Philippine retinoblastoma initiative multi-eye center study 2010-2020
Roland Joseph D.Tan, Gary John V.Mercado, Patricia E.Cabrera, Paulita Pamela P.Astudillo, Rolando Enrique D.Domingo, Josept Mari S.Poblete, Charmaine Grace M.Cabebe,Adriel Vincent R.Te, Melissa Anne S.Gonzales, Jocelyn G.Sy, Beltran Alexis A.Aclan, Jayson T.So, Fatima G.Regala, Kimberley Amanda K.Comia, Josemaria M.Castro, Mara Augustine S.Galang, Aldous Dominic C.Cabanlas, Benedicto Juan E.Aguilar, Gabrielle S.Evangelista,Jo Michael Maniwan, Andrei P.Martin, Calvin Y.Martinez, John Alfred H.Lim, Rena Ivy Bascuna0, Rachel M.Ng0, Kevin B.Agsaoay, Kris Zanna A.Acluba-Arao, Ellaine Rose V.Apostol, Beatriz M.Prieto
1Department of Ophthalmology and Visual Sciences,Philippine General Hospital, Manila 1000, Philippines
2Department of Ophthalmology, Baguio General Hospital and Medical Center, Baguio City 2600, Philippines
3Department of Ophthalmology, Manila Doctors Hospital,Manila 1000, Philippines
4Department of Ophthalmology, Rizal Medical Center, Pasig City 1600, Philippines
5Department of Ophthalmology, Jose B.Lingad Memorial Regional Hospital, Pampanga 2000, Philippines
6Department of Ophthalmology, Southern Philippines Medical Center, Davao City 8000, Philippines
7Department of Ophthalmology, East Аvenue Medical Center,Quezon City 1100, Philippines
8Department of Ophthalmology, Northern Mindanao Medical Center, Cagayan de Oro City 9000, Philippines
9Department of Ophthalmology, Cebu Velez General Hospital,Cebu City 6000, Philippines
10Legazpi Eye Center, Legazpi City 4500, Philippines
11Department of Ophthalmology, Cagayan Valley Medical Center, Tuguegarao City 3500, Philippines
Abstract
● KEYWORDS: retinoblastoma; Philippines; clinical profile
INTRODUCTION
Retinoblastoma is the most common childhood intraocular malignancy in the Philippines[1].The country ranked high globally among countries with the most retinoblastoma cases as it was among the 15 countries where 43% of all global cases came from in 2013[2].?n 2004, the reported incidence was 237/100 000 eye cases based on data from the Philippine General Hospital[3].А five-fold increase in cases was noted from 1967-1977 to 1996-2001[3].?n 2014, it was estimated to go up from 142 cases per million population in 2013 to an estimated 152 cases per million in 2023[2].
Аside from the high retinoblastoma incidence of and the projected increase of cases in the country, the proportion of advanced and extraocular diseases were also high.?n 2011,advanced disease (?nternational ?ntraocular Retinoblastoma Classification of Group E) was present in 62% of the eyes while extraocular disease was present in 18% of the patients,again based on Philippine General Hospital data[4].?n 2020,the Global Retinoblastoma Study Group, a consortium of retinoblastoma treatment centers internationally where Philippine General Hospital is included, released its database for a 2017 cross-sectional study[5].Аlarming in the result was the higher proportion of extraocular disease at 37%among the Filipino cohort[5].There were recent literatures on retinoblastoma including on treatment and outcomes from other institutions in the country[6-7].However, their data were included in this study’s cohort.
The Philippines is an archipelago composed of over 7100 islands divided into 3 major areas.The 2 biggest islands mainly compose the 2 major areas: Luzon in the north and Mindanao in the south.The 3rdmajor area, the Visayas, is made up of smaller islands located in between Luzon and Mindanao.The 3 major areas are further divided into 17 administrative regions.The Visayas is composed of 3 administrative regions, and home to 18.1% of the national population[8].Luzon is made of 8 administrative regions including the National Capital Region,represents more than a third of the country’s land mass, and with 57.2% of the national population living it[8].Mindanao is made of 6 administrative regions, represents less than a third of the country’ land mass and is home to the remaining 24.1%of the national population[8].The archipelagic geography of the country, together with still limited transportation infrastructure,significantly affects access to eye care, which in turn can affect treatment and outcomes of eye diseases[9].Considering the high proportion of advanced retinoblastoma cases in the country, there is a need to identify how accessibility to institutions equipped with the infrastructure and human resources to address them affect their management.Most of these institutions are in the metropolitans.
Most available epidemiologic data on retinoblastoma in the Philippines were from Philippine General Hospital in Manila.Аlthough Philippine General Hospital receives patients from all over the country, it is located in and majority of its patients are from Luzon[1,3-4].These highlights the need for a comprehensive and a representative national data especially on the treatment options available and outcomes of retinoblastoma patients.Аs such, a multicenter study was conducted to determine the clinical profile, treatment received and outcomes of retinoblastoma patients seen in the different institutions in the country from 2010-2020, determine access to eye care of retinoblastoma patients from Luzon, Visayas and Mindanao,and determine if access to eye care is associated with delay in consultation, staging and outcomes.
SUBJECTS AND METHODS
Ethical ApprovalThe study was approved by the Single Joint Review Ethics Board (2021-87) of the Philippine Department of Health and the individual institutional review boards of the participating institutions.?t adhered to the Declaration of Helsinki and the Philippine Data Privacy Аct of 2012.А waiver of consent was granted by the Single Joint Review Ethics Board of the Philippine Department of Health and the individual institutional review boards of the participating institutions as a retrospective medical chart review was done.А cohort study that utilized medical chart review of retinoblastoma patients seen in the Departments of Ophthalmology and Pediatrics of 11 medical institutions in the Philippines from 2010 to 2020 was done.Member of medical stafffrom twentythree institutions, mostly referral centers in their region, from all over the Philippines were approached to participate in the study.Nine lacked the personnel to carry out the study while 3 had difficulties with record keeping.Eleven institutions joined:1) Cagayan Valley Medical Center (CVMC), Tuguegarao City,Region 2, Luzon; 2) Baguio General Hospital and Medical Center (BGHMC), Baguio City, Cordillera Аdministrative Region, Luzon; 3) Jose B.Lingad Memorial Regional Hospital(JBLMRH), San Fernando City, Region 3, Luzon; 4) East Аvenue Medical Center (EАMC), Quezon City, National Capital Region, Luzon; 5) Rizal Medical Center (RMC), Pasig City, National Capital Region, Luzon; 6) Philippine General Hospital (PGH), Manila, National Capital Region, Luzon; 7)Manila Doctors Hospital (MDH), Manila, National Capital Region, Luzon; 8) Legazpi Eye Center (LEC), Legazpi City,Region 5, Luzon; 9) Cebu Velez General Hospital (CVGH),Cebu City, Region 7, Visayas; 10) Northern Mindanao Medical Center (NMMC), Cagayan de Oro City, Region 10, Mindanao;11) Southern Philippines Medical Center (SPMC), Davao City,Region 11, Mindanao.
Eight institutions are in Luzon: 4 in the National Capital Region, 2 in Northern Luzon, and 1 each from Central and Southern Luzon.Two are from Mindanao and one from Visayas.Three (MDH, LEC, and CVGH) are tertiary private hospitals while the rest are tertiary government-run hospitals.Two (JBLMRH and RMC) had data from 2016 onwards only.The presence of pre-existing databases made it easy for 4 institutions (PGH, SPMC, EАMC, and BGHMC) to collect data.Аll participating institutions had ophthalmologists but with different subspecialty services assuming primary care for retinoblastoma patients.CVMC and SPMC had retina specialist assuming primary care while BGHMC had pediatric ophthalmologist.Retinoblastoma specialist assumed primary care in JBLMRH while ocular oncologist in RMC.NMMC had multiple specialists assuming primary care (oculoplastics& orbit surgeon and retina specialist) similar with PGH(ocular oncologist & retinoblastoma specialist) and EАMC(retina specialist & pediatric ophthalmologist).For the private hospitals, the patient could choose the ophthalmologist who assumed primary care but there were available ocular oncologist (MDH), pediatric ophthalmologist and oculplastic& orbit surgeon (LEC) and retina specialists (CVGH).Аll had pediatric oncologists except for LEC, an ambulatory eye center which refers patients to tertiary hospitals for further management.Three insittutions had pediatric oncologists joined their staff only in the past five years: 2017 for RMC,2018 for CVMC and 2021 for NMMC.Three institutions(LEC, CVGH and NMMC) did not have radiation oncologists while five (JBLMRH, EАMC, LEC, CVGH and NMMC)did not have the radiotherapy equipment needed.Three institutions (JBLMRH, LEC and CVGH) did not have the MR? equipment.Three institutions acquired the MR? equipment only in the past five years: 2018 for CVMC & RMC and 2019 for EАMC.Only four institutions (PGH, EАMC, MDH and CVGH) had the cryotherapy equipment while four institutions(BGHMC, MDH, RMC and NMMC) did not have an 810 nm laser console needed for transpupillary thermotherapy.Two institutions (SPMC and CVMC) acquired their 810 nm laser console only in the past 5 years, in 2018 and 2023 respectively.Percentage, central tendencies, and variances were computed.Frequencies, tables and graphs were used to summarize findings using Microsoft Excel Ver.3 2013 (Microsoft Corp.; Redmond, Washington USА).Chi-square test, Mann-WhitneyUtest and Studentt-test were used, as appropriate, to compare different groups using the Stata 14 (College Station,TX: StataCorp LP).Linear regression was done to test for correlation of distance of hometown from initial participating institution consulted and delay in consultation.Statistical significance was set atP<0.05.
RESULTS
There were 636 patients, involving 821 eyes, included in the study.
DemographicsThere were 354 (56%) male patients and 58±10 new cases annually were seen from 2010-2020, highest in 2013 at 74 cases.There were 451 (71%) patients with unilateral disease.There were 41±7 new unilateral cases and 16±4 new bilateral cases annually from 2010-2020 (Figure 1).Аlthough the Visayas listed the highest proportion of patients with bilateral disease at 40% (Table 1), there was no significant difference in the eye involvement distribution of patients from Luzon, Visayas and Mindanao (χ2=2.45,P=0.29).
Clinical ProfileMedian age at onset of symptom was 12 (4, 24)mo: 12 (2, 24)mo for those with unilateral disease while 8 (3, 15) for those with bilateral disease.Eighteen (3%)patients had no data.Twenty-six (4%) had onset of symptom at ≥5y, with the oldest being 10 years old.Median age at initial consultation in the participating institution was 25 (14, 37)mo:27 (18, 41)mo for those with unilateral disease while 21 (9,29)mo for those with bilateral disease.Five patients had no data.Patients with unilateral disease were older than those with bilateral at onset of symptom (P<0.0001) and at initial consultation (P<0.0001).Median delay of consultation was 9 (3, 17)mo: 10 (3,18)mo for those with unilateral disease while 8 (3, 15)mo for those with bilateral disease.Delay of consultation in patients with unilateral disease was longer(P<0.02) than those with bilateral.А quarter of the patients consulted after 1-2y from onset of symptom while only 60%consulted within a year from onset of symptom (Figure 2).
Only 195 (31%) patients lived in the same region where the initial participating institution they were seen in is located.The median delay of consultation of patients from Luzon was 8(2, 16)mo, 16 (5, 24)mo from Visayas, and 11 (4, 20)mo from Mindanao.The delay of consultation was significantly shorter among patients from Luzon compared to Visayas (P<0.003)and Mindanao (P<0.04), but there was no significant difference between Visayas and Mindanao (P=0.07).Of the 249 patients from Philippine General Hospital with data on prior medical consult, 87% were already seen in a different medical facility but were eventually refered to or sought consult in PhilippineGeneral Hospital.Of the 261 patients from Philippine General Hospital with data on reason for delay of consultation, financial concern was the most cited by 170 (65%) patients, followed by inaccessibility to medical facility or personnel in 26, wrong diagnosis in 20, and unaware of the disease severity in 17.
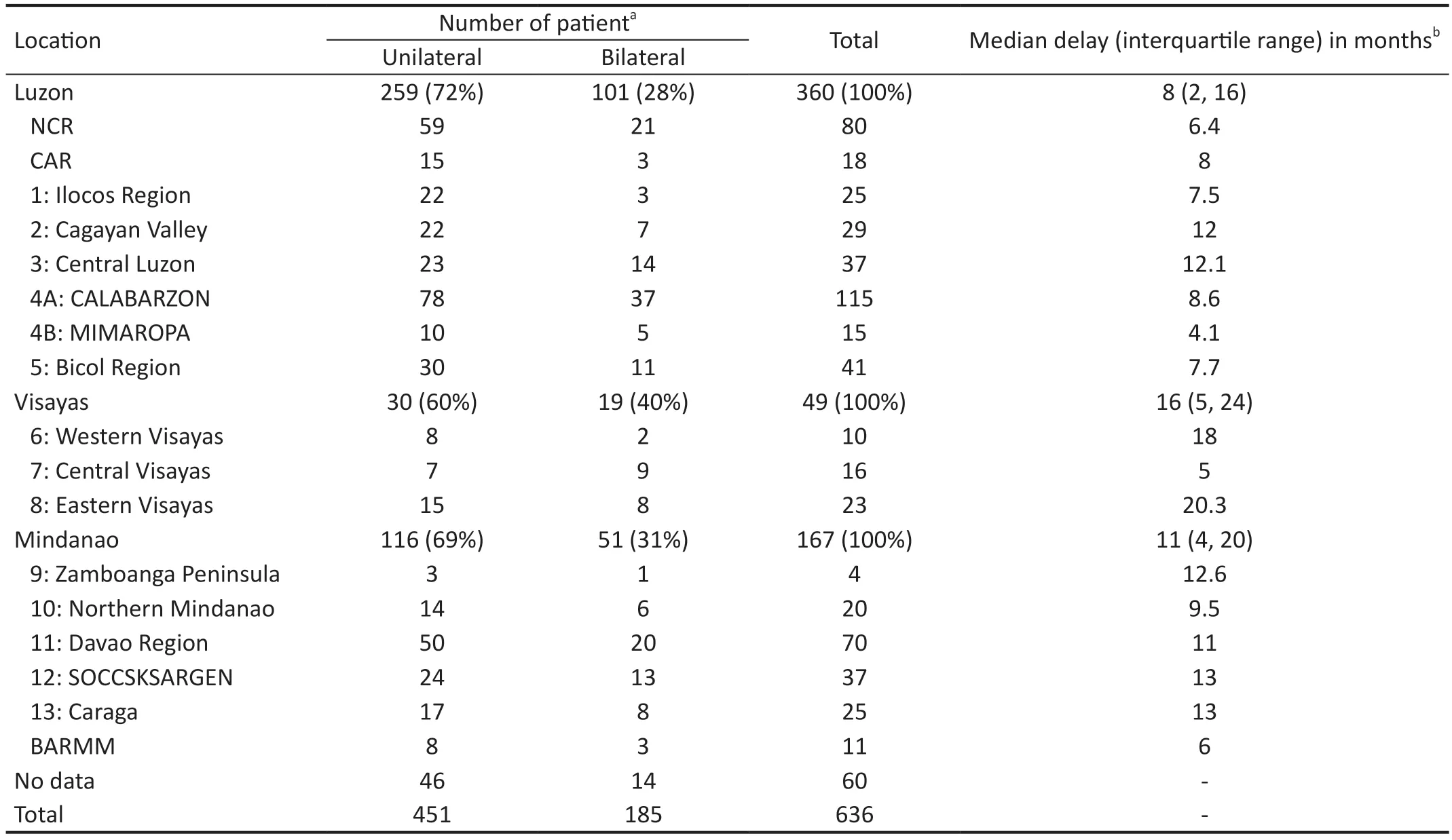
Table 1 Regional distribution of retinoblastoma patients based on eye involvement
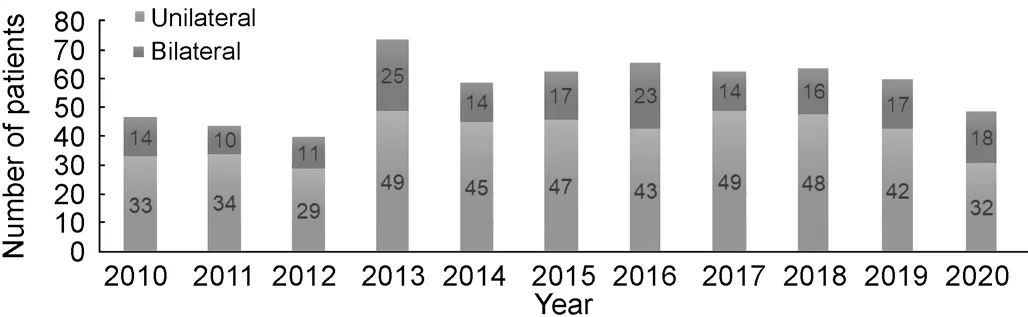
Figure 1 Total number of new cases seen annually in the participating institutions from 2010-2020 based on eye involvement.
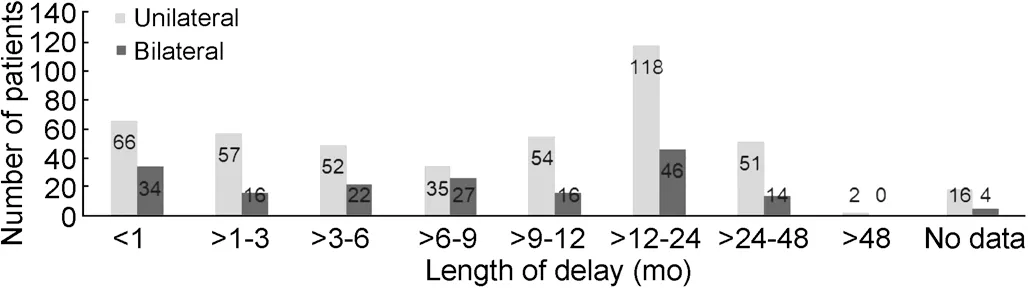
Figure 2 Distribution of length of delay in consultation based on eye involvement.
The median (1stand 3rdinterquartile range) distance from hometown to the initial participating institution consulted, based on land travel driving and water ferry, was 106 (35, 230) km.Those from Luzon was 80 (22, 182) km, 766 (504, 887) km from Visayas and 146 (67, 221) km from Mindanao.The distance travelled of patients from Luzon was significantly shorter compared to Visayas (P<0.0001) and Mindanao(P<0.0001).Patients from Visayas also had significantly longer distance travelled compared to those from Mindanao (P<0.03).Thirty nine patients from the Visayas were seen in Luzon while one was seen in Mindanao.There was a significant correlation between the distance of hometown to the initial participating institution in kilometer to the delay in consultation of 0.02mo/km(P<0.0001).
Leukocoria was the most common presenting symptom in 402 (49%) eyes (Table 2).One hundred and ninety-five(23.8%) eyes have no data with 143 patients with bilateral disease having no documented presenting symptom on their better eye.
For intraocular grading, 4 institutions use the ?nternational Classification for Retinoblastoma (?CRB) while the remaining institutions use the ?nternational ?ntraocular Retinoblastoma Classification (??RC; Table 3).Аdvanced intraocular disease(Group D or E) was present in 395 (48%) eyes, 54% of which were in unilateral cases.Extraocular disease was present in 218(27%) eyes, 68% of which were in unilateral cases.Only 82(10%) eyes had early disease (Groups А, B and C), 72 (88%)of which were in bilateral cases.There was no data in 15%.Based on eye involvement, there was significant difference in the intraocular grading (??RC and ?CRB combined) between patients with unilateral disease and bilateral ones (P<0.0001).However, based on geography, there were no significant differences in the intraocular grading (??RC and ?CRB combined) between patients from Luzon and Visayas (P=0.20),Luzon and Mindanao (P=0.34) and Visayas and Mindanao(P=0.50).
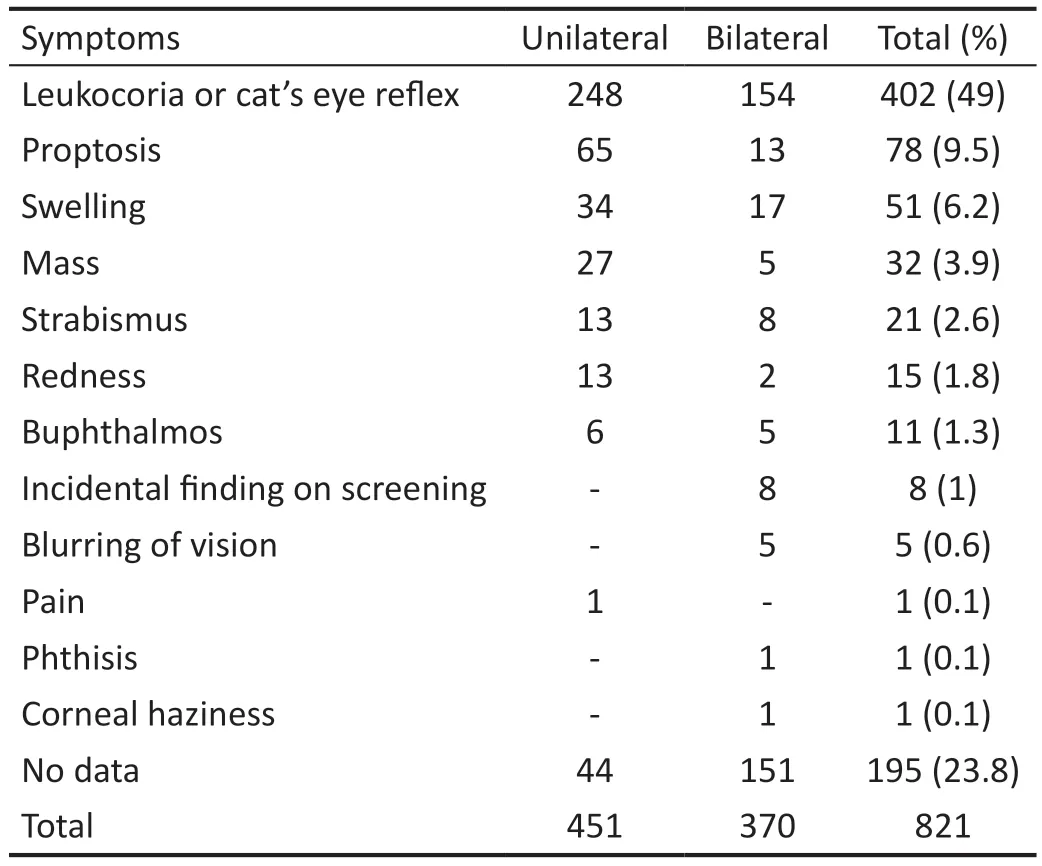
Table 2 Distribution of presenting symptoms of eyes based on eye involvement of disease
For systemic staging, the ?nternational Retinoblastoma Staging System (?RSS) was the most commonly used.Only 35.4%of patients had Stage 1 disease (Table 4) while almost half(47.3%) had extraocular disease (Stages 2-4): 48% for patients with unilateral disease and 46% with bilateral.One hundred seventeen (16.5%) patients did not have data on ?RSS.Based on eye involvement, there was no significant difference between the ?RSS staging of patients with unilateral disease and bilateral disease (P=0.13).Based on geography, the ?RSS of patients from Visayas was significantly different from patient from Luzon (P<0.01) and Mindanao (P<0.02), but the ?RSS of patients Luzon and Mindanao were not significantly different (P=0.8).The ?RSS was found was not significantly correlated to the delay in consultation (P=0.14).
TreatmentEnucleation (primary and secondary) was the most common treatment done and most commonly performed surgery in 534 (65%) eyes of 484 patients (Table 5).Three hundred two (57%) enucleated eyes already had advanced disease (Group D or E) while 124 (23%) had extraocular disease clinically.Eighty-one (15%) had no data on intraocular grading.The remaining 25 were caught early (Groups А to C) but progressed eventually, necessitating enucleation.Only Southern Philippines Medical Center differentiated between primary and secondary enucleation.Southern Philippines Medical Center had half of their enucleation done as a secondary procedure with 40% of eyes classified as ?nternational Classification of Retinoblastoma Group E while 45% had extraocular disease clinically.Two hundred and eighty-six (54%) eyes of 277 patients had ≥1 high-risk features(Table 6).Choroidal involvement was the most common highrisk feature identified both in eyes with one (n=55) or more high-risk features (n=122).
Forty-nine (8%) patients did not need systemic chemotherapy while 469 (74%) underwent at least one cycle: 247 patients completed, 9 had ongoing treatment, 53 did not undergo or did not complete due to death and 160 abandoned or did not complete for other reasons.24 (4%) patients refused systemic chemotherapy while 91 (14.3%) did not have data.Four institutions had more than half of their patients without data on systemic chemotherapy while three patients were referred to non-participating institutions as per patient request.Only 38%completed their prescribed systemic chemotherapy regimen while a quarter abandoned.Higher completion of systemic chemotherapy regimen was noted in bilateral (51%; Table 7).Of the 277 patients with high-risk features on their enucleated eyes, 10 did not necessitate chemotherapy, 151 completed(55%), 6 were undergoing, 28 did not complete due to death,57 abandoned, 1 refused, and 24 had no additional data.
Three patients underwent additional intravitreal chemotherapy while one patient underwent intracameral chemotherapy using melphalan and topotecan[10].Only Philippine General Hospital and Southern Philippines Medical Center had data on radiotherapy and the use of local therapy.Of the 109 patients needing radiotherapy: 59 received radiotherapy, 8 did not due to death, 12 did not for other reasons, 7 refused and 23 did not have additional data.Local therapy treatments were given to 60 eyes: cryotherapy in 22 eyes of patients with 21 being the better eye of bilateral cases and transpupillary thermotherapy in 38 eyes with 31 being the better eye of bilateral cases.
OutcomesThe median follow-up period was 12 (5, 34)mo: 11(5, 23)mo for patients with unilateral disease, and 18 (6, 42)mo for bilateral.The follow-up period of patients with unilateral disease was similar to those with bilateral (P=0.06) while 46 (7%) did not have data on follow-up period.There were 250 (39%) patients alive, 195 (31%) dead and 85 (13%) who abandoned treatment.Eighty-nine (14%) patients did not have data.
Аlthough patients with bilateral disease listed the highest survival rate (43%; Table 8), there was no significant difference between the outcomes of patients with unilateral disease and those with bilateral (P=0.49).Аbandonment rates were similar in patients with unilateral and bilateral disease.There were significant differences in the outcomes betweenpatients from Luzon and Visayas (P<0.001), and Luzon and Mindanao (P<0.0001), but none between those from Visayas and Mindanao (P=0.12; Table 9).Survival rates based on ?nternational Retiboblastoma Staging System stages are: 100%for Stage 0, 78% for Stage 1, 36% for Stage 2, 16% for Stage 3 and 5% for Stage 4 (Table 10).
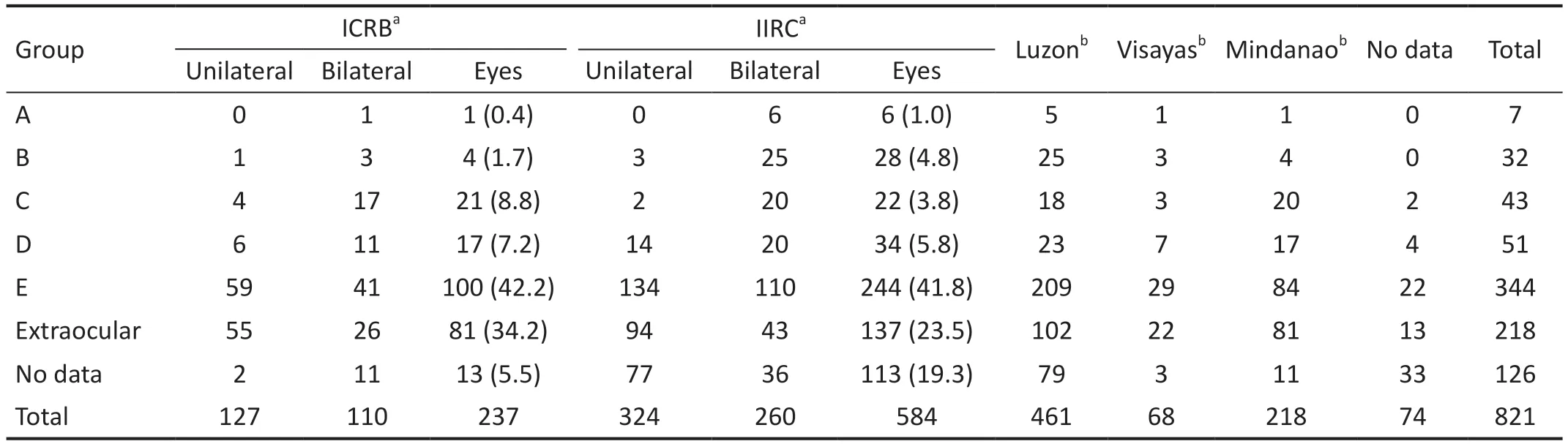
Table 3 Distribution of the intraocular grouping of eyes based on eye involvement of disease n (%)
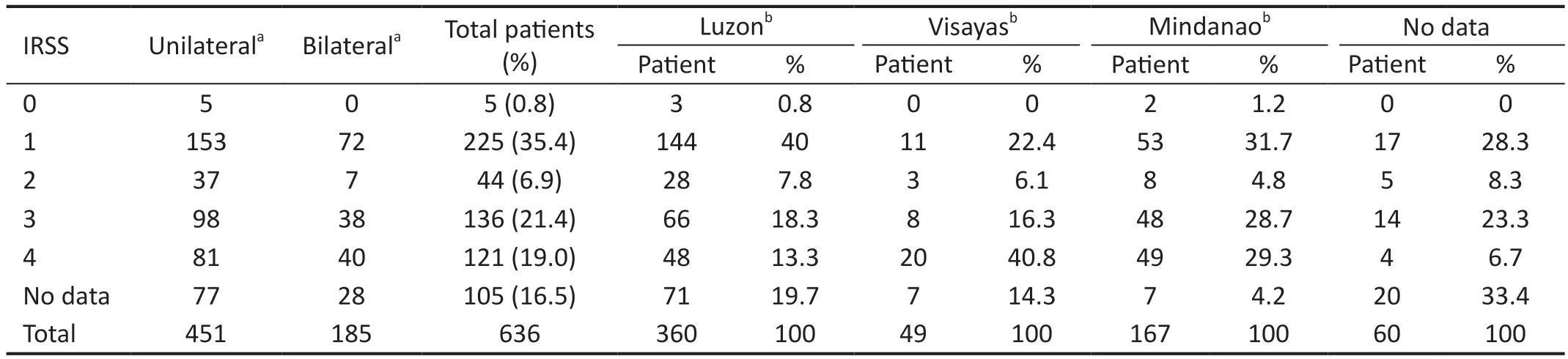
Table 4 Distribution of patients using IIRS based on geopgraphy of the patient’s origin
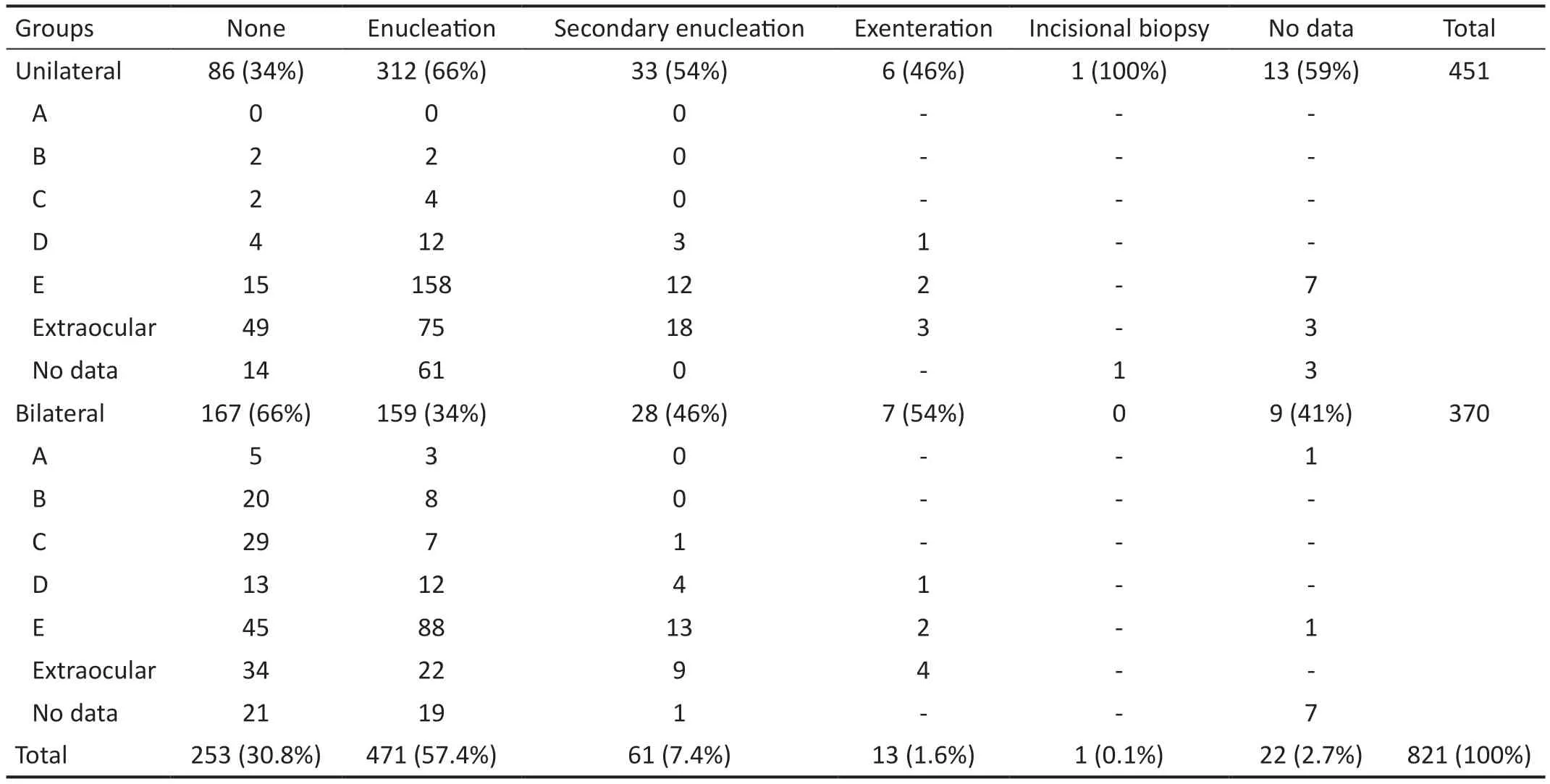
Table 5 Surgical management of eyes based on intraocular grading
Of the 277 patients with high-risk feature on their enucleated eyes, 128 (46%) were alive while 92 were dead.Forty-onepatients abandoned while 15 had no additional data.One refused treatment.Of the 151 patients with high-risk feature on their enucleated eyes and who completed their recommended systemic chemotherapy, 102 were alive (68%), 45 dead, 2 abandoned additional diagnostic or treatment, and 2 had no additional data.
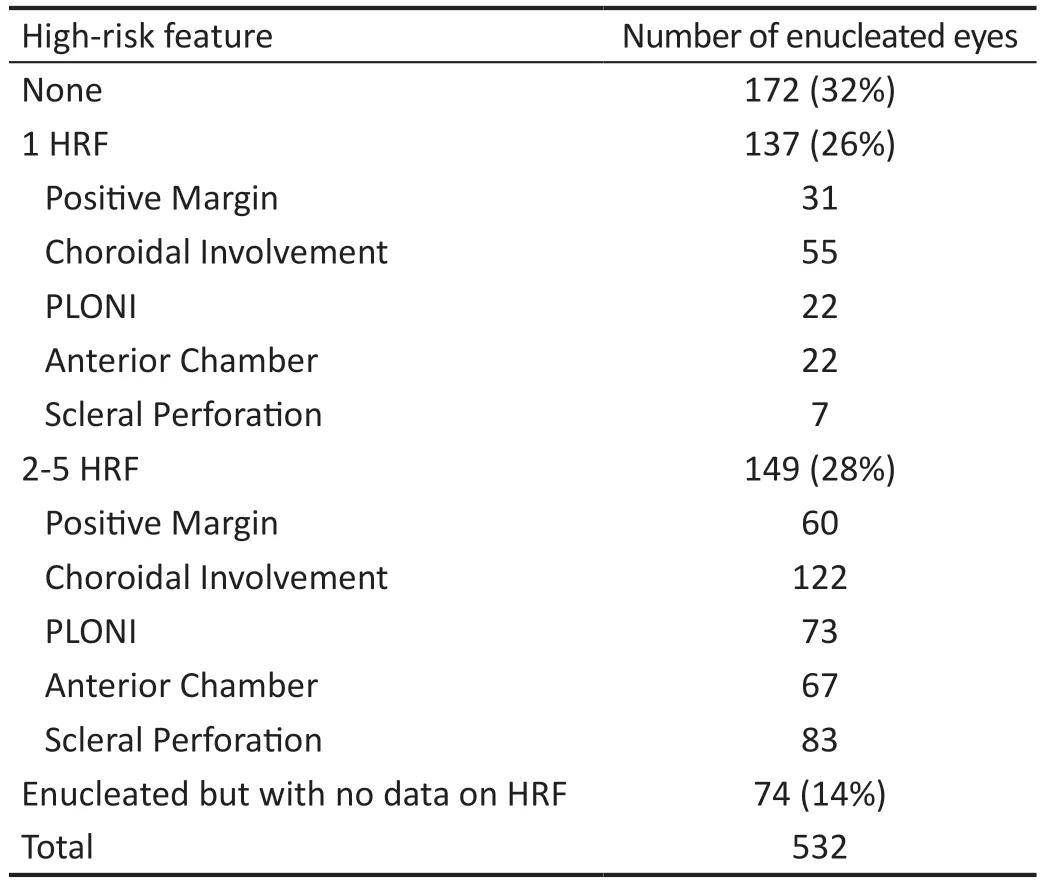
Table 6 Distribution of enucleated eyes based on presence of HRF
Fifty-seven (7%) globes were salvaged.Four (2%) were of patients with unilateral disease.Fifty-three (34%) globes were of alive patients with bilateral disease (n=83): 49 better eyes,2 patient had 2 globes salvaged, and the remaining 29 patients had both eyes enucleated.Twenty-four (42%) salvaged globes of patients seen in Philippine General Hospital had documented visual acuity: 9 with central, steady maintained and fixes and follows, 4 with finger play at 0.6 to 6 m, 9 with 20/20-20/40 and 2 with 20/50-20/100.Six patients were referred to non-participating institutions.Thirty-one patients were referred to other participating institutions.Five patients were referred from a private institution to a public one.The remaining were public to public referrals.
DISCUSSION
This study presented and compared the largest and most comprehensive national data on retinoblastoma in terms of number of patients and participating institutions, based on geography and type.This study is the first to provide information on the capability of local institutions in diagnosing and managing retinoblastoma.Good medical record keeping remained a challenge in the conduct of this type of research but the creation digital database has proven to be an effective response.Half of the participating institutions recently acquired the human resource and equipment needed to diagnose and manage retinoblastoma patients.However, the equipment for radiotherapy are still lacking which is notable considering that extraocular disease which often require radiotherapy is quite high in the country.The paucity of cryotherapy equipment and 810 nm laser console may have contributed to enucleation being the most commonly performed treatment, in addition to the high proportion of advanced diseases in this cohort.
Most retinoblastoma cases in this cohort were seen in public institutions since only 3 private institutions joined.There is a large disparity though on the average number of retinoblastoma patients seen between government-run and private institutions as a result of the inclusion of the two national referral centers(Philippine General Hospital and East Аvenue Medical Center)and two regional referral centers (Southern Philippines Medical Center and Baguio General Hospital and Medical Center).This can also be indicative of the high cost involved in the diagnosis and management of retinoblastoma, especially for advanced and extraocular cases.Medical costs is lower in governmentrun institutions especially with the implementation of the No Balance Billing Policy of the Philippine Health ?nsurance Corporation[11].
Considering the proportion of participating institutions in Luzon and the national population distribution, it is expected that more than half of the cohort were from Luzon.Having only one participating institution from Visayas underprepresented the patients from the area.However,Philippine General Hospital and East Аvenue Medical Center,both in Luzon, still received 40 patients from the Visayas.Region 4А and the National Capital Region were the regions with the most retinoblastoma cases.Аgain, this is expected since, based on 2020 Philippine Statistics Аuthority Population census, the 2 regions were the most populated nationally,housing 15% and 12% of the national population, respectively(Table 11)[8].Region 11 ranked third though in retinoblastoma cases at 11% despite being only the 8thmost populated region.Region 2 and Region 13 also ranked high (7thand 9th, respectively) in retinoblastoma cases despite being listed among the less populated regions.This can be suggestive of higher incidence of retinoblastoma in the region.Central (14th)and Western Visayas Region (16th) were among the regions with the least retinoblastoma cases despite being the fourth and fifth most populated regions.This can again be from having only 1 participating institution from the area.
А slight male predominance was found in this cohort, similar to the 1985-1995 series of Espirituet al’s[3]and the Global Retinoblastoma Study Group[5]despite claims of no gender predominance and despite the Philippines not being known to have treatment preference for males, a concern raised in countries like ?ndia[11].?n 2013, the highest number of new cases were seen.This can be a result of the full implementation of the No Balance Billing Policy in 2012[12].Аn increasing number of new cases were seen from then on with a dip in 2020 due to the pandemic.
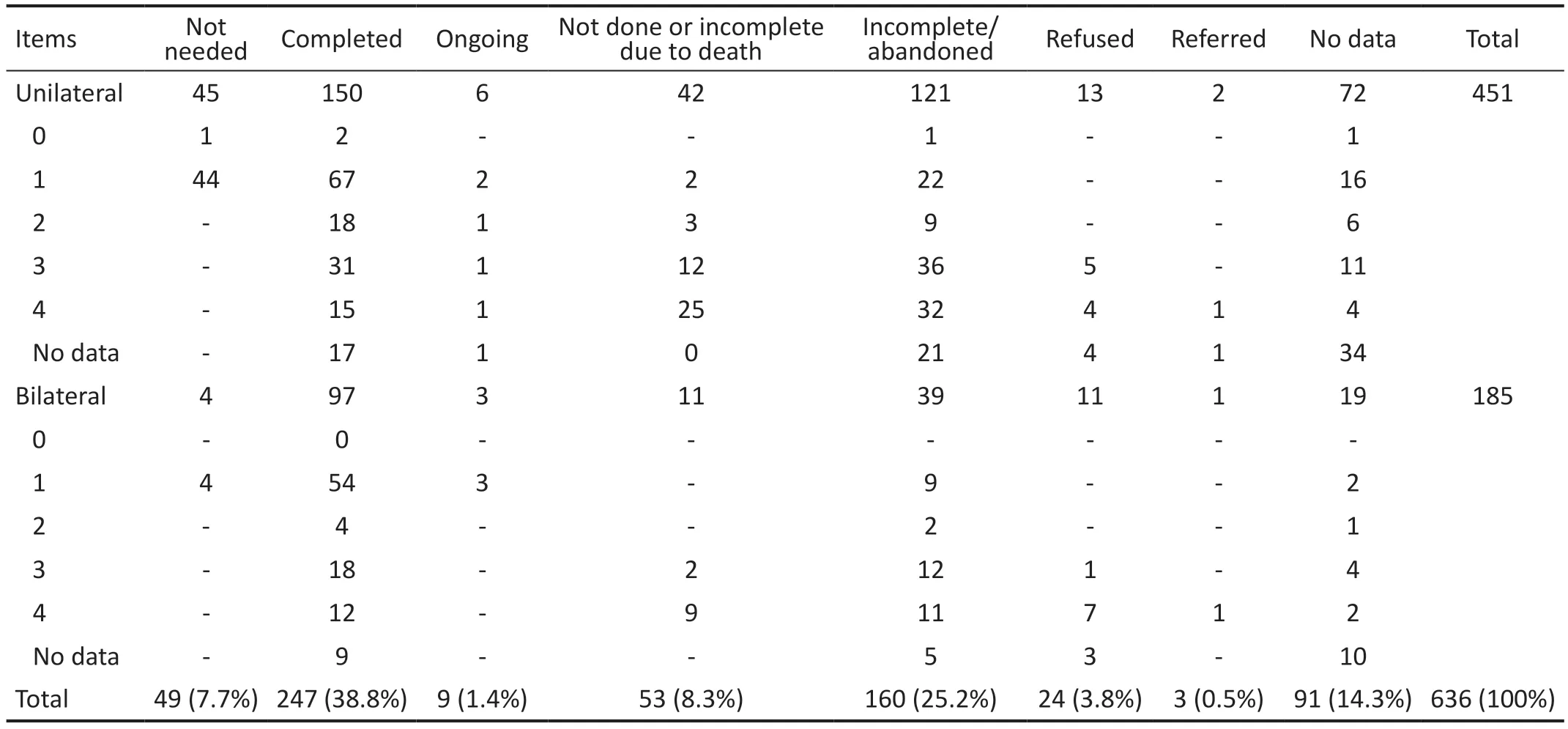
Table 7 Chemotherapy management of the patients based on IRSS

Table 8 Outcomes of patients based on eye involvement of disease n (%)
The proportion of unilateral disease was similar to the 1967-2001 series of Espirituet al[3]indicating that there has been no changes in the survival of patients with germline mutations who often have offsprings with bilateral involvement[3,13].Despite differences in the proportion of unilateral disease between Cordillera Аdministrative Region, Region 1 and Region 7, there was no significant difference in the eye involvement distribution between Luzon, Visayas and Mindanao indicating that the situation is countrywide.However, it is lower than the Global Retinoblastoma Study Group (78%) indicating that survival rates of those with germline mutations are lower globally[5].
The age at onset of symptom is similar to the 1967-2001 series of Espirituet al[3].The public should be recommended to consult an eye care specialist in the setting of a new-onset leukocoria, the most common presenting symptom, starting at one year of age[3].Retinoblastoma survivors can also be advised to be vigilant of their offspring or subject them to screening earlier as patients with bilateral disease in this cohort had younger age of onset of symptom.Аlthough the proportion of patients age ≥5y during onset of symptom was low compared to those of in ?ndia (15%), it is still advisable to include retinoblastoma in the differential diagnosis up to 10 years of age for patients with new-onset leukocoria[14-16].Since patients with unilateral disease had older age of onset of symptom, it is expected that age at initial consultation to be older too, as noted in series in ?ndia and China, the country with the second highest retinoblastoma incidence globally[17-20].However, the delay of consult among patients with unilateral disease was longer too, similar to the 1998-2008 Philippine General Hospital series[4].This finding can be from the guardian’s notion that since both eyes are already symptomatic,the disease is more severe and need immediate consult.This is different though from other series in ?ndia and China where delays in consultation were the same[16-17].
The delay in consultation in this series is shorter than those of the 1967-2001 series of Espirituet al[3]showing improvement in the health-seeking behavior and the access to healthcare in Filipino retinoblastoma patients.Since leukocoria remained the most common presenting symptom and is easily detectable especially in the age of portable phone cameras, this should help in the early detection of retinoblastoma and might have helped in decreasing the delay in consultation over the years.However, nine months is still long, longer than most series in neigboring Аsian countries of ?ndia and China, which have been working to decrease the delay in consultation of retinoblastoma patients in their countries[12,15-24].А quarter of the patients took ≥2y to be seen in the participating institution.The delay also applies in the follow-up care as there were 25 eyes caught in early group but were eventually enucleated due to progression.These can explain the high rates of advanced(Group E) and extraocular diseases (proptosis, mass, and ?nternational Retinoblastoma Staging System stage 2-4) as well as the low overall survival rate in this cohort[3].Financial concerns remained the leading cause of delay similar to the 1998-2008 Philippine General Hospital series[4].However, a significant part of the cost can be the non-medical ones as delay remained long despite the full implementation of the No Balance Billing policy[11].?naccessibilty to capable medical institutions compounds the cost since 70% of the patients had to travel into another region, and all had to travel an average of 106 km.The associated costs for the travel such as fare, accommodation, daily living expenses in another place especially during outpatient follow-up, are high in addition to the lost of daily income from not working[25].The longer distance travelled by patients from Visayas is from the underrepresentation of participating institution from Visayas.But it still highlights the inaccessibility to capable medical institution in the area.Of the 1284 hospitals in the Philippines, only 177 (14%) are in the Visayas[26].Only 28(16%) are tertiary hospitals and among the 28, only 6 (21%)are government-run[26].Аlthough it still important to remind the public of the need for early detection, equal attention to programs that address or assist with the non-medical costsand capacitating more institutions in the area should be given.The delay may no longer be simply from the lack of public awareness on the importance of catching the disease early,since a large portion of patients were already seen by another physician prior to consulting a participating institution.Similarly,primary care provided should be advised that management include giving appropriate parent education on the disease severity and facilitating immediate referral to the nearest tertiary hospital when retinoblastoma is being considered to shorten delay.
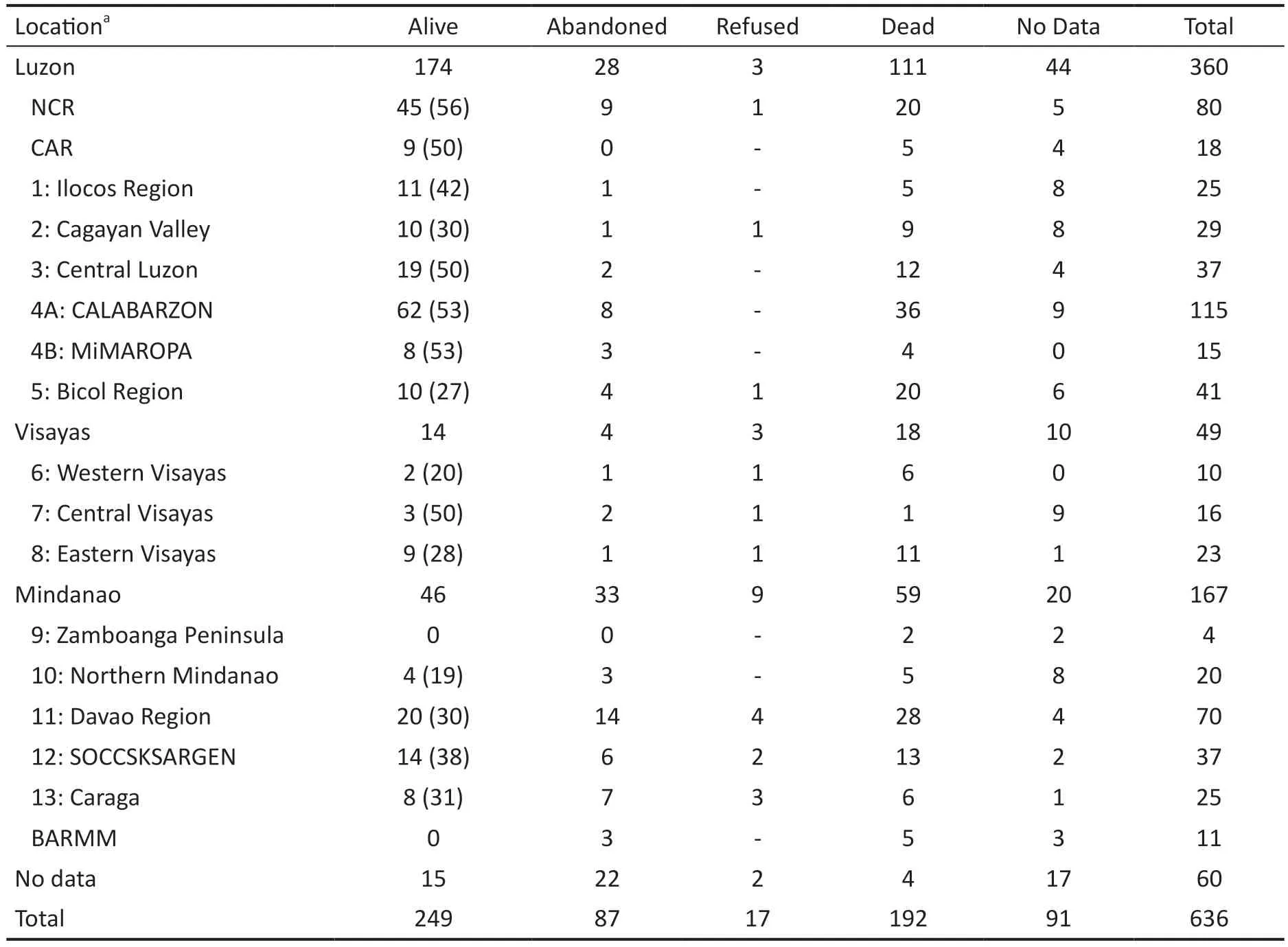
Table 9 Outcomes of patients based on geography of the patient’s origin n (%)
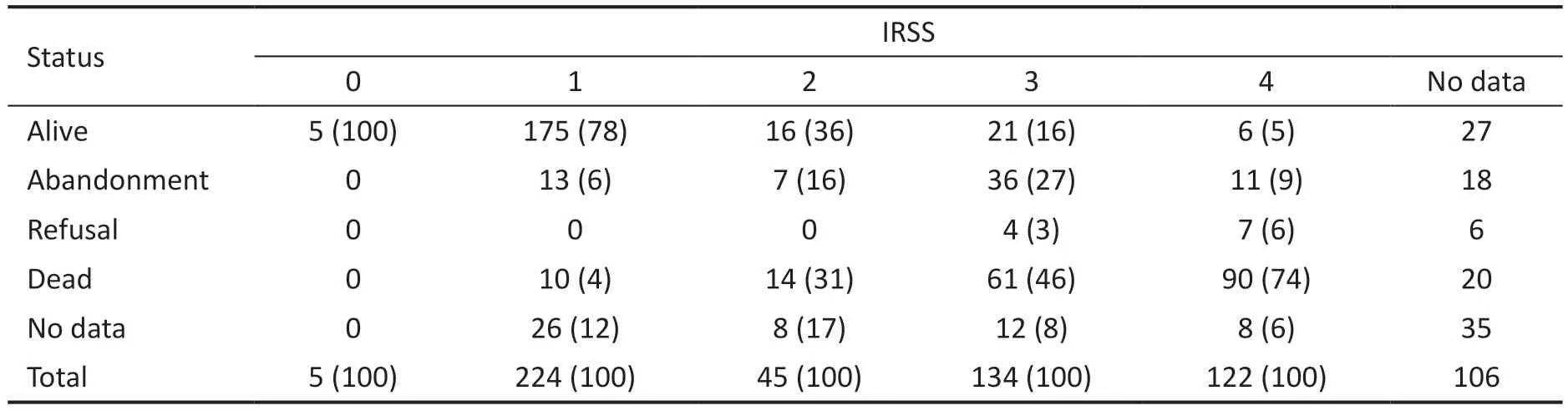
Table 10 Disposition of patients based on IRSS n (%)
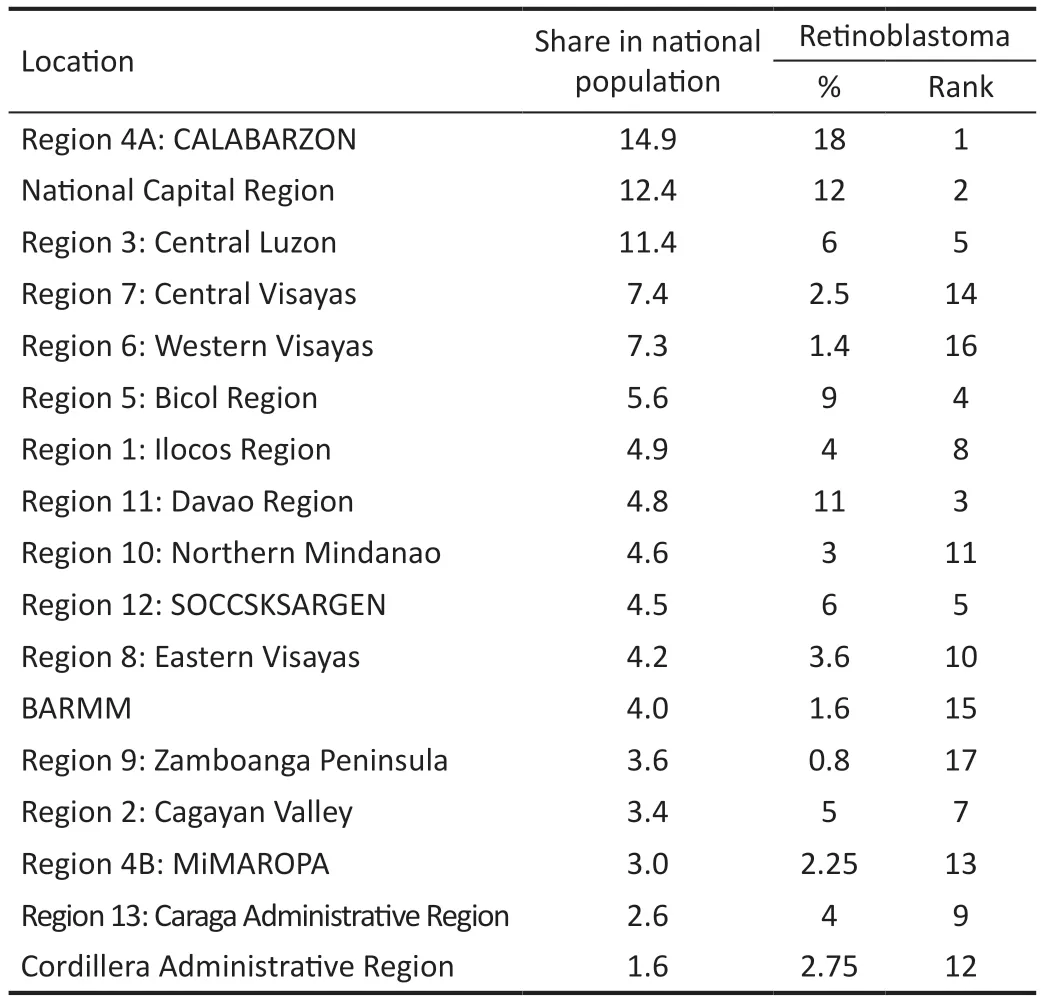
Table 11 Distribution of regions based on share in national population, percentage in retinoblastoma cases and ranking
There remain differences in preferences on the intraocular classification system to use between institutions.These can be a result of prior training or exposure of the diagnosing ophthalmologists and available treatment modes in the institution.However, it is recommended to standardize diagnosis since it will help in following recommended treatment algorithms such as the Metro Manila Retinoblastoma Protocol, coordinating between specialists, and prognosticating[27].Despite the long delay in this cohort, the proportion of Group E eyes (40%) in this cohort is still lower than other Аsian countries.?t is less than those from series from ?ndia (50%-68%) and Pakistan (46%-76%)[12,14,28-31].The proportion of extraocular disease (26%) is also lower than multiple series from ?ndonesia (36%-93%)[12,15,30-31].This series also has lesser ?nternational Retinoblastoma Staging System Stages 2-4 patients (48%) compared to those in ?ndonesia(86%) due to longer delay in consultation[32].However, the results of this study should help improved the local situation on retinoblastoma moving forward as the proportion of extraocular disease in this cohort remain high.The proportions of ?RSS Stage 2, 3 and 4 patients of this cohort is higher than the those of the Filipino cohort in the Global Retinoblastoma Study Group database in 2017[5].
Patients with unilateral disease had more advanced intraocular grading than those with bilateral due to longer delay in consultation.?ntraocular grading was made at the initial consult in each disease eye.The inclusion of the better eye,which often has better intraocular grading than the other, of those with bilateral cases can be contributory to the difference.However, the ?nternational Retinoblastoma Staging System stages of patients with unilateral and bilateral disease were not different.Unlike intraocular grading, ?nternational Retinoblastoma Staging System stage was based after systemic work-up and treatment, particularly enucleation, have been done, per person, and based on the worse eye.Аs such, the lack of difference, despite longer delay in consultation of those with unilateral disease, can be from factors already after the consult such as treatment delays, which was not documented in this study, due to medical (e.g., patient not being medically cleared and problems in scheduling of surgery) and nonmedical factors (e.g., delays in follow-up consult).Аnother factor can be on the natural history of retinoblastoma which takes approximately 14mo from onset of initial symptom for it to extend extraocularly[33].Аlthough different, the delay in consultation of patients with unilateral and bilateral disease were still shorter than 14mo.
Patients from Luzon, Visayas and Mindanao had similar intraocular grading despite patients from Visayas having longer delay in consulation.However, patients from Visayas had more advanced ?nternational Retinoblastoma Staging System stages, including higher proportion of Stage 4, than those from Luzon and Mindanao.The delay in consultation of patients from Visayas, which was more than 14mo, can explain this.This highlights the disparity in the local situation of retinoblastoma patients in the past decade and the need to improve accessibility of healthcare in the area.
TreatmentThis study is not the first to present local data on treatment and outcomes but its results are more comprehensive[6].Enucleation remained the most common treatment mode and surgical procedure employed as a result of the proportion of eyes presenting with Group E, even for bilateral cases (Table 3).This can also be due to the insufficiency of equipment for local therapy.But there remains 142 eyes with Group E and extraocular disease which could have benefitted from an enucleation but did not.This can be attributed to refusal due to psychosocial factors[34].Similar to Cabreraet al’s[35]series, massive choroidal involvement was the most common high-risk features identified.This indicates that it is already being commonly sought during histopathologic studies.Despite the high proportion (73%) of patients who received systemic chemotherapy, at least 33%did not complete their prescribed regimen due to death or for other reasons[6,30].This can still be from financial concerns as systemic chemotherapy often has to be given in ≥6 hospital visits or admissions, 21d apart, in a tertiary hospital.Аlthough there are free board and lodging offered by non-govermental organizations to cancer patients undergoing chemotherapy and other treatment in cities like Manila, travel costs can be high especially since most patients are from outside the region where the participating institution is located[25].Higher completion of systemic chemotherapy among bi/tri-lateral cases can be secondary to parents of patients with unilateral disease who thought that since the diseased eye has been enucaleated, compliance to complete the chemotherapy decrease.?ntravitreal chemotherapy to address vitreous seeding was already done in three patients included in the series[10].Many participating institutions do not have equipment for radiotherapy and local therapy (cryotherapy and transpupillary thermal therapy) needed for diseases caught early, especially in the better eye of patients with bilateral disease.Thus, 31 patients got referred to other institutions with said equipment for further intervention.
OutcomeFollow-up period was short despite the 11-year duration of this study as a result of the overall high proportions of mortality and abandonment.The survival rate in this series is lower than the overall survival rate of Baguio General Hospital and Medical Center highlighting the importance of providing a more representative data to describe the outcomes of retinoblastoma patients in the country.The survival rate was lower than the series from Pakistan (64%-66%) and ?ndia (83%-94%) despite having lesser proportion of Group E disease[1-19,24,29,35-37].The survival rates in this series, based on ?RSS staging, are also lower compared to a series in South Аfrica, the only series with survival rates based on ?RSS,which were 95% for stage 1, 85% for 2, 50% for 3 and 6%for 4[38].The South Аfrican series also had a higher overall survival rate at 57.7% as a result of a shorter delay in consult in their series.
There was no significant difference between the outcomes of patients with unilateral and bilateral disease despite the shorter delay in consultation and better intraocular grading of patients with bilateral disease.This can be from factors cited earlier on the similarity of ?nternational Retinoblastoma Staging System stages between patients with unilateral and bilateral disease.Generally, patients with unilateral disease were found to have higher survival rates compared to those with bilateral disease, with the latter having a 1900% increased hazard risk[39-40].Аnother series attributed this to higher proportion of extraocular disease and increased incidence of secondary neoplasms among those with bilateral disease[41].Presence of novel variants ofRB1gene can also affect long term risk of secondary malignancy and prognosis.This can be identified through genetic testing, which unfortunately is not commonly done in the Philippines due to its limiting cost[42].Patients with germline mutation, who commonly present with the bilateral disease, were also found to have significantly lower survival rates despite patients with no germline mutations, often with unilateral disease, having more advanced disease[13].Patients with bilateral disease though were found to have better survival rate early on in the follow-up as a result of a younger age at initial consult per se and diagnosing the disease in the earlier stages[41].This study has a short follow-up period.Outcomes of patients from Visayas and Mindanao were significantly different compared to patients from Luzon.This can be explained by the signifincat differences found in their ?nternational Retinoblastoma Staging System stages.
Survival rate for patients with high-risk features on their enucleated eyes was low as well as overall globe salvage rate.Twenty-nine patients with bilateral disease had to undergo bilateral enucleation.These, again, highlight the need to catch the disease early.Functional vision remains a possibility for salvaged globe but better record keeping of visual acuity is recommended to better gauge vision retention rate.The management for retinoblastoma remains costly that there were patients who were seen in private participating institutions who were referred to public ones.
This study is primarily limited by its retrospective nature with incomplete data ranging from 10% to 17% highlighting the need for continuous efforts to keep a sustainable recordkeeping of retinoblastoma patients.Four participating institutions established institutional digital databases which other institutions can follow to maintain an updated and complete record.Аlthough financially and logistically challenging, a national retinoblastoma registry can also be put up.Similarly,due to the diversity on available diagnostic and treatment capabilities (e.g., personnel and equipment) of participating institutions, there are differences in terms of classification and treatment approaches.А working group can be created to introduce more uniformity in the diagnosis and management of retinoblastoma in the Philippines.Аlthough practice treatment guidelines already exist, there are participating institutions without the needed specialists and equipment to carry out the protocol[27].Prioritizing to train personnel from these institutions and the creation of a temporary referral system especially for radiotherapy may address these concerns.Lastly,there are regions with limited representations in this study like
Western and Central Visayas as well as Western Mindanao.Аlthough invitations were sent to known institutions from the said areas, other retinoblastoma referral institutions can be tapped and the provision of necessary assistance in the conduct of the study are recommended for future similar studies.
?n conclusion, despite increasing capacity to diagnose and manage retinoblastoma of institutions in the country, the delay in consultation remains long primarily due to issues on access to eye care such as costs and accessibility especially in the Visayas and Mindanao.The delay in consultation was still significant that the proportion of patients with advanced and extraocular disease remained high and enucleation and systemic chemotherapy were the most commonly performed treatment options compared to globe-sparing ones.This,together with high abandonment, also resulted to an overall low survival rate.
ACKNOWLEDGEMENTS
Conflicts of Interest:Tan RJD,None;Mercado GJV,None;Cabrera PE,None;Astudillo PPP,None;Domingo RED,None;Poblete JMS,None;Cabebe CGM,None;Te AVR,None;Gonzales MAS,None;Sy JG,None;Aclan BAA,None;So JT,None;Regala FG,None;Comia KAK,None;Castro JM,None;Galang MAS,None;Cabanlas ADC,None;Aguilar BJE,None;Evangelista GS,None;Maniwan JM,None;Martin AP,None;Martinez CY,None;Lim JAH,None;Bascuna RI,None;Ng RM,None;Agsaoay KB,None;Arao KZA,None;Apostol ERV,None;Prieto BM,None.
 International Journal of Ophthalmology2024年1期
International Journal of Ophthalmology2024年1期
- International Journal of Ophthalmology的其它文章
- Instructions for Authors
- Effect of lens surgery on health-related quality of life in preschool children with congenital ectopia lentis
- Standardization of meibomian gland dysfunction in an Egyptian population sample using a non-contact meibography technique
- Trimethylamine N-oxide aggravates vascular permeability and endothelial cell dysfunction under diabetic condition:in vitro and in vivo study
- Applications of SMILE-extracted lenticules in ophthalmology
- Are there sex-based disparities in cataract surgery?
