The perceptions and experiences of advanced cancer patients and their families in advance care planning:a systematic review and synthesis of qualitative studies
Peng-Shuai Wu,Hong-Yang Liu,Meng-Ying Leng,Hai-Guang Zhao*
1Department of Plastic Surgery,Qilu Hospital of Shandong University,Qingdao 266000,China.2School of Nursing,Yanbian University,Yanji 136200,China.
Abstract Background:The goal of this study was to conduct a meta-synthesis of advanced cancer patients’and their relatives’experiences with advanced care planning(ACP)and to provide evidence-based guidance for the development and implementation of ACP in advanced cancer patients.Methods:We searched databases including China Knowledge Network,Wanfang database,VIP database,China Biomedical Literature Database,PubMed,Web of Science,Embase,Cochrane Library,and Cinahl from inception to April 2022 to collect qualitative studies on advanced cancer patients and families'experience about ACP.We use Joanna Briggs Institute Critical Appraisal Checklist for Qualitative Research to evaluate the quality of literature.After quality assessment,meta-synthesis was used to summarize and explain the results.Results:Eleven qualitative studies were included involving 29 results and ten categories.Three integrated themes were extracted:facilitators and barriers to the implementation of advanced medical care programs as perceived by patients and families with advanced cancer;attitudes of patients with advanced cancer and their families towards pre-existing medical care programs;suggestions from patients with advanced cancer and their families on the implementation elements of the pre-existing medical care program.Conclusion:ACP is a complex social process and influenced by many factors.It requires joint efforts of different stakeholders to achieve high-quality and successful ACP.
Keywords:advance care planning;cancer;experience;qualitative research;meta-synthesis
Background
The Global Cancer Statistics Report,published in 2018,shows that there are approximately 18.1 million new cancer cases and 9.6 million cancer deaths expected worldwide[1].At present,malignant tumors have a low cure rate,a high morbidity and mortality rate,and have become one of the major causes of human death.In the advanced stages of tumors,patients often have no opportunity to express their treatment wishes due to their limited decision-making capacity,suffer treatment measures that are not in accordance with their wishes,and have difficulty securing their autonomy over their lives and their choice of treatment[2,3].Family members,as the primary medical decision-making agents,usually opt for protective medical measures because they do not know whether the decisions made are in line with the patient’s interests and wishes[4].As a result,they also develop adverse emotions such as learned helplessness,guilt and anxiety.Advance care planning(ACP)is the process by which adults with decision-making capacity communicate their values and wishes about future health care with healthcare professionals,family members,and others while they are aware of them[5,6].The primary purpose of ACP is to help patients receive medical care that is consistent with their values,goals,and wishes during a severe or chronic illness[5,6].Studies have found that ACP can facilitate communication among medical staff,patients,and families;enable patients to make end-of-life care decisions consistent with their wishes;protect patients’rights to information and autonomy;and help patients’families and medical staff escape from decision-making dilemmas while helping to save social resources and reduce overmedication[7,8].ACP has been developed in western countries for many years and has been widely recognized.However,in clinical practice,65%–85%of advanced oncology patients die in the absence of ACP,and dignity and comfort at the end of life cannot be guaranteed[9,10].
For patients with advanced tumors,it is difficult to improve their cure rate in the short term,and overtreatment instead decreases patients’quality of life.Therefore,understanding the experiences and feelings of advanced cancer patients and family members participating in ACP can help patients and family members establish a common understanding,increase awareness of ACP,respect patients’values and preferences,and thus improve the quality of services for advanced cancer patients.This study utilizes a meta-synthesis approach to conduct a systematic review of the existing literature to explore the feelings and experiences of advanced cancer patients and their families participating in ACP and to provide information to improve the quality of life of this group.
Study design
Search strategy
To gather information on the participation of patients with advanced cancer or their family members in ACP experiences,computer searches of five foreign language databases,PubMed,CINAHL,Web of Science,Embase,and The Cochrane Library,and four Chinese databases,China Biomedical Literature Database,China Knowledge Network,Wanfang,and VIP database,were conducted.The search was conducted using subject terms combined with free terms,and the search time frame was from the establishment of the database to April 2022.References in published reviews were also retrospectively searched manually to avoid missing relevant literature.Cancer,carcino*,leukemia*,tumor*,malignan*,lymphoma*,metastat*,sarcoma*,oncolog*;advance care planning,ACP,advance directive*;qualitative,narrative,phenomenolog*,grounded theory.Chinese search terms include:癌癥,腫瘤(cancer,tumor);患者,家屬(patient,relative);預(yù)立醫(yī)療照護(hù)計(jì)劃,預(yù)前照護(hù)計(jì),生前預(yù)囑,預(yù)先指示,預(yù)立自主計(jì)劃(advance care planning,advance directive).This systematic review was pre-registered in the PROSPERO Registry(CRD42022325488).
Inclusion and Exclusion Criteria
P(participant)study subjects
Patients or their family members who clinicians clearly diagnosed as having advanced cancer(stage IV),or although patients with different diseases were involved,the number of patients with advanced oncology was more than 50%,and the study subjects were required to have participated in ACP,where family members refer to spouses,children,siblings and other caregivers.For studies that explored the experiences of patients or family members and the experiences of other people,only data about patients’or family members’perspectives or experiences were analyzed.
I(interest of phenomenon)
Investigate phenomena of interest:the experiences,experiences,and feelings of advanced cancer patients or family members who have participated in ACP.
Co(Context)research scenarios
Patients or family members who have participated in ACP initiated or led by a third-party initiated or guided ACP communication(including meetings,guidelines,manuals,ACP-specific intervention programs).
S(Study plan)study type
Qualitative studies,mixed-methods studies,or qualitative data from quantitative studies.Only qualitative data was included for mixed-methods studies or qualitative data in quantitative studies.Exclusion criteria:1.Studies that only explored the acceptance of ACP,the development or application of tools to implement the ACP process,etc.,without substantive implementation of ACP.2.Duplicate published studies.3.Literature with inaccessible full text or incomplete data.4.literature not in Chinese or English.
Study selection and data extraction
Two researchers trained in text entry read the retrieved literature,independently screened and extracted information based on inclusion and exclusion criteria,and cross-checked.In the case of disagreement,discussion and analysis or consultation with experts in the relevant fields were used to make judgments.Literature screening was performed by first excluding duplicate literature,then reading the titles and abstracts to exclude literature that did not match the study topic,and then further reading the full text to determine the final literature to be included in this study.The data extraction had author(year),country,aim,setting,participants,methods,and findings(themes).
Appraisal of methodological quality
The methodological quality of the included studies was independently evaluated by two researchers trained in evidence-based methodology,using the Joanna Briggs Institute qualitative research quality evaluation criteria[11].The evaluation consisted of 10 entries,focusing on the consistency between the philosophical view of the study,the methodology and the interpretation of the results,the researcher’s influence on the study,the typicality of the study population,and the ethical norms.Each item was evaluated as“yes”,“no”,“unclear”,and“not applicable”.A grade of A was assigned for fully meeting the above criteria with minimal possibility of bias;a grade of B was assigned for partially meeting the above quality criteria with a moderate possibility of bias;and a grade of C was assigned for not meeting the above quality criteria with a high possibility of bias.After independent evaluation of the quality of the literature,the screening and evaluation results of the two individuals were compared.Disagreements were discussed,and consensus was reached between the two individuals,or a third researcher was invited to arbitrate and decide whether to include or not.Finally,studies with quality grades A and B were included,and studies with quality grade C were excluded.
Data synthesis
The integrative method used in this study is convergent meta-integration(aggregative-synthesis),which is philosophically based on pragmatism and a priori phenomenology[12].Among the integrative methods of qualitative research,this method is the most transparent,emphasizing the need for the researcher to avoidreinterpreting the included literature and to present the results of the included studies exactly as the original authors intended,making it suitable for synthesis of evidence from various types of qualitative research in different fields.A researcher familiar with the philosophical ideas and other theories and methods of qualitative research extracts the findings(the original authors’analysis and interpretation of the data)word by word by repeatedly reading the included studies with the corresponding supporting information(participants’words,field observations,etc.)in the original text,and then summarizes the similar findings into generalized categories,further integrating them by analyzing the internal and external connections between the categories and results to obtain new interpretations.In this study,Nvivo 12 Plus was used to free-code the text of the results and conclusion sections of the included literature on the experiences of patients with advanced cancer and their families participating in advance care planning,line by line.Three researchers independently completed the data extraction and coding process and upon completion,discussed their respective extracted data with each other in an effort to achieve consistency.
Results
Results of literature search and screening
A preliminary search of 2,268 relevant literature was conducted,and 11 studies were finally included,as shown in Figure 1.
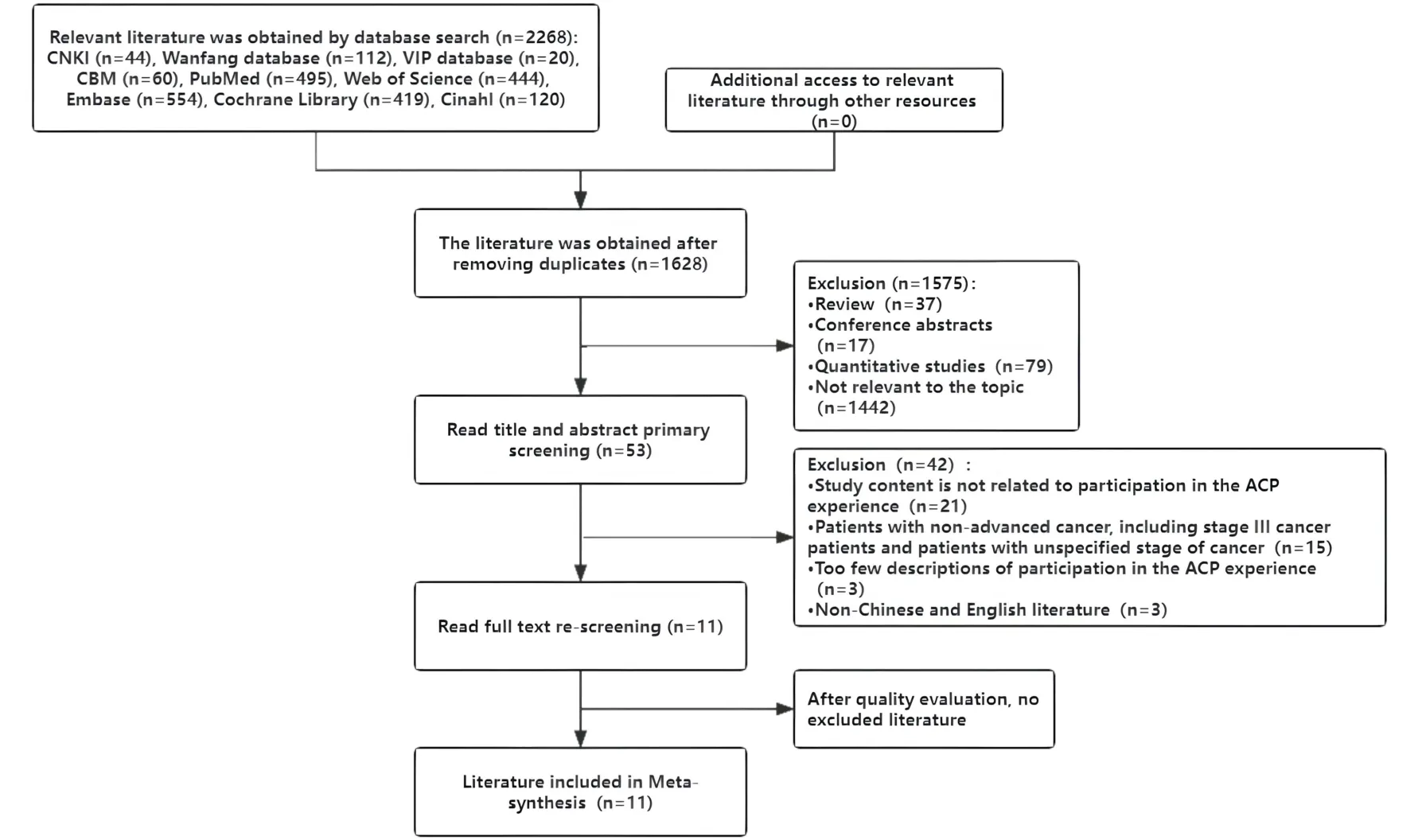
Figure 1 Literature selection process
Quality evaluation of included studies
The results of the quality evaluation showed that 3 of the 11 included studies were rated A and 8 studies were rated B.The studies obtained after screening were included,as shown in Table 1.
Basic characteristics of the included studies
The initial search yielded 1,062 relevant papers,and 11 were finally included;the basic characteristics of the included papers are shown in Table 2.
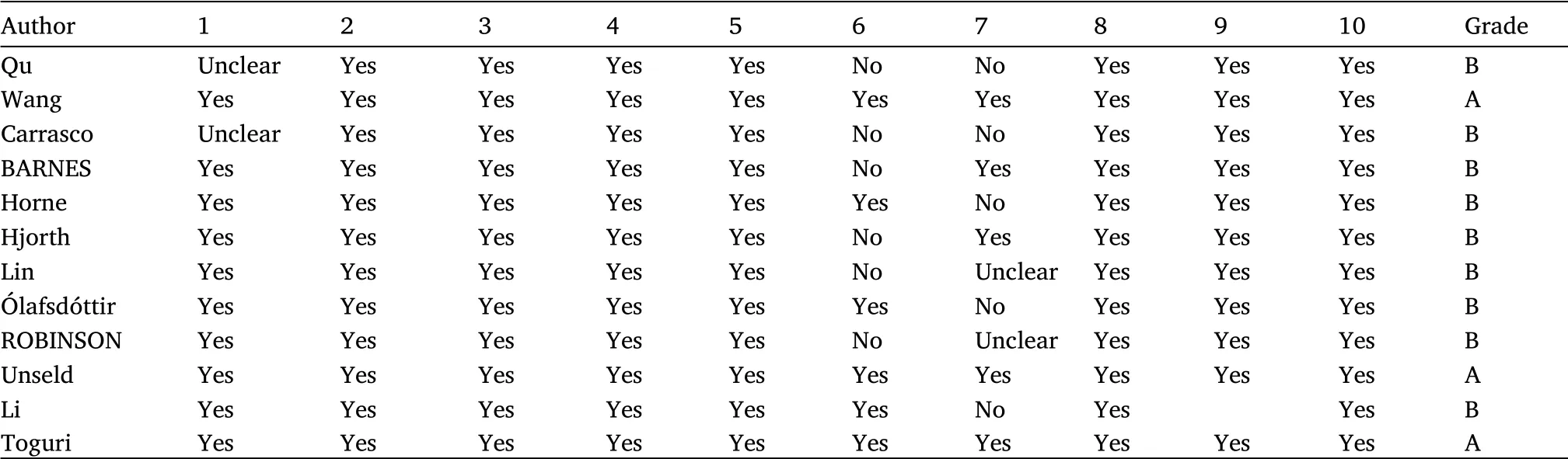
Table 1 Quality evaluation of included studies
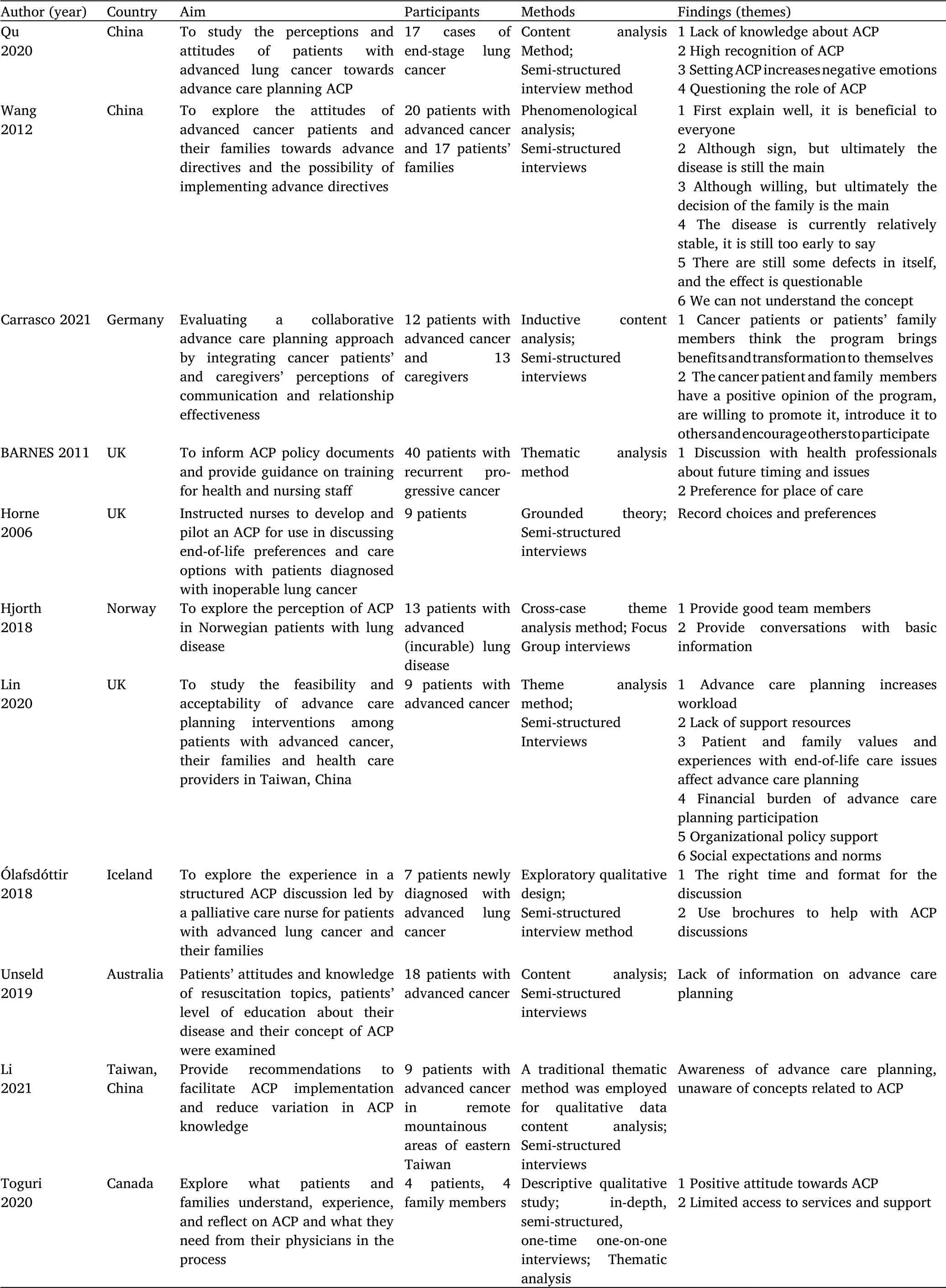
Table 2 Basic characteristics of the included studies
Meta-synthesis results
Synthesis I.Facilitators and barriers to implementing advanced medical care programs as perceived by patients and families with
advanced cancer.
Facilitating factors for implementing pre-existing medical care programs as perceived by patients and families with advanced cancer.Some cancer patients and families had positive comments about the ACP and were willing to promote and introduce it to others,encouraging others to participate(“everything will be done the way you want it to be done;this is important to me and what I need;I would definitely recommend this to others”)[13].Patient and family values and experiences with end-of-life care issues influence the implementation of ACP,and having experience caring for patients with cancer can make them more willing to participate in ACP discussions(“people who have cared for patients with cancer will have a better understanding of the dilemmas and related issues that patients may experience during their disease trajectory,and they will be more willing to come to ACP consultations”)[14].Implementing ACP interventions in clinical care requires policy support at the organizational level,which is necessary to make ACP possible(“can ACP be part of routine hospital care?I think it really depends on the hospital’s policy support”)[14].
Obstacles to implementing pre-existing medical care programs as perceived by advanced cancer patients and families.Clinical situation constraints require additional effort to embed ACP in clinical practice,increasing the workload of medical staff.Workload has increased as a result of advanced care planning(“we are already busy with our daily routines,and now I have to spend more time implementing ACP”)[14].Lack of adequate resources is a barrier to implementing ACP(“I think all of the reasons we were unable to implement ACP were because we lacked the manpower and resources to do so”)[14].Cancer patients and families do not feel they have access to the services and support they need to have ongoing discussions about prognosis and future care(“no access to ongoing services”)[15].Patients and families felt that ACP would increase their financial burden because they would have to pay for each ACP consultation.(“ACP allows providers to learn more about what patients want.However,nothing happens if patients can’t afford it”)[14].The public takes medical care services for granted and should be paid for by national health insurance.Patients and families are reluctant to pay the out-of-pocket costs of advance care planning consultations.There is a high incidence of surrogate decision-making by the health care team,resulting in a lower willingness of patients to participate in ACP discussions(“patients are used to a health care delivery system with no additional costs and trust the health care team to make the best decisions for them”)[14].Most patients reported a lack of knowledge about the ACP and could not understand the concept(“I didn’t know what a pre-established medical care plan was,so I didn’t set one up either”)[16].The medical staff did not explain very clearly(“I consulted with them during my previous hospitalization,and they did not explain very clearly,so I did not have a deep understanding of this”)[17].There is a misconception about ACP:“I feel that if a pre-established medical care plan is set up,it is as if the treatment is abandoned,so will it be possible to resuscitate without resuscitation?”[18].
Synthesis II.Attitudes of patients with advanced cancer and their families towards pre-existing medical care programs.
Some patients and family members had a high level of acceptance of the ACP and expressed willingness to discuss and sign it.The majority of patients and family members who participated in the study considered the ACP important and expressed willingness to go to discussions about the patient’s end-of-life care and decision-making(“I think the ACP is good for him;otherwise,everyone will just guess what he wants”.)[16].Some family members considered discussing the ACP as a form of self-protection because knowing the patient’s preferences before making decisions can reduce the emotional burden(“I know it is his wish and it gives me inner peace”)[19].Some patients and their families fully affirm the role and benefits that ACP brings to them.The ACP was considered essential and thought-provoking(“It made me think deeply about what is important to me”)[13].Willingness to discuss,believing that ACP is thought-provoking to think about end-of-life issues and make plans(“ACP discussion is thought-provoking,and I am willing to think about this and then make plans”)[15].
Some patients and families are reluctant to accept the ACP and do not see the need to sign it.Some patients are not ready(“I know these thoughts are in here somewhere(pointing to head),but I’ve always pushed them away since I was diagnosed.I don’t know if I’m ready to face them or if I feel uncomfortable)[16].Living in the moment and trying not to think about it(“I choose not to think ahead and would rather live each day”)[19].Immature ACP management processes,signed ACP documents not being enforced,relatives witnessing and then affecting acceptance of ACP(“I lost my sister in Canberra,and she signed a lot of documents,no more CPR,etc.,but the hospital didn’t have them,so they kept resuscitating her”)[16].
Some patients indicated that although they were willing to try to discuss and sign,ultimately it was the condition or the family’s decision(“No,I don’t want to make a specific decision yet,I want to wait for...”)[19].
Synthesis III.Suggestions from patients with advanced cancer and their families on the implementation elements of the pre-existing medical care program.
Timing of the discussion.There was more controversy about the timing of the discussion,with some patients saying that it was too early for ACP but that they would talk to their doctor more often if their condition worsened.If the doctor told me,“l(fā)ook...it’s coming back”...if that’s the case,then I think I would say,“Now let’s plan this”)[20].Some patients felt that this should be done as early as possible(“otherwise it would be too late to benefit”)[21].Some patients felt that they needed to choose the right time to discuss this and that having enough time to discuss these issues was an important factor(“doctors are busy,so I didn't talk to them because I think it is a rather long topic”)[20].
Discussion format.Decision aids such as manuals or videos were helpful in implementing ACP,and it was relatively natural for medical staff to introduce ACP(“at least I think this manual is perfect for this discussion;it fits what we are talking about”)[21].Communication between families was also more accessible(“I want my family to read this manual(crying),I just want to take it and say to my family,I want everyone to read this together”.)[21].
Location of care.Most said they wanted to be cared for at home for as long as possible(“If I had a choice,I would rather stay at home and be in a familiar place”)[20].Some patients also said that receiving care at home would be a burden on their families(“it is good to be cared for at home at first,but if you do that,you can put a lot of stress on people”)[20].
People involved.Physicians,nurses,or other health care teams should be involved in the ACP,and in particular,there are certain qualities that nurses possess that are more appropriate(“there are not many people who can discuss this topic,really not many.Nurses understand my situation and can help me ask questions.Nurses are approachable and compassionate,all of which help discuss end-of-life issues”)[22].Family members play an important role in maintaining treatment decisions,and family involvement is expected(“If there are decisions to be made and the doctor really doesn’t know which is in your best interest,family involvement in the discussion can be a good solution to that problem”)[22].
Documentation.Patients were generally more receptive to having their wishes documented in writing or recorded(“I feel much better;it’s clearer for everyone;if it’s written down,everyone knows where it is and you can express your wishes yourself”)[23].However,there were also cases where patients’attitudes toward medical choices at a later stage were not consistent with the content of the documents signed earlier because of the inadequate discussion process of the ACP and the patient’s poor understanding of end-of-life options(“I don’t remember having an ACP.My wishes were to use morphine if the disease was severe and to‘let go and go’”).Yet the patient had an ACP documented and in the record asked the physician to decide whether to take maintenance treatment”)[22].Some patients felt that the documentation of the record was of little significance and that what was important was that the family already knew the patient’s wishesafter the discussion process(“the ACP record documentation was useless,it was just that I thought I should have it and my only thought was that legally it would be better to have one because the family already knows what I think”)[23].
Discussion
Gradually increasing advanced cancer patients’and their families’knowledge of ACP and assisting them in increasing their acceptance
The discussion of ACP may require a process of acceptance by patients and their families.Paying attention to the changing attitudes of advanced cancer patients and their families toward ACP and increasing their acceptance of participating in ACP are essential prerequisites for the smooth development of ACP.In the early stages of the disease,patients want to maintain a positive attitude and believe that it is too early to discuss this issue[20].Still,they also realize the importance of these topics,which have planted a seed in the patients’minds and need to be reminded at the right time;for example,when there is a change in the disease or when the current treatment plan is not working[24].Some studies have shown that medical staff is reluctant and hesitant to open ACP discussions,and they are influenced by the social climate and unit culture[25,26].Therefore,the positive effect of ACP on patients and their families should be affirmed,and ACP discussions should not undermine patients’hopes[27].More importantly,the development of ACP can help patients and their families think about and discover what is most important at the end of life and thus choose medical care that is consistent with their values[28].
Reducing barriers to advanced cancer patients and their families participating in ACP and encouraging advanced cancer patients to express their preferences
Interventionists should establish a good relationship with patients with advanced cancer,maintain a sincere,open,and positive attitude in ACP communication,and keep the atmosphere of the conversation relaxed[29].However,the interventionist needs to remain neutral,allow the patient to express freely,be able to detect changes in the patient’s mood,and will enable the patient to end the conversation when appropriate.Using techniques such as scenario simulation techniques to make the patient feel that it is just a hypothesis eliminates the patient’s fear and repression and opens these topics more easily[30,31].
Conclusion
In this study,the meta-synthesis of qualitative research was used to explore the experiences of advanced cancer patients and their families in participating in ACP and to gain insight into the problems of advanced cancer patients in facing death,facing future medical care options,and discussing the process.The cooperation among patients with advanced cancer,their families,and health care professionals should be strengthened to overcome the difficulties of participation in ACP for patients with advanced cancer in many aspects and to enrich the content and form of ACP participation for the development and improvement of ACP.
- Cancer Advances的其它文章
- Advancing oncology nursing practice:a vital and changing role
- Research progression on immunotherapy biomarkers of peripheral blood in non-small-cell lung cancer
- Advances in the exploration of adjuvant therapy of colon cancer with Chinese medicine
- Research progress of uremic myopenia in traditional Chinese and western medicine
- Effect of Chinese herbal medicine on lung disease:an updated review
- Primary mucinous carcinoma of the thyroid:case report and review of the literature

