Effect of screening colonoscopy frequency on colorectal cancer mortality in patients with a family history of colorectal cancer
Li Zheng,Bin Li,Ling Lei,Li-Jia Wang,Zhi-Ping Zeng,Jian-Dong Yang
Abstract BACKGROUND Colorectal cancer is a common malignant tumor in China,and its incidence in the elderly is increasing annually.Inflammatory bowel disease is a group of chronic non-specific intestinal inflammatory diseases,including ulcerative colitis and Crohn’s disease.AIM To assess the effect of screening colonoscopy frequency on colorectal cancer mortality.METHODS We included the clinicopathological and follow-up data of patients with colorectal cancer who underwent laparoscopic colectomy or open colectomy at our Gastrointestinal Department between January 2019 and December 2022.Surgical indicators,oncological indicators,and survival rates were compared between the groups.The results of 104 patients who met the above criteria were extracted from the database (laparoscopic colectomy group=63,open colectomy group=41),and there were no statistically significant differences in the baseline data or follow-up time between the two groups.RESULTS Intraoperative blood loss,time to first ambulation,and time to first fluid intake were significantly lower in the laparoscopic colectomy group than in the open colectomy group.The differences in overall mortality,tumor-related mortality,and recurrence rates between the two groups were not statistically significant,and survival analysis showed that the differences in the cumulative overall survival,tumor-related survival,and cumulative recurrence-free rates between the two groups were not statistically significant.CONCLUSION In elderly patients with colorectal cancer,laparoscopic colectomy has better short-term outcomes than open colectomy,and laparoscopic colectomy has superior long-term survival outcomes compared with open colectomy.
Key Words: Colorectal cancer;Laparoscopic surgery;Open surgery;Prognosis;Laparoscopic colectomy;Open colectomy
lNTRODUCTlON
Colorectal cancer is a common malignant tumor in China[1-5].Owing to an increase in the elderly population,the incidence of colorectal cancer in the elderly is increasing annually[6-10].There is no consensus on whether patients should undergo open or laparoscopic colectomy[11-15].Furthermore,elderly patients with colorectal cancer have a high mortality rate after open colectomy[16],and early randomized controlled clinical studies on the short-and long-term outcomes of laparoscopic colectomy mostly excluded elderly patients.Until recently,the results of short-term studies have confirmed the applicability of laparoscopic colectomy in elderly patients.Although the short-term outcomes of laparoscopic colectomy in elderly patients with colorectal cancer have been reported to be superior to those of open colectomy in China,few reports have analyzed the long-term survival outcomes both in China and around the world[17-20].In clinical practice,diverse temporal frequencies may affect screening accuracy.Therefore,we assessed the effect of screening colonoscopy at different frequencies on the mortality of patients with colorectal cancer and a family history of rectal cancer.
MATERlALS AND METHODS
General information
Patients with colorectal cancer who underwent laparoscopic or open colectomy at our Gastrointestinal Department between January 2019 and December 2022 according to the American Joint Committee on Cancer tumor-node-metastasis staging system (7thedition) were included in this study.Patients were selected according to the following criteria: Patients aged > 65 years;those who had postoperative pathologically confirmed primary colorectal or mucinous adenocarcinoma;and those who successfully underwent radical D3 resection,except for emergency colectomy.The patients were treated with a 5-fluorouracil-based postoperative chemotherapy regimen.
Observation indicators
Clinical and pathological data,including age,sex,tumor location,tumor size,degree of differentiation,type of pathology,surgical procedure,and tumor-node-metastasis stage,were included as observation indicators.
Perioperative-related indicators
Preoperative comorbidities,history of abdominal colectomy,mean operative time,intraoperative blood loss,postoperative length of hospital stay,time to first ambulation,time to first fluid intake,time to first gastric discharge,and postoperative complications were included as perioperative indicators.The above indexes were measured in both groups.Except for different treatment methods,the other arrangements were consistent between the two groups.
Oncological and prognostic indicators
The length of the specimen,distance of the tumor from both sides of the excised edge,number of dissected lymph nodes,number of positive lymph nodes,recurrence rate,overall survival rate,and tumor-related survival rate were included as oncological and prognostic indicators.
Statistical analysis
SPSS 25.0 software was used for statistical analyses.Measurement data are expressed as the mean ± SD,and thet-test was used for comparison between groups and within groups.Enumeration data are expressed as percentages or composition ratiosn(%),and theχ2test was used for comparison between groups and within groups.P< 0.05 was considered statistically significant.
RESULTS
Comparison of clinical and pathological data between the two groups
The results of 104 patients who met the above criteria were extracted from the database (laparoscopic colectomy group=63,open colectomy group=41).The differences in sex,age,tumor location,tumor size,degree of differentiation,and pathological stage between the two groups were not statistically significant (Table 1).
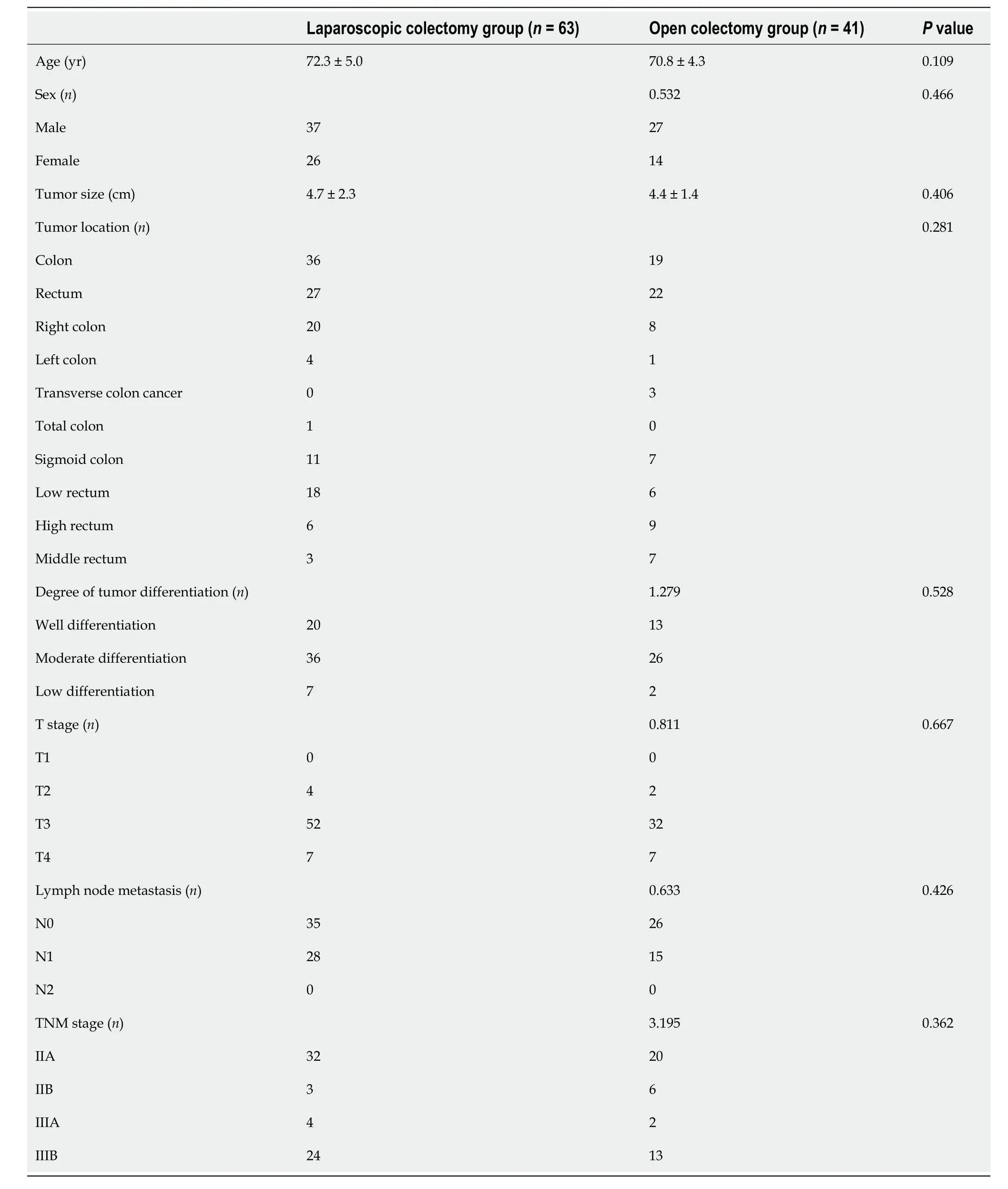
Table 1 Comparison of clinical and pathological data between the two groups
Comparison of perioperative-related indicators between the two groups
Except for the preoperative anemia rate,which was higher in the laparoscopic colectomy group than in the open colectomy group,no statistically significant difference was noted between the two groups in terms of preoperative comorbidities and preoperative abdominal digestive disease history;intraoperative blood loss,time to first ambulation,and time to first fluid intake were significantly lower in the laparoscopic surgery group than in the open surgery group.The mean operative time was slightly longer in the laparoscopic colectomy group than in the open colectomy group,although the difference was not statistically significant.
Comparison of oncological indicators between the two groups
No statistically significant differences were noted in the length of the specimens,distance of the tumor from the cut edge on either side,number of lymph nodes dissected,or number of positive lymph nodes between the two study groups (Table 2).
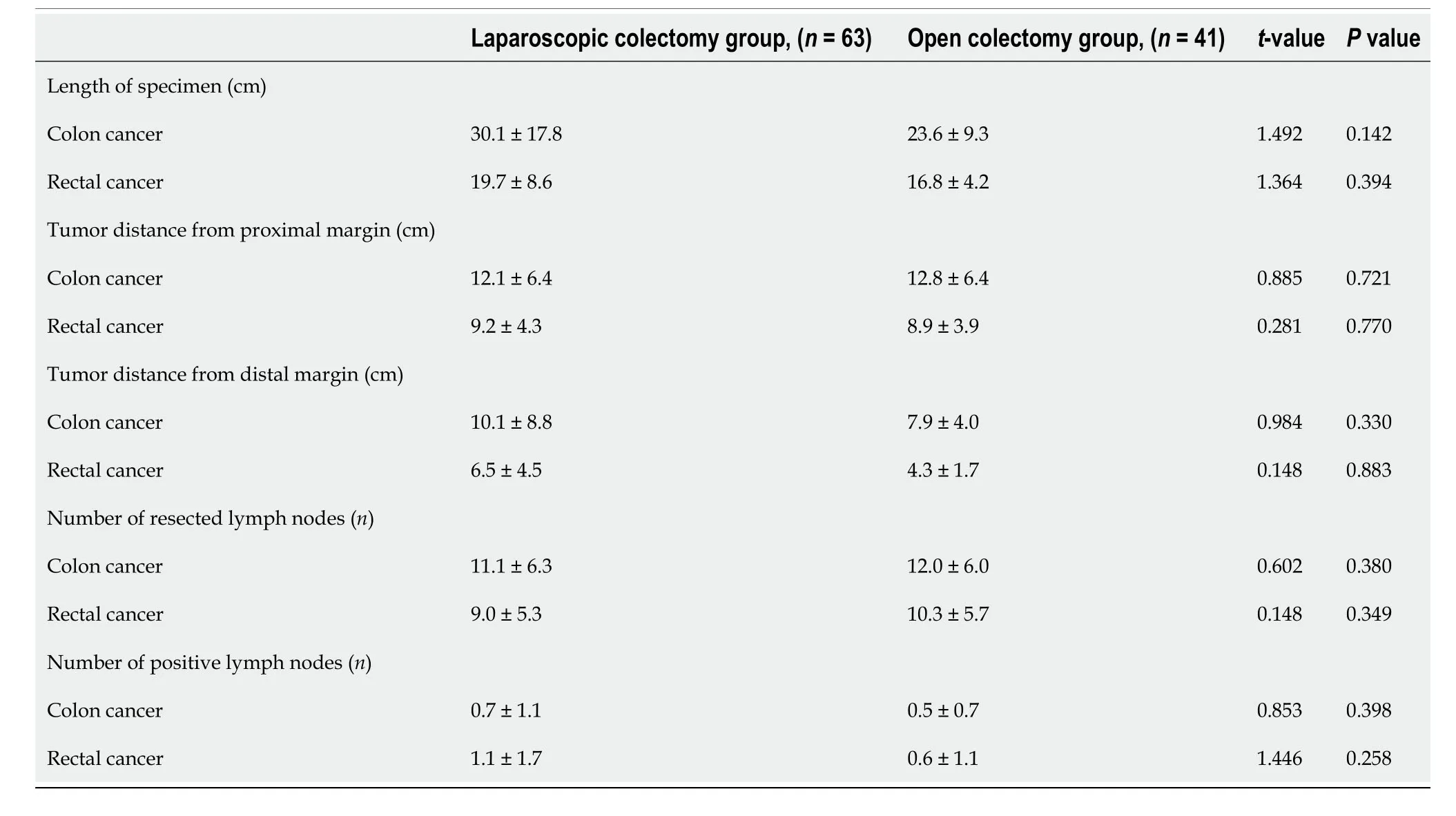
Table 2 Comparison of oncological indicators between the two groups
Comparison of intestinal cleaning compliance rate between the two groups
The compliance rates of intestinal cleanliness in the observation and control groups were 90.47% and 53.66% (144/200),respectively,thus indicating a significant difference (Table 3).
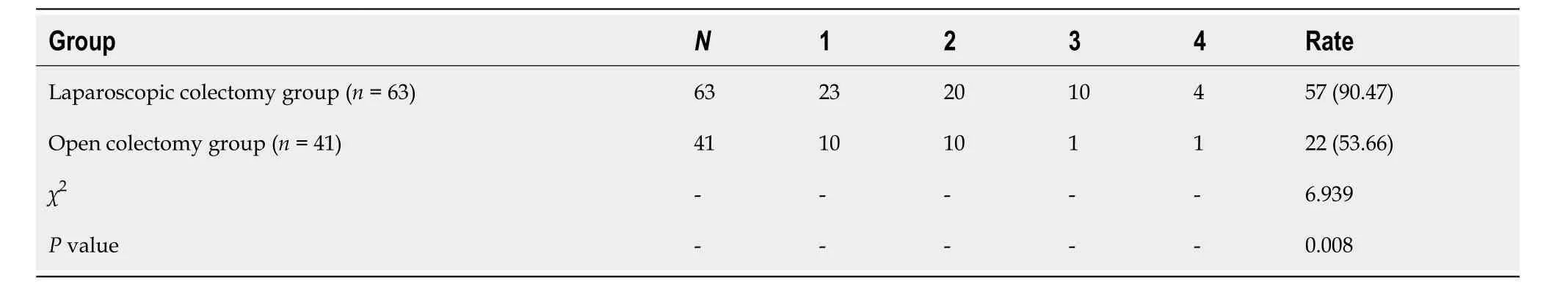
Table 3 Comparison of intestinal cleaning compliance rate between the two groups,n (%)
Bowel examination preparation
The Boston bowel preparation scale score and adenoma detection rate in the laparoscopic colectomy group were higher than those in the open colectomy group,whereas the colonoscopy time was shorter than that in the control group (P< 0.05) (Table 4).Based on Tables 1-4 and the current research results,it can be seen that the frequency of colonoscopy had a greater impact on the mortality of colorectal cancer in patients with a family history of colorectal cancer,which can be used as a means of evaluation.
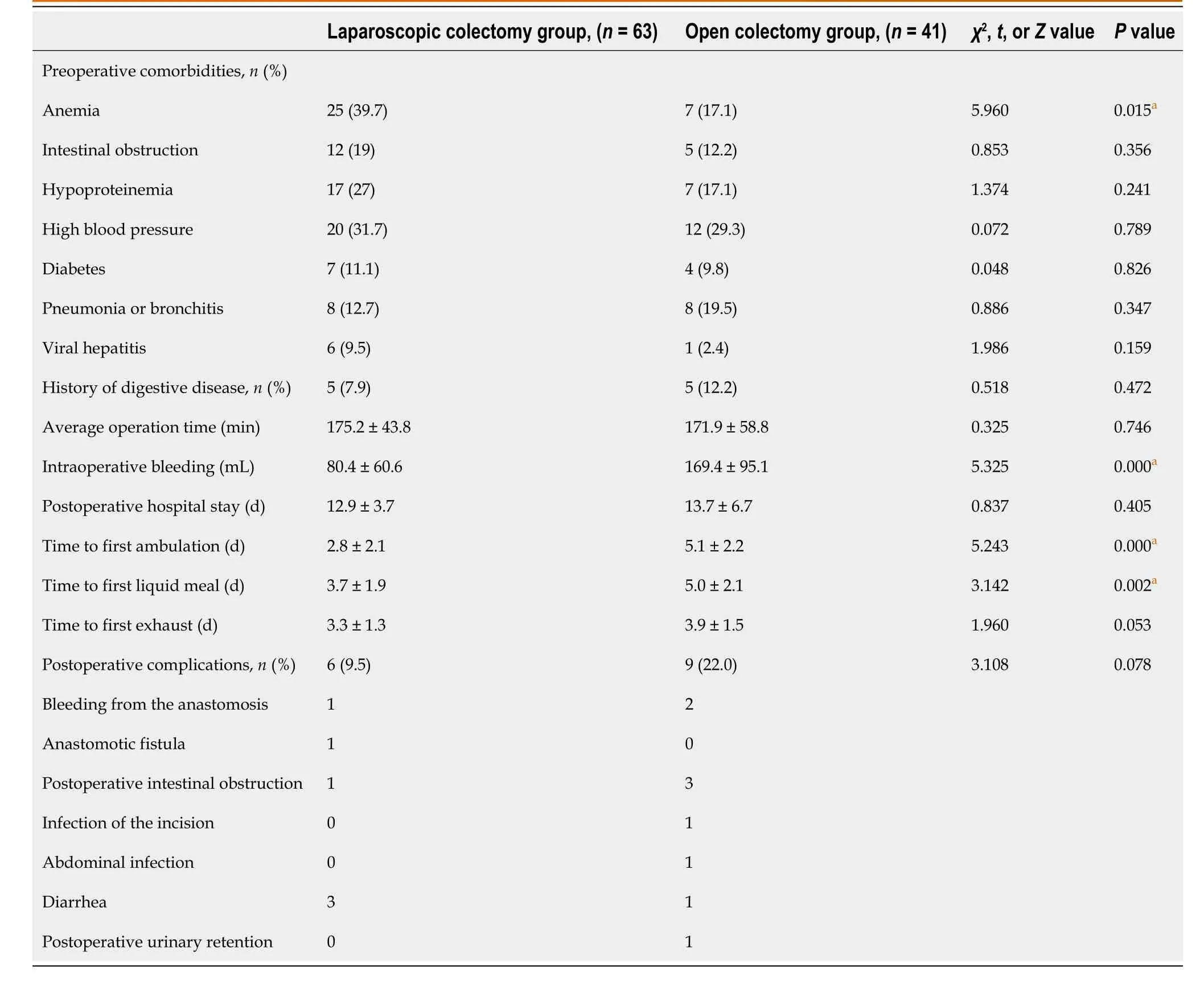
Table 4 Comparison of perioperative-related indicators between the two groups
DlSCUSSlON
Delay in consultation is common in patients with a positive family history of colorectal cancer
This study found that patients with a positive family history of colorectal cancer experienced serious delays in consultation[21-25],with a delay rate of 39.9%,and many patients missed the optimal time for early detection and treatment of colorectal cancer[26-30].The results of the univariate analysis showed that a longer time to consultation is associated with a more advanced pathological stage and worse prognosis.Therefore,delayed consultation seriously affects the prognosis of patients and increases the burden on families and the society.The reason for the delay in consultation in the current study was that the hospital where the study was conducted is a higher-level specialist hospital where patients from various regions of the country visit,and the patient’s knowledge of the disease varied.Conversely,a previous study conducted the study at a general hospital,and the patients included were mostly residents of the big city where they were located[29];furthermore,the patients had sufficient knowledge of the disease and medical examination findings.Therefore,consultations were conducted in a timely manner.The delay in consultation of patients in the present study was similar to that in studies from other developing countries[31] but was more serious than that in Denmark[32].This finding may be related to differences in socioeconomic and cultural environments,particularly in health service policies,resources,and organizations in different regions,in addition to individual factors[33].
The level of social support for patients with colorectal cancer and a positive family history of colorectal cancer is low and needs improvement
The effect of social support as an available external resource wherein individuals engage with and receive information,comfort,and reassurance from other people or groups in formal and informal ways[34] has received increasing attention in the field of nursing.Good social support has a positive effect on the physical and mental health of patients with cancer[35].The results of the present study showed that the total social support score of patients with colorectal cancer and a family history of colorectal cancer (37.51 ± 8.43) was higher than that of the normal population.The reason for the low level of social support in this study could be attributed to the fact that negative tumor-related events in other members of the family tended to make patients feel negative and unable to seek and use social support.Moreover,it specifies that most patients failed to understand the positive role of social support for patients with cancer and were unable to obtain a high level of social support from their sick relatives during previous medical treatment.Therefore,healthcare professionals should pay special attention to patients with a positive family history of cancer,understand their level of socialsupport,take effective measures to improve the social support of each individual,encourage patients and their relatives to socialize more with friends,encourage behaviors that could help others,and seek external help for increasing social support.Healthcare professionals should use appropriate communication methods to provide effective social support to patients.
Timing of consultation for patients with colorectal cancer and a positive family history of colorectal cancer is influenced by multiple factors
The timing of patient visits in the present study was influenced by several factors,including the level of social support,medical examinations,and number of relatives with cancer.
Effect of social support level on consultation timing:The results of this study showed that the level of social support was significantly negatively associated with the delay in patient hospital visits and that the lack of social support significantly increased the delay in hospital visits,thus suggesting that good social support has an enabling effect on patients’ timely hospital visits.This finding is in line with the findings of both national and international studies.Patients who lack social support may be less able to adapt psychosocially,thus leading to high levels of psychological stress and negativity,which may affect their self-esteem levels and coping methods.Furthermore,individuals who lack social support may receive less positive advice and opinions from others regarding seeking medical care,thus ultimately predisposing them to delays in seeking medical care.Previous studies have shown that talking to others after symptoms have been identified can reduce delays in consultation,and close relationships with family members can help determine symptoms and facilitate consultation.Patients who are living alone are more likely to experience delays in consultation than those living with family members,and many patients are persuaded and encouraged by family members to seek consultation.Therefore,healthcare professionals should teach patients on how to obtain support from their families and instruct patients’ relatives on how to help and encourage patients obtain support from outside the family,particularly for the management of cancer within their family.Mutual support for the entire family is important.
Effect of medical examination status on consultation timing:This study showed that the length of delay in consultation for patients with colorectal cancer was significantly correlated with the status of medical examination,and the delay inconsultation was shorter for patients who had undergone medical examination than for those who had never undergone a medical examination.Those who had undergone a medical examination were more aware of the disease,more worried about their health condition,more alert,and more likely to consult the doctor immediately after the appearance of symptoms (Table 5).
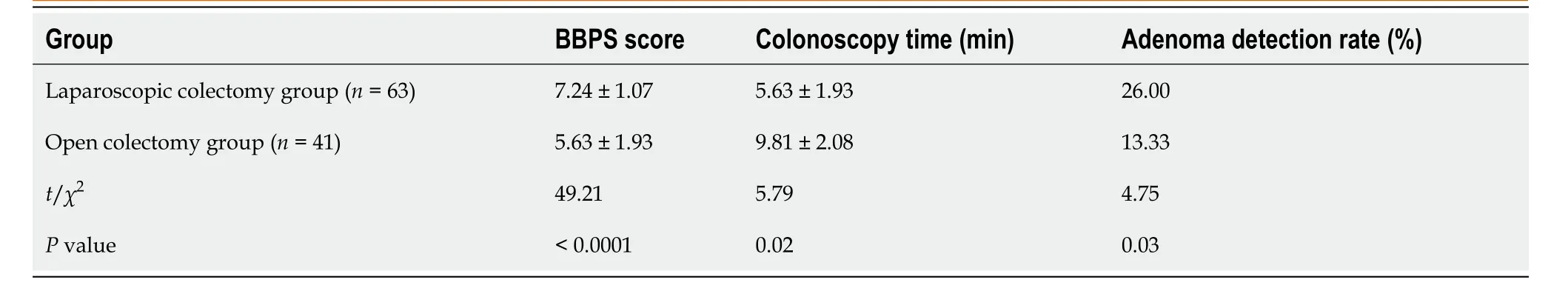
Table 5 Comparison of results of bowel preparation assessment in 104 patients undergoing colonoscopy
Colorectal cancer can be immediately detected during physical examinations;thus,the time to visit a doctor is greatly reduced.However,the results of this study showed that more than half of the patients with colorectal cancer had never undergone a physical examination and that only eight patients (5.2%) had been screened for colorectal cancer.This indicates that although the prevention and treatment of colorectal cancer are receiving increasing attention,prevention and treatment efforts are quite uneven across regions,and the cooperation of some patients is low compared with patients in developed countries.
Effect of number of relatives with cancer on consultation timing:The results of this study showed that the number of relatives suffering from colorectal cancer significantly influenced the time taken to see a patient.Patients with three or more relatives with colorectal cancer had significantly shorter times to consultation than other patients.A larger number of relatives with similar diseases may draw the attention of family members to the disease,thus allowing them to actively or passively obtain information about the clinical symptoms,prevention methods,and treatment of the disease;make quicker and riskier decisions;and seek medical attention quickly when they develop symptoms.However,the results of the present study showed that even when relatives had a history of colorectal cancer,the delay in consultation was still significant,and the major reason for the delay was the “l(fā)ack of knowledge and attention”.This is because there is a lack of health education for patients and their relatives on the causes,clinical symptoms,and screening of colorectal cancer during clinical treatment and care.Despite the greater understanding of the genetic mechanism of tumors in recent years,its clinical application has not yet been popularized.Most medical institutions in China are still managing the disease according to the diagnosis and treatment model of sporadic colorectal cancer,thus resulting in high-risk groups not beingidentified in time.
Summary and recommendations
Given that colorectal cancer is a common cancer in China,improving its prevention and control is of great significance to both individuals and the country.This study shows that delayed consultation is common among patients with colorectal cancer and a family history of colorectal cancer,and the acceptance rate of colorectal cancer screening is very low.Therefore,healthcare professionals should pay attention to the intervention of delayed consultation and screening of patients in the secondary prevention of colorectal cancer by taking the following measures: (1) Clinical practice should ensure the accuracy of family history taking to avoid missing diagnosis because of incomplete family history taking;(2) Referring patients with a positive family history of colorectal cancer to oncological genetic counseling for further confirmation of the diagnosis;(3) Explaining in detail the hereditary aspects of colorectal cancer,law of inheritance,and range of high-risk relatives to patients and relatives who are suspected of having a genetic predisposition to the disease;(4) Popularizing the knowledge of symptom recognition and screening of colorectal cancer in medical and nursing staff at all levels to strengthen health education for patients and their relatives and encourage participation in cancer prevention health check-ups;(5) Medical centers that treat a large number of patients with colorectal cancer should adopt case management for the dedicated and systematic management of high-risk families to track colorectal cancer screening,early diagnosis,and treatment of patients’ high-risk relatives;and (6) Emphasizing the importance of education on cancer prevention and control for people in rural and remote areas.
CONCLUSlON
This study was designed to develop effective measures for the prevention,control,and treatment of colorectal cancer.These results provide a scientific basis for the early treatment of tumors in the relatives of patients with hereditary colorectal cancer and for the systematic management of families with hereditary colorectal cancer.This study has great clinical value as a reference for the treatment and prevention of malignant tumors of the gastrointestinal tract.
In summary,screening strategies should be improved,screening should be integrated with other public health campaigns,more cost-effective screening techniques should be sought,screening methods with high sensitivity and accuracy should be explored,risk stratification should be performed using low-cost and high-efficiency risk assessment tools,technologies such as data mining and artificial intelligence should be appropriately utilized to establish a more accurate colorectal cancer screening prediction model,and individualized screening should be carried out for high-risk groups.It also suggests screening methods,starting ages,and screening intervals for different risk groups,and establishes a reasonable screening model.
ARTlCLE HlGHLlGHTS
Research background
Colorectal cancer is one of the common malignant tumors in China,and its incidence in the elderly population has steadily increased.Inflammatory bowel disease is a group of chronic non-specific intestinal inflammatory diseases,including ulcerative colitis and Crohn 's disease.
Research motivation
To evaluate the effect of colonoscopy frequency on the mortality of colorectal cancer.
Research objectives
We included the clinicopathological and follow-up data of patients with colorectal cancer who underwent laparoscopic colectomy or open colectomy at our gastrointestinal department.
Research methods
Surgical indicators,oncological indicators,and survival rates were compared between the groups.The results of 104 patients who met the inclusion criteria were extracted from the database (laparoscopic colectomy group=63,open colectomy group=41),and there were no statistically significant differences in the baseline data or follow-up time between the two groups.
Research results
Intraoperative blood loss,the time to firs ambulation,and time to first liquid meal in the laparoscopic colectomy group were significantly lower than those in the open colectomy group.There was no significant difference in total mortality,tumor-related mortality,or recurrence rate between the two groups.Survival analysis showed that there was no significant difference in cumulative overall survival rate,tumor-related survival rate,or cumulative recurrence-free survival rate between the two groups.
Research conclusions
In elderly patients with colorectal cancer,laparoscopic colectomy has better short-term outcomes than open colectomy.
Research perspectives
Laparoscopic colectomy has superior long-term survival outcomes compared with open colectomy.
FOOTNOTES
Author contributions:Zheng L and Yang JD contributed equally to this work;Zheng L,Li B,Lei L,Wang LJ,Zeng ZP,and Yang JD designed the study and were involved in the data acquisition and writing of this article;Zheng L and Yang JD contributed to the analysis of the manuscript;and all authors have read and approved the final manuscript.
Supported byScience and Technology Plan of Jiangxi Provincial Health Commission,No.202311202 and No.SKJP220 219076;and the Science and Technology Support Plan Project of Nanchang,Jiangxi Province,No.2020-133-5.
lnstitutional review board statement:The study was reviewed and approved by the First Hospital of Nanchang Institutional Review Board.
lnformed consent statement:All patients provided written informed consent for participation in the study.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Data sharing statement:No additional data are available.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Bin Li 0009-0007-4240-0343;Jian-Dong Yang 0009-0005-1315-963X.
S-Editor:Wang JJ
L-Editor:Wang TQ
P-Editor:Zhang XD
 World Journal of Gastrointestinal Oncology2024年2期
World Journal of Gastrointestinal Oncology2024年2期
- World Journal of Gastrointestinal Oncology的其它文章
- Does enhanced recovery after surgery programs improve clinical outcomes in liver cancer surgery?
- Cardiotoxicity induced by fluoropyrimidine drugs in the treatment of gastrointestinal tumors
- Preoperative controlling nutritional status as an optimal prognostic nutritional index to predict the outcome for colorectal cancer
- Tumour response following preoperative chemotherapy is affected by body mass index in patients with colorectal liver metastases
- Expression of cyclin-dependent kinase 9 is positively correlated with the autophagy level in colon cancer
- Progress in the treatment of advanced hepatocellular carcinoma with immune combination therapy
