Acupuncture-moxibustion Theories of Wang Shu-he
Le Yi-min, Chen Yong,, Yang Zong-bao, Wei jia
1 Jiangxi University of Traditional Chinese Medicine, Nanchang 330004, China
2 Fuda Cancer Hospital, Guangzhou 550030, China
Acupuncture-moxibustion Theories of Wang Shu-he
Le Yi-min1, Chen Yong1,2, Yang Zong-bao1, Wei jia1
1 Jiangxi University of Traditional Chinese Medicine, Nanchang 330004, China
2 Fuda Cancer Hospital, Guangzhou 550030, China
Acupuncture-Moxibustion Theories; Literature Research; Points, Five transport-Shu; Points, Back-Shu; Points, Front-Mu; Diagnosis (Traditional Chinese medicine);Mai Jing
1 Life Story
Wang Shu-he, or Wang Xi, was an outstanding physician from Gaoping (Gaoping of Shanxi Province; another saying is Ji’ning of Shandong Province) of Western Jin Dynasty who lived around the 3rd century. His major contribution was the 10 volumes ofMai Jing(Pulse Classic), which has further systemized sphygmological theories and methods. AlthoughMai Jing(Fig.1) is known as a monographic book of sphygmology, it also records many acupuncture-moxibustion opinions. We are now summarizing its acupuncture-moxibustion theories as follows.
2 Academic Theories of Acupuncture-moxibustion Therapy
2.1 Exterior-interior connections of Zang-fu organs and three jiao (triple energizer)
Mai Jingconnects Zang-fu organs, meridians, yin-yang, and exterior-interior aspects via three jiao, revealing that the exteriorly-interiorly related meridians meet at three jiao, namely upper, middle, and lower jiao. It then creates the theory that Cun, Guan, and Chi pulses are respectively related to the upper, middle and lower jiao, which is known as the exterior-interior relationship between Zang-fu organs and three jiao (table 1).
Meanwhile,Mai Jingalso generally categorizes the common syndromes of the exteriorly-interiorly related meridians. For example, excess in the lung and large intestine will cause headache, dizziness, madness, and sore throat, etc. It’s one of Wang’s innovations to classify syndromes of exteriorly-interiorly related meridians from the perspectives of three jiao and pathology.
2.2 Excess and deficiency of meridian diseases
Huang Di Nei Jing(Yellow Emperor's Classic of Internal Medicine) also talks about excess-deficient syndrome differentiation in meridian diseases, butwith some points stated unclearly. However,Mai Jingremedies the deficit by dividing meridian and Zang-fu diseases into two types, deficiency and excess. Take the Liver Meridian of Foot Jueyin as an example. It’s recorded in Chapter Meridians ofLing Shu(Miraculous Pivot) that when this meridian is diseased, it will be manifested by extreme pain in the lumbar causing inability to stretch; hernia in male patients; swollen lower abdomen in females; dry throat and pale complexion in severe cases. Patients with diseased liver will have fullness in chest, vomiting, diarrhea, hernia, enuresis, or oliguria. It does not tell clearly whether the above diseases and syndromes are deficient or excess.Mai Jingdiscusses about liver deficiency and liver excess in Chapter 2 of Volume 2: “yin deficiency in Guan pulse of the left hand reflects the disease of the Foot Jueyin Meridian, manifested by hardness beneath hypochondrium, aversion to cold and fever, fullness in abdomen, poor appetite, abdominal swelling, moodiness, menstrual problems, and pain in lumbar and abdomen; yin excess in Guan pulse of the left hand refers the disease of the Foot Jueyin Meridian, manifested by hardness in epigastric area, pain in bilateral hypochondriums, and hurried breath as if in anger. It offers evidence to the differentiation of excess and deficient syndromes.
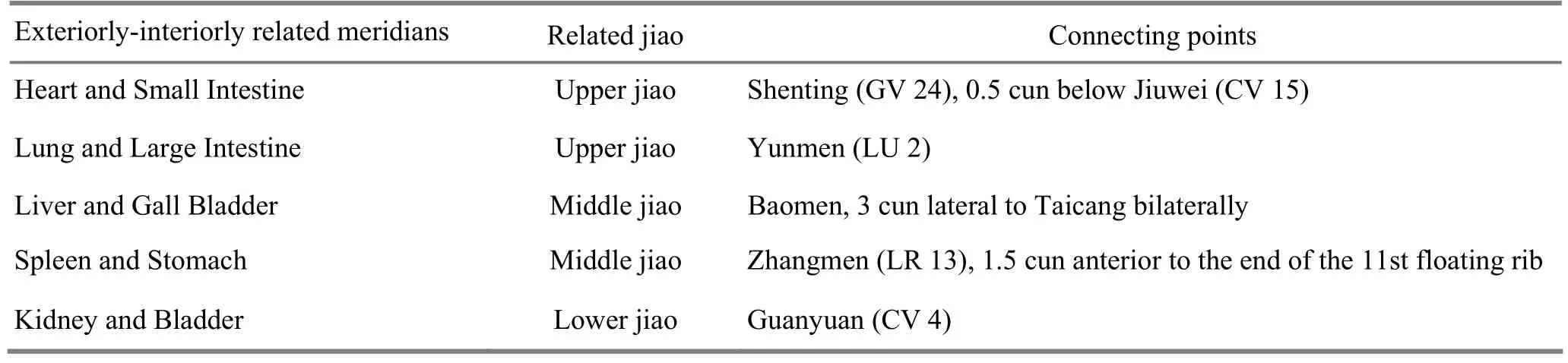
Table 1. Connecting locations of Zang-fu organs with three jiao
The prominent characteristic of deficient-excess hypothesis is that it combines pulse taking and differentiation of Zang-fu and meridian syndromes closely, by differentiating deficiency and excess according to pulse diagnosis and then establishing treatment principles. For example, it says in Chapter 1 of Volume 2 ofMai Jingthat yang exhaustion in the left Cun pulse indicates exhaustion of the Small Intestine Meridian, present by pain or numbness in umbilicus, mass in lower abdomen, cold feeling in heart. It should be treated by puncturing the Heart Meridian to correct yin aspect by selecting Daling (PC 7). Yang-excess in the left Cun pulse indicates excess in the Small Intestine Meridian, present by pain or numbness in lower-heart area, heat in the small intestine, yellowish urine. It should be treated by puncturing Hand Taiyang Meridian to correct yang aspect by selecting acupoint Houxi (SI 3).
Regarding pulse locations, the left Cun, Guan, and Chi pulses are considered representing the heart, liver, and kidney, while the right Cun, Guan, and Chi pulses are representing the lung, spleen, and kidney (life gate). Since Six Fu organs are paired with Five Zang organs according to five elements theory, so as mentioned above, the left Cun pulse refers to both small intestine and heart. Regarding pulse forms, sufficiency and deficiency define yin and yang, e.g. changes of yang in Cun pulse determine small intestine, and changes of yin determine heart. The Heart Meridian, the meridian of yin, is treated when it’s yang exhaustion; Small Intestine Meridian, the meridian of yang, is treated when it’s yang excess. Vice versa, the Small Intestine Meridian is treated when it’s yin exhaustion, and Heart Meridian is treated when it’s yin excess. Other organs are treated likewise.
Besides, Wang also supplemented diseases and syndromes of the extraordinary meridians, such as diseases of the Governor Vessel. Gu Kong Lunof Su Wen(Plain Questions) only mentions opisthotonos, and the 29th Medical Problem ofNan Jing(Classic of Difficult Issues) only records unconsciousness due to rigidity of spine. However,Mai Jing(Volume 2, Chapter 4) made important supplements when discussing about the diseases of extraordinary meridians. When talking about the Governor Vessel, it adds stiff pain in lumbar vertebrae causing inability to stretch or bow, mania in adults, and epilepsy in kids. It is of great significance for the treatment of epilepsy and mania by using the Governor Vessel acupoints.
2.3 Integrative use of four diagnostic methods, combining application of acupuncture and medication
Wang paid much attention to sphygmology, but he didn’t depend solely on pulse diagnosis. On the contrary, he always used the four diagnostic methods together. Whenever he determined pulse conditions, he would describe symptoms at the same time. While obtaining every single symptom, he would also inspect whether there was ulcer in mouth, irritability, shortness of breath, and dozing eyes, etc. Wang also adopted auscultation and olfaction to judge cold and heatsyndromes. For example, in cases of coldness, deficient heat, and heat in the stomach, he would make further judgment according to the odor of vomit and discharges. He confirmed syndromes by pulses, combined four diagnostic methods, and integratively used acupuncture and medication. Therefore, we can see that inMai Jing(Volume 2, Chapter 3), there recorded the treatment of wind stroke byGui ZhiTang(Decoction of Ramulus Cinnamomi) together with acupuncture at Fengchi (GB 20), Fengfu (GV 16), as well as moxibustion and application ofZhi Feng Gao(Paste of Treating Wind); in treatment of febrile, Wang prescribedMa Huang Tang(Decoction ofHerba Ephedrae), plus acupuncture at Meichong (BL 3) and Taiyang (EX-HN 5), along with paste for febrile and moxibustion at acupoints for expelling wind;Qian Hu Tang(Decoction of Radix Peucedani) and acupuncture at Taiyang (EX-HN 5) and Juque (CV 14) with reducing needling technique were used to treat fullness in chest and vomiting. These all reflect the integrative treatment method combining acupuncture-moxibustion and herbal medication, which has significantly improved the treatment result.
2.4 Expanding the application of Five Shu-Transport, Back-Shu and Front-Mu points
Wang described the locations of the Back-Shu and Front-Mu points of the gall bladder and liver, spleen and stomach, lung and large intestine, kidney and bladder.Mai Jing(Volume 3) states that the Back-Shu point of liver is located at T9, and its Front-Mu point is Qimen (LR 14); the Back-Shu point of gall bladder is at T10, and its Front-Mu point is Juque (CV 14). The Back-Shu point of small intestine is at S1, and its Front-Mu point is Guanyuan (CV 4). These records have significantly enriched the Back-Shu and Front-Mu theories inHuang Di Nei JingandNan Jing(Classic of Difficult Issues).
Wang preferred to apply acupuncture to Five Shu-Transport points and moxibustion to Back-Shu and Front-Mu points to treat Five Zang diseases. InMai Jing(Volume 6), it states that if there are green expression, spasm of limbs, fullness in hypochondriums, dizziness, and wiry long pulse in liver disease, it is treatable. The proper treatment should beFang Feng Zhu Li Tang(Decoction of Radix Saposhnikoviae and Bamusa Tuldoides Munro),Qin Jiao San(Radix GentianaeMacrophyllae Powder), and acupuncture at Dadun (LR 1) in spring, Xingjian (LR 2) in summer, Ququan (LR 8) in winter, all with tonifying needling technique. Taichong (LR 3) should be selected in the last month of summer and Zhongfeng (LR 4) should be punctured in autumn both with reducing needling technique. Besides, moxibustion is performed at Qimen (LR 14) with a hundred cones and at T9with 50 cones. Of the points, Dadun (LR 1), Xingjian (LR 2), Taichong (LR 3), Zhongfeng (LR 4), and Ququan (LR 8) are all Five Shu-Transport points; Qimen (LR 14) is the Front-Mu point of liver and T9is the Back-Shu point of liver. The Five Shu-Transport points should be selected according to seasons and the Back-Shu and Front-Mu points can be used anytime by the 74th Medical Problem ofNan Jing.
3 Other Academic Achievements
Wang Shu-he is well known forMai Jing, in which various pulses are divided into 24 kinds. It has further systemized the theories and methods of sphygmology and compared the similar pulses for being easily mastered, making important contributions to the research on sphygmology. Moreover, he reorganizedShang Han Za Bing Lun(Treatise on Cold Damage and Miscellaneous Diseases) of Zhang Zhong-jing.
4 Conclusion
Besides the aforementioned academic achievements, Wang Shu-he also recorded over 50 acupoints inMai Jing, and more than 20 of them were present for the very first time. This book has also enriched the theories of meridian diseases, diagnosis and syndrome differentiation. In the field of acupuncture-moxibustion,Mai Jingalso made some innovative contributions, such as the depth of needling, and cones of moxibustion. All of these are significant in supplementing the academic theories of acupuncture-moxibustion, and in promoting the development of acupuncture-moxibustion techniques.
Translator: Hong Jue
R2-09
A
Date: August 31, 2012
Author: Le Yi-min, professor, supervisor of master candidates. E-mail: leyimin2000@yahoo.com.cn
Chen Yong. E-mail: 13576049679@163.com
 Journal of Acupuncture and Tuina Science2013年1期
Journal of Acupuncture and Tuina Science2013年1期
- Journal of Acupuncture and Tuina Science的其它文章
- Treatment of Tolosa-Hunt Syndrome with Acupuncture: A Case Report
- Research Progress of Acupuncture Analgesia for Labor
- Clinical Study on Puncturing Houxi (SI 3) Toward Hegu (LI 4) plus Lumbar Movement for Acute Lumbar Sprain
- Therapeutic Effect of Warm Needling Therapy Combined with Rehabilitation Therapy for Brachial Plexus Injury after Surgery
- Electroacupuncture in Treating Depression: A Randomized Controlled Study
- Study on the Relation Between MRI Findings and Acupuncture Effect in Trigeminal Neuralgia Patients
