COVID-19 presentation as acute pancreatitis: A case report
Abhyuday Kumar, A. Valiyaparambath, Neeraj Kumar, Amarjeet Kumar, Ajeet Kumar
1Department of Anaesthesiology, AIIMS Patna, Bihar, India, 801505
2Departments of Trauma & Emergency, AIIMS Patna, Bihar, India, 801505
ABSTRACT Rationale: The gastrointestinal manifestations of COVID-19 include anorexia, nausea, vomiting, abdominal pain, and diarrhea. However,pancreatitis as the presentation of COVID-19 is rarely reported.Patient’s Concern: A 63-year-old COVID-19 patient presented with complaints of abdominal pain and difficulty breathing for 5 d.Diagnosis: Contrast-enhanced computed tomography of the abdomen suggested acute interstitial pancreatitis without any biliary tract obstruction.Interventions: The patient was resuscitated with intravenous fluids based on dynamic parameters of fluid responsiveness. The patient was started on enteral feeding, analgesics, antibiotics,dexamethasone, low molecular weight heparin, and supportive therapy.Outcomes: The patient developed severe acute respiratory distress syndrome and died 6 days after admission.Lessons: Management of COVID-19 in the presence of pancreatitis is challenging. Adequate early fluid resuscitation is an important aspect of medical management for COVID-19 patients with pancreatitis and restrictive strategies must be followed. Increased liver enzymes and renal dysfunction in acute pancreatitis can also limit the use of specific therapies like remdesivir. Dexamethasone,even though it has shown a benefciial effect in treating COVID-19,can have an additive effect in causing hyperglycemia in these cases. Clinicians should be aware of this atypical presentation of COVID-19 with pancreatitis and adjust their management strategies,keeping in mind the considerations for both diseases.
KEYWORDS: Pancreatitis; COVID-19; APACHE II; Remdesivir;Fluid
1. Introduction
COVID-19 commonly manifests as respiratory symptoms but may present with gastrointestinal symptoms. The gastrointestinal manifestations of COVID-19 include anorexia, nausea, vomiting,abdominal pain, and diarrhea. However, pancreatitis as the presentation of COVID-19 is rarely reported. Here we report a case of COVID-19 presenting as acute pancreatitis.
2. Case report
Informed written consent was obtained from the patient’s relative.The relative of the patient has given his consent for images and other clinical information to be reported.
A 63-year-old man, whose RT-PCR test was positive for SARSCoV-2 virus and without any comorbidities, complained of abdominal pain and difficulty breathing for 5 d when visiting the emergency room. The pain was epigastric and was associated with nausea and vomiting.
The patient did not have any history of alcohol consumption,hypertriglyceridemia, hypercalcemia, smoking, gallstone, or abdominal surgeries. The patient’s vitals and blood pressure were low with a respiratory rate of 30/min (normal: 10-20/min). Oxygen saturation was maintained through anasal cannula. The abdomen was non-distended but tender.
Bilirubin, liver enzymes, serum amylase, serum lipase, and inflammatory markers of the patient were elevated (Table 1).The ultrasound of the abdomen showed mild ascites with abulky pancreas. The contrast-enhanced computed tomography (CT) of the abdomen was suggestive of acute interstitial pancreatitis without any biliary tract obstruction (Figure 1A). Bilateral ground-glass opacity and consolidation were seen in lung parenchyma with a CT severity score of 12 (Figure 1B). APACHE II score at admission was 10.
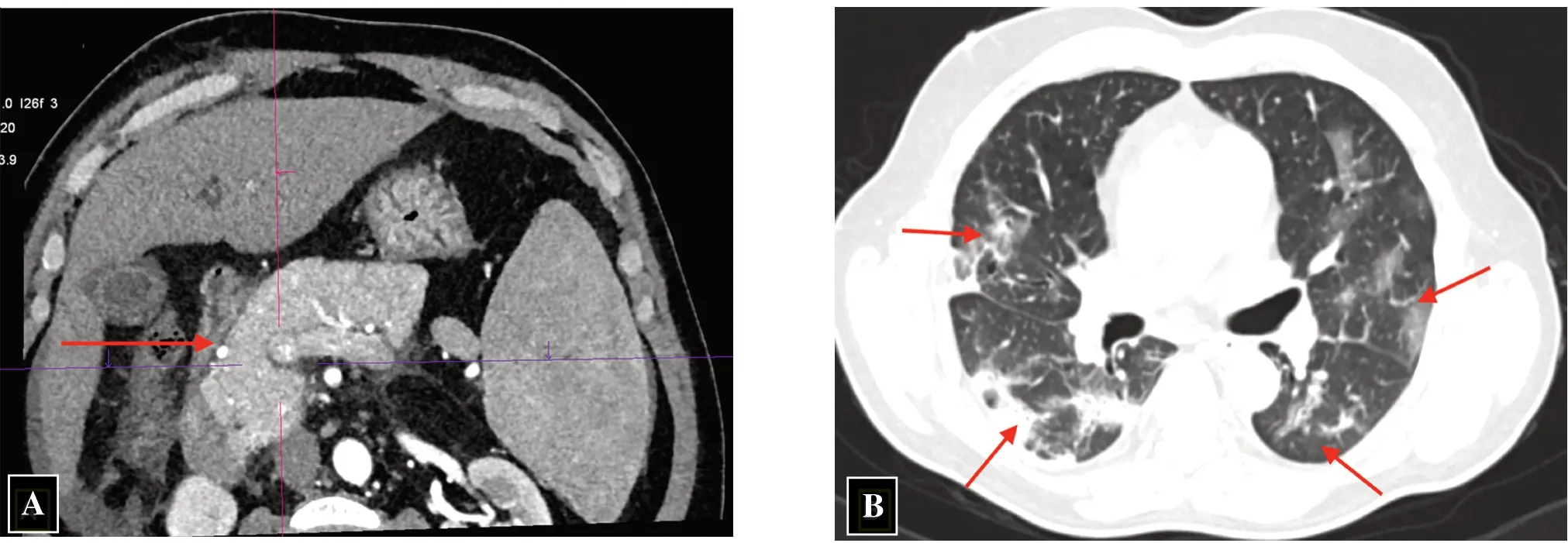
Figure 1. The CT images of a 63-year-old COVID-19 patient with pancreatitis. (A) Mild diffusely enlarged pancreas with peripancreatic fat stranding (red arrow), suggestive of acute interstitial pancreatitis. (B) Multifocal patches of discrete and confluent ground glass opacities and consolidation within apicobasal and anteroposterior gradient in bilateral lung parenchyma (red arrows).
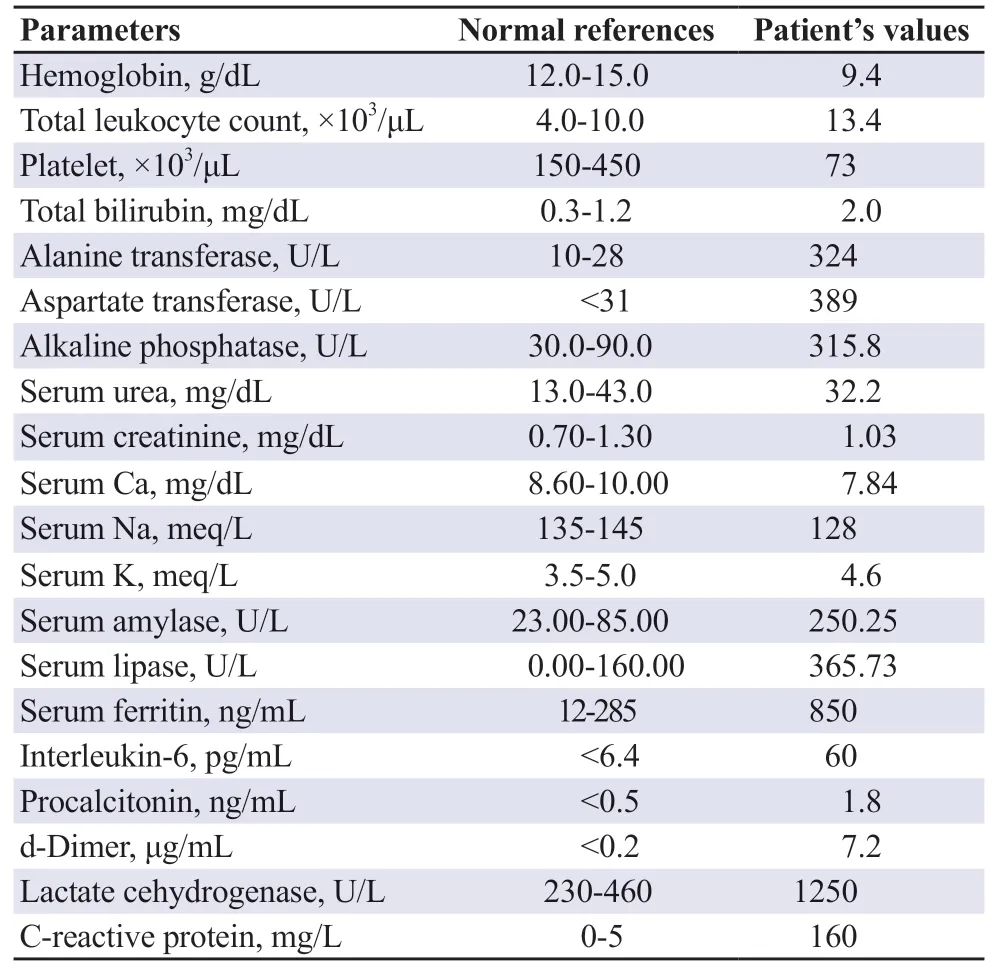
Table 1. Blood parameters of the patient with pancreatitis.
The patient was resuscitated with intravenous fluids based on dynamic parameters of fluid responsiveness, and was started on enteral feeding, analgesics, antibiotics, dexamethasone, low weightheparin, and supportive therapy. However, the patient’s oxygen requirement increased in due course, and he was put on invasive mechanical ventilation on the 3rd day. He developed severe acute respiratory distress syndrome and died on the 6th day of admission.
3. Discussion
Biliary stones and alcohol overuse are the most common causes of acute pancreatitis comprising 70%-80% of cases[1]. Other causes include trauma, surgical manipulations, and metabolic derangements.Acute inflammation of the pancreas has been reported in infections caused by human immunodeficiency virus, mumps, cytomegalovirus,coxsackievirus B, and influenza A (H1N1) Epstein-Barr virus[2]. In SARS-CoV infection (2003), the virus was detected in the lungs,liver, kidneys, intestine, and pancreas, indicating that the pancreas is a potential coronaviral target[3]. The pathogenesis of COVID-19 is mediated by angiotensin-converting enzyme-2 (ACE-2) receptors on cells. As ACE-2 receptors are highly expressed in pancreatic islets, this may be the reason for acute pancreatitis in our case[4].A case series of 52 COVID-19 patients reported that pancreatic injury was present in 17% of patients[5]. However, the pancreatic injury was induced by modestly elevated pancreatic enzyme levels and acute pancreatitis was not present in these cases. Increased C-reactive protein level of >150 mg/dL and APACHE score ≥8 is suggestive of severe disease. Associated acute pancreatitis along with COVID-19 may be the reason for the rapid deterioration of our patient. Management of COVID-19 in the presence of pancreatitis is challenging. Adequate early fluid resuscitation is an important aspect of medical management, reducing organ failure, and in-hospital mortality in acute pancreatitis. Increased liver enzymes and renal dysfunction in acute pancreatitis can also limit the use of specific therapies like remdesivir. Hyperglycaemia is a common finding in pancreatitis mainly in severe diseases. Dexamethasone, even though it has shown a beneficial effect in treating COVID-19, can have an additive effect in causing hyperglycemia in these cases. Clinicians should be aware of this atypical presentation of COVID-19 with pancreatitis and adjust their management strategies, keeping in mind the considerations for both diseases..
Conflict of interest statement
The authors report no conflict of interest.
Funding
This study received no extramural funding.
Authors'contributions
A.K., A.V.P., N.K., A.K., and A.K. all contributed to the concept and design of the study, clinical studies, preparation, editing and review of the manuscript. In addition, A.K. and A.V.P. defined the intellectual content, performed literature search, and acquired data.
 Journal of Acute Disease2022年5期
Journal of Acute Disease2022年5期
- Journal of Acute Disease的其它文章
- Congestive heart failure masquerading as acute abdomen: A case report
- Symmetrical peripheral gangrene triggered by Escherichia coli sepsis
- Successful management of depression skull fracture in a boy with dog bite injury: A case report
- Effect of pH, lactate, electrolyte, and strong ion difference variability on prediction of intensive care unit mortality: A retrospective study
- Effectiveness of ChAdOx1 nCoV-19 coronavius vaccine in preventing severe disease and mortality during the second wave of pandemic: A case-case analysis from a tertiary care center in South India
- Comparative efficacy of ketamine, lidocaine, acetaminophen, and dexmedetomidine combined with morphine patient-controlled analgesia in treating opium-addicted patients undergoing tibia fracture surgery: A randomized clinical trial
