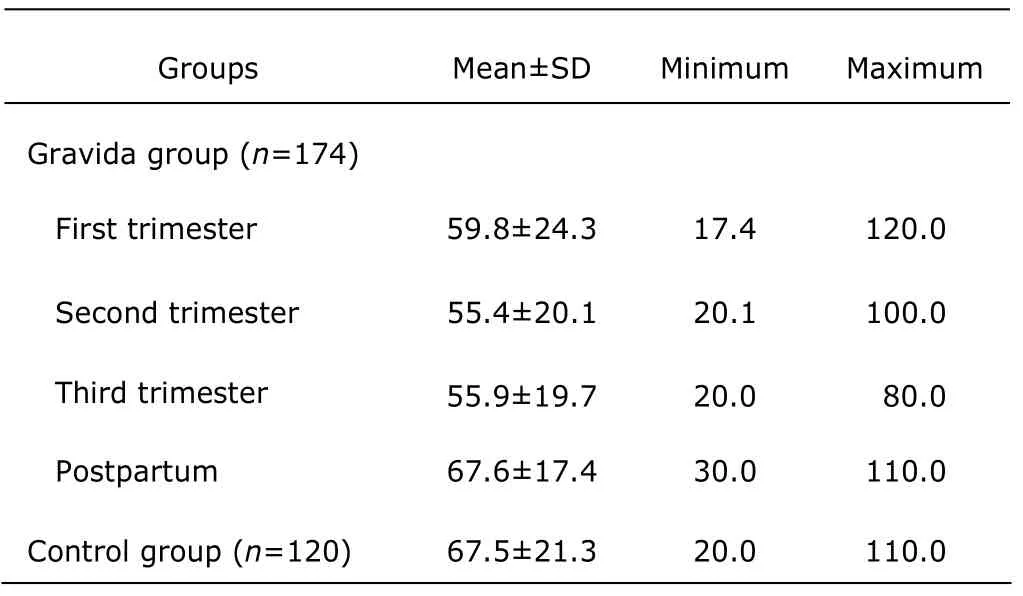
Table 1.Blood lead levels (BLLs) in 3 trimesters and postpartum 6-12 weeks of the gravida group and the control group (μg/L)
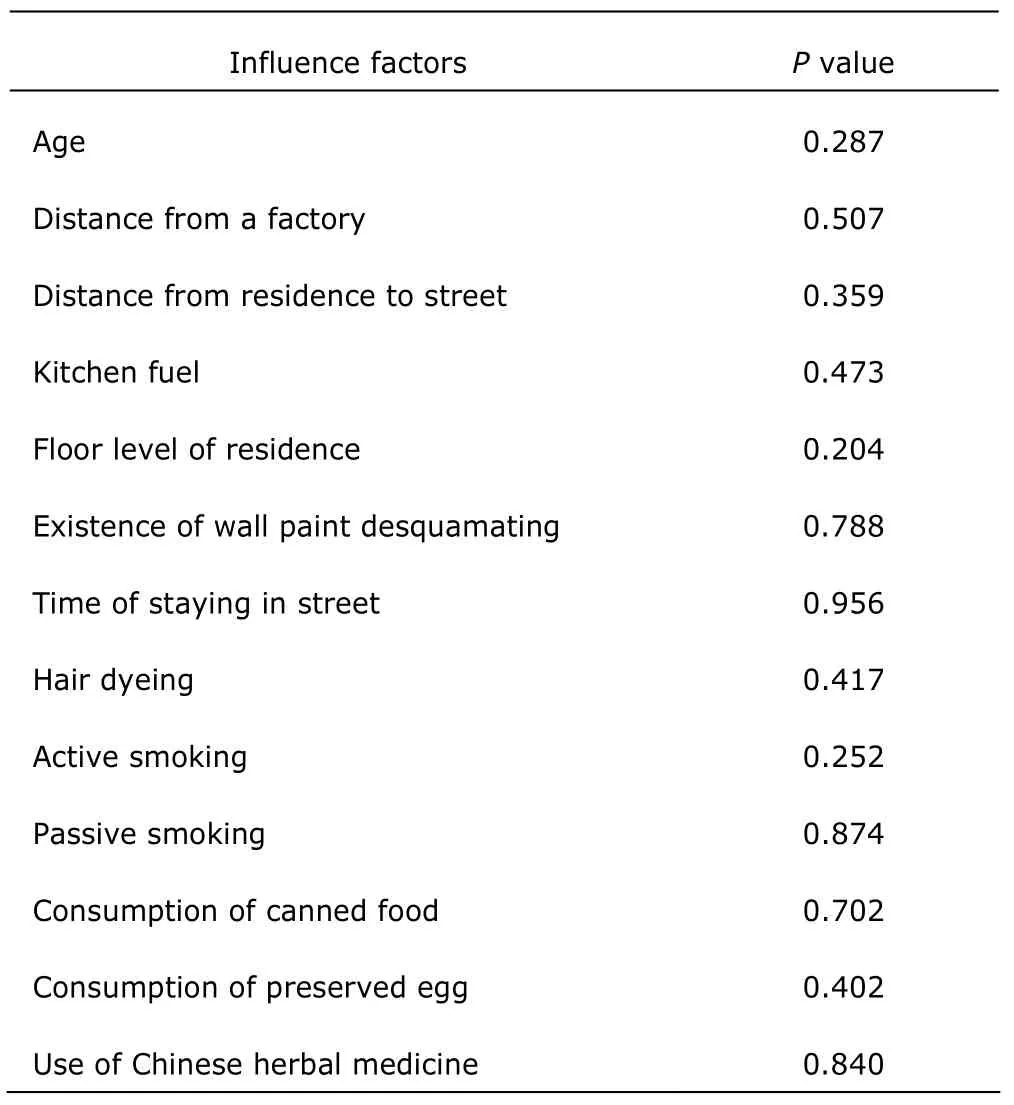
Table 2.Factors which have no correlations with BLLs in pregnant women
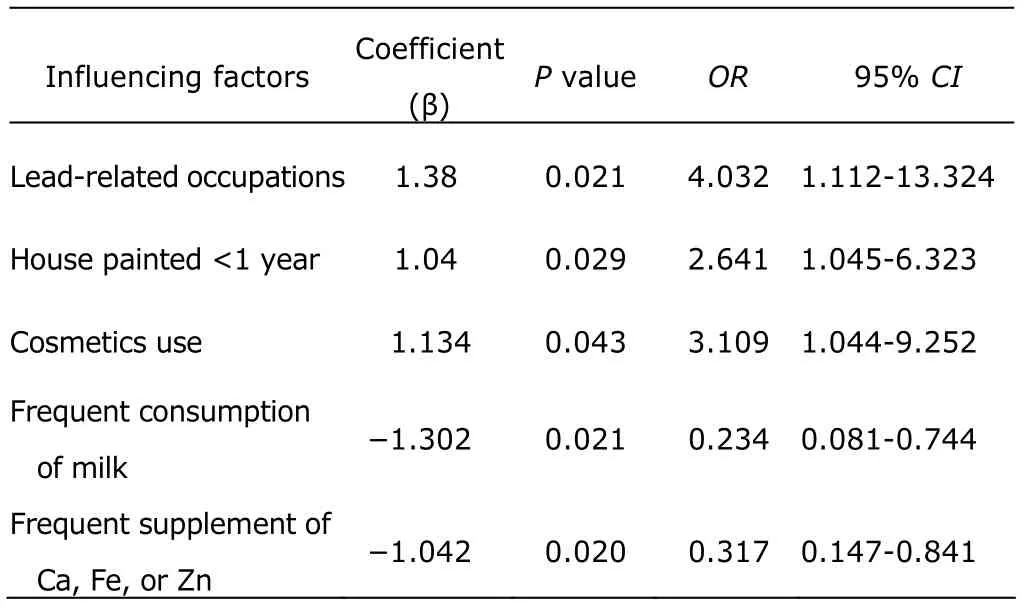
Table 3.Influencing factors correlated with BLLs in pregnant women
Currently,the most common sources of lead exposure in the US are lead-based paint,contaminated soil,household dust,drinking water,lead crystal,and lead-glazed pottery.Historically,lead intake into the gastrointestinal tract was mostly from food and drinking water,into the lung through breathing,and into cutis or mucous membranesviacontact.22Canned food may be polluted during processing and storage,thus being a source of lead exposure.23Many traditional Chinese herbal medicines have been found to contain considerable amounts of heavy metals and studies showed that lead poisoning is associated with the application of Chinese herbal medicine.24,25However,in the present study,we found that women who took canned foods and Chinese herbal medicine had indiscriminate BLLs compared with those did not.It was possible that in a few pregnant women in this study,consumption of canned foods and Chinese herbal medicine had little influence on their BLLs.Drinking water is a more common source of lead exposure.Lead leaches out from plumbing systems which contain lead pipes or lead solders,making the lead level higher in the tap water.The corrosiveness of the water,the quantity and surface area of the lead materials,the age of the lead components,and the temperature of the water also affect lead levels.23,26Since all of the participants of this study were from urban area of Nanjing,where water was supplied through the same pipeline system,we did not consider water as an influencing factors for BLLs.
Lead may interact with various nutrients including calcium,iron,and zinc.Supplements of these nutrients could reduce the absorption of lead and release of it from maternal bones.27,28Milk contains abundant nutrients(proteins,calcium,iron) that could reduce lead absorption or facilitate lead excretion.29This may partly explain our finding that the women who regularly took calcium,iron,and zinc supplements or milk had lower BLLs.Leaded gasoline accounted for most of the airborne lead pollution in large cities.30Dust and soil are the final resting place for airborne lead from gasoline.Since the ban on leaded gasoline in 2000 in China,the influence of automobile exhaust on BLLs has been diminished,which may account for the result that the distance of residence from street was not correlated with BLLs in this study.The occupations related to metal processing are another source of lead pollution.14,31The present study also found that the women who were occupied with lead-related work had higher BLLs.
However,we found that distance from a factory (such as battery factory,iron and steel factory) had no correlation with BLLs in pregnant women.This may be interpreted that since many factories (such as iron and steel factory) had been removed to suburbs,most of our study subjects were not living near a factory.
In the present study,BLLs in the pregnant women who lived in a house/apartment painted less than 1 year before were higher,which may be due to the lead-containing paints and other decoration materials.Although using leaded paint in residential decoration was banned,no intervention has been made so far to remove existing lead-based paint from apartments constructed before this edict went into effect.31The older the building is,the more leaded paint desquamating and plumbeous particulates there will be,hence the more harm to health.14Nevertheless,this study detected no correlation between wall paint desquamating and BLLs,which may be because of the small number of pregnant women living in apartments having wall paint desquamating.Cosmetics are another common source of lead in daily life.This study found that the pregnant women who usually wore cosmetics had higher BLLs.
In conclusion,the present study demonstrated that BLLs in all the three trimesters in pregnant women were lower than that in non-pregnant controls,which returned to the level of control group in 6-12 weeks after delivery.Lead-related occupations,cosmetics use,and living in a house/apartment painted less than 1 year are risk factors,while calcium,iron,zinc supplementation,and milk consumption are protective factors for BLLs in pregnant women.Those influencing factors could be useful for enacting measures to reduce lead exposure for pregnant women.BLLs in pregnant women should be monitored.Health care organizations and government bodies should carry out a series of measures to reduce lead exposure,including encouraging healthy diet and living habits in women of child-bearing age,educating people about lead poison,and maintaining a better environment.
ACKNOWLEDGEMENTS
This study was supported by Nanjing Maternity and Child Health Care Hospital.The authors are grateful to the women who volunteered to participate in this study.
1.Rossipal E,Krachler M,Li F,et al.Investigation of the transport of trace elements across barriers in humans∶studies of placental and mammary transfer.Acta Paedriatr 2000;89∶1190-5.
2.Bellinger DC.Teratogen update∶lead and pregnancy.Birth Defects Res A Clin Mol Teratol 2005;73∶409-20.
3.Hu H,Téllez-Rojo MM,Bellinger D.Fetal lead exposure at each stage of pregnancy as a predictor of infant mental development.Environ Health Perspect 2006;114∶1730-5.
4.Jones A.Emerging aspects of assessing lead poisoning in childhood.Emerg Health Threats J 2009;2∶e3.
5.Chen PC,Pan IJ,Wang JD.Parental exposure to lead and small for gestational age births.Am J Ind Med 2006;49∶417-22.
6.Braun JM,Froehlich TE,Daniels JL,et al.Association of environmental toxicants and conduct disorder in U.S.children∶NHANES 2001-2004.Environ Health Perspect 2008;116∶956-62.
7.Gump BB.Stewart P,Reihman J,et al.Prenatal and early childhood blood lead levels and cardiovascular functioning in 9(1/2) year old children.Neurotoxicol Teratol 2005;27∶655-65.
8.Herman DS,Geraldine M,Venkatesh T.Evaluation,diagnosis,and treatment of lead poisoning in a patient with occupational lead exposure∶a case presentation.J Occup Med Toxicol 2007;2∶7.
9.Goyer RA.Transplacental transport of lead.Environ Health Perspect 1990;89∶101-5.
10.Wan BJ,Zhang Y,Tian CY,et al.Blood lead dynamics of lead-exposed pregnant women and its effects on fetus development.Biomed Environ Sci 1996;9∶41-5.
11.Hertz-Picciotto I.The evidence that lead increases the risk for spontaneous abortion.Am J Ind Med 2000;38∶300-9.
12.Borja-Aburto VH,Hertz-Picciotto I,Rojas Lopez M,et al.Blood lead levels measured prospectively and risk of spontaneous abortion.Am J Epidemiol 1999;150∶590-7.
13.Gardella C.Lead exposure in pregnancy∶a review of the literature and argument for routine prenatal screening.Obstet Gynecol Surv 2001;56∶231-8.
14.White LD,Cory-Slechta DA,Gilbert ME,et al.New and evolving concepts in the neurotoxicology of lead.Toxicol Appl Pharmacol 2007;225∶1-27.
15.Wang S,Zhang J.Blood lead levels in children,China.Environ Res 2006;101∶412-8.
16.Jiang YM,Shi H,Li JY,et al.Environmental lead exposure among children in Chengdu,China∶blood lead levels and major sources.Bull Environ Contam Toxicol 2010;84∶1-4.
17.Shih RA,Hu H,Weisskopf MG,et al.Cumulative lead dose and cognitive function in adults∶a review of studies that measured both blood lead and bone lead.Environ Health Perspect 2007;115∶483-92.
18.Lagerkvist BJ,Ekesrydh S,Englyst V,et al.Increased blood lead and decreased calcium levels during pregnancy∶a prospective study of Swedish women living near a smelter.Am J Public Health 1996;86∶1247-52.
19.Moura M,Gon?alves Valente J.Blood lead levels during pregnancy in women living in Rio de Janeiro,Brazil.Sci Total Environ 2002;299∶123-9.
20.Hertz-Picciotto I,Schramm M,Watt-Morse M,et al.Patterns and determinants of blood lead during pregnancy.Am J Epidemiol 2000;152∶829-37.
21.Ettinger AS,Téllez-Rojo MM,Amarasiriwardena C,et al.Levels of lead in breast milk and their relation to maternal blood and bone lead levels at one month postpartum.Environ Health Perspect 2004;112∶926-31.
22.Markowitz M.Lead poisoning.Pediatr Rev 2000;21∶327-35.
23.Hackley B,Katz-Jacobson A.Lead poisoning in pregnancy∶a case study with implications for midwives.J Midwifery Womens Health 2003;48∶30-8.
24.Karri SK,Saper RB,Kales SN.Lead encephalopathy due to traditional medicines.Curr Drug Saf 2008;3∶54-9.
25.Ko RJ.A U.S.perspective on the adverse reactions from traditional Chinese medicines.J Chin Med Assoc 2004;67∶109-16.
26.Philip AT,Gerson B.Lead poisoning-Part 1.Incidence,etiology,and toxicokinetics.Clin Lab Med 1994;14∶423-44.
27.Johnson MA.High calcium intake blunts pregnancy induced increases in maternal blood lead.Nutr Rev 2001;59∶152-6.
28.Zimmermann MB,Muthayya S,Moretti D,et al.Iron fortification reduces blood lead levels in children in Bangalore.Indian Pediatr 2006;117∶2014-21.
29.Rothenberg SJ,Khan F,Manalo M,et al.Maternal bone lead contribution to blood lead during and after pregnancy.Environ Res 2000;82∶81-90.
30.Meyer PA,Brown MJ,Falk H.Global approach to reducing lead exposure and poisoning.Mutat Res 2008;659∶166-75.
31.Lidsky TI,Schneider JS.Lead neurotoxicity in children∶basic mechanisms and clinical correlates.Brain 2003;126∶5-19.
 Chinese Medical Sciences Journal2013年2期
Chinese Medical Sciences Journal2013年2期
- Chinese Medical Sciences Journal的其它文章
- Unsuspected Gallbladder Cancer During or After Laparoscopic Cholecystectomy
- Ureteral Stent Fragmentation:a Case Report andReview of Literature
- Physiological Testosterone Retards Cardiomyocyte Aging in Tfm Mice via Androgen Receptor-independent Pathway△
- Introduction of Management of Prostate Cancer:a Multidisciplinary Approach
- Chinese Herbal Medicine in Treatment of Polyhydramnios: a Meta-analysis and Systematic Review△
- Open Surgical Insertion of Tenkchoff Straight Catheter Without Guide Wire
