Contrast-enhanced ultrasound manifestations of synchronous combined hepatocellular-cholangiocarcinoma and hepatocellular carcinoma:A case report
lNTRODUCTlON
Liver cancer is predicted to be the sixth most commonly diagnosed cancer and the fourth leading cause of cancer death worldwide in 2018[1]. Approximately half of primary liver cancers exhibit multifocal origins[2]. According to different origins, multifocal liver cancer can be divided into primary liver cancer with intrahepatic metastasis and liver cancer with a multicentric origin[3,4].Synchronous combined hepatocellular-cholangiocarcinoma (CHC) and hepatocellular carcinoma (HCC) is rare in multicentric liver cancer, and it is often misdiagnosed as multiple HCC and has a poor prognosis[5,6].Moreover, the treatment strategies and outcomes of the two diseases are different. When CHC and HCC occur synchronously, due to the unique fiber components of intrahepatic cholangiocarcinoma (ICC)contained in CHC, treatments typically used for multiple HCC,transcatheterial arterial chemoembolization (TACE) and chemotherapy, provide limited benefits[6]. Therefore, an accurate preoperative diagnosis is very important.
CASE PRESENTATlON
Chief complaints
A 69-year-old female referred to our hospital due to months of epigastric pain and anorexia.
He mustered11 his strength and climbed to the top, and there he found a giant tree whose foot kept firm the wrinkled earth, and whose crest12 touched the very heaven
History of present illness
Epigastric pain and anorexia were presented. No nausea, vomiting, acid regurgitation, belching, chills,fever, hematemesis, melena or jaundice (among other symptoms) were observed.
History of past illness
The patient had a 20-years history of chronic hepatitis B and did not receive standardized treatments.
Personal and family history
The patient had a > 20-year history of alcoholism (approximately 50 mL liquorday) and did not have a smoking history, nor did she have a travel history to pastoral areas or epidemic areas.
Physical examination
The patient's height and weight were 155 cm and 59 kg, respectively, with a body mass index of 24.6 kg/m2. No swollen lymph nodes were found. The abdomen was soft without rebound tenderness, and the liver and spleen were not palpable under the ribs. There was no percussion pain in the liver area.Mobility dullness was negative, and bowel sounds were normal.
Finally spring burst into glorious green and Reuben s spirits erupted. The time had come! He ran into the barn, climbed to the hayloft and uncovered the tin can. He poured the coins out and began to count.
I ve always loved this place , she said, it has a lot of memories for me, and for others. We all used it. They called it Lovers lane . It s not much of a lane, and it doesn t go anywhere important, but that s why we all came here. To be away from people, to be by ourselves she added.
Laboratory examinations
Platelet count:93 × 10/L; white blood cell count:2.65 × 10/L; red blood cell count:3.99 × 10/L;hemoglobin:124 g/L; albumin:42.2 g/L (normal range:40.0-55.0 g/L); globulin:23.1 g/L (normal range:20.0-40.0 g/L); total bilirubin:10.3 μmol/L (normal range:5.0-28.0 μmol/L); direct bilirubin:3.4 μmol/L (normal range:< 8.8 μmol/L); alanine aminotransferase (ALT):50 IU/L (normal range:< 40.0 IU/L); aspartate aminotransferase (AST):61 IU/L (normal range:< 35.0 IU/L); alkaline phosphatase(ALP):126 IU/L (normal range:50.0-135.0 IU/L); hepatitis B surface antigen (+); hepatitis B e antibody(+); hepatitis B core antibody (+); hepatitis C antibody (-); HBV DNA level:6.32 × 10IU/Ml (normal range:< 1.0 × 10IU/mL); Serum bio-marker analysis showed elevated alpha-fetoprotein (AFP):219.00 ng/mL (normal range:< 7 ng/mL), serum carbohydrate antigen 19-9 (CA19-9):38.40 U/mL (normal range:< 30 U/mL) and protein induced by vitamin K absence or antagonist-II (PIVKA-II):54.00 mAU/mL (normal range:6.0-32.5 mAU/mL); carcinoembryonic antigen (CEA) and serum carbohydrate antigen 125 (CA-125) were both normal.
Imaging examinations
FlNAL DlAGNOSlS
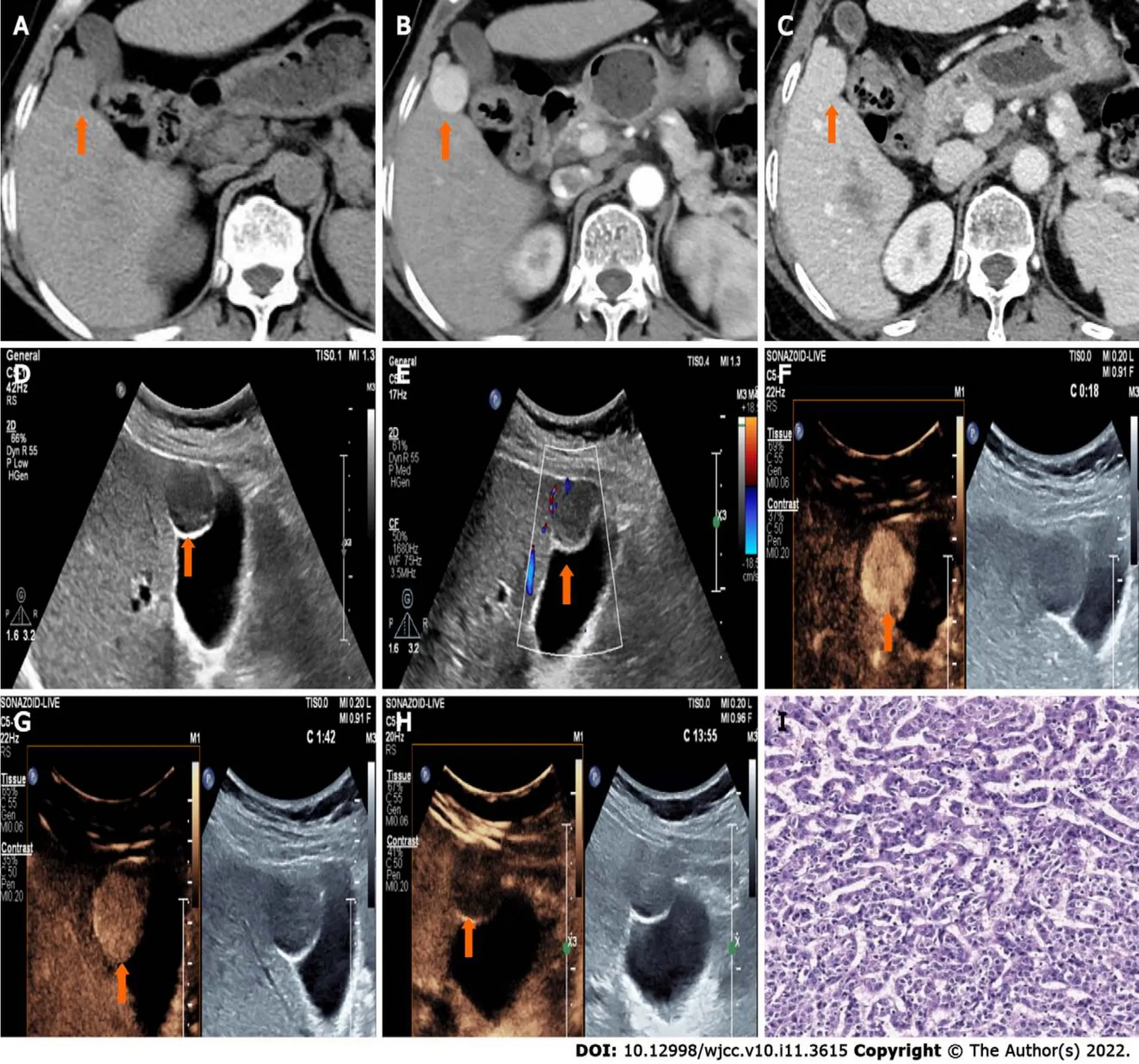
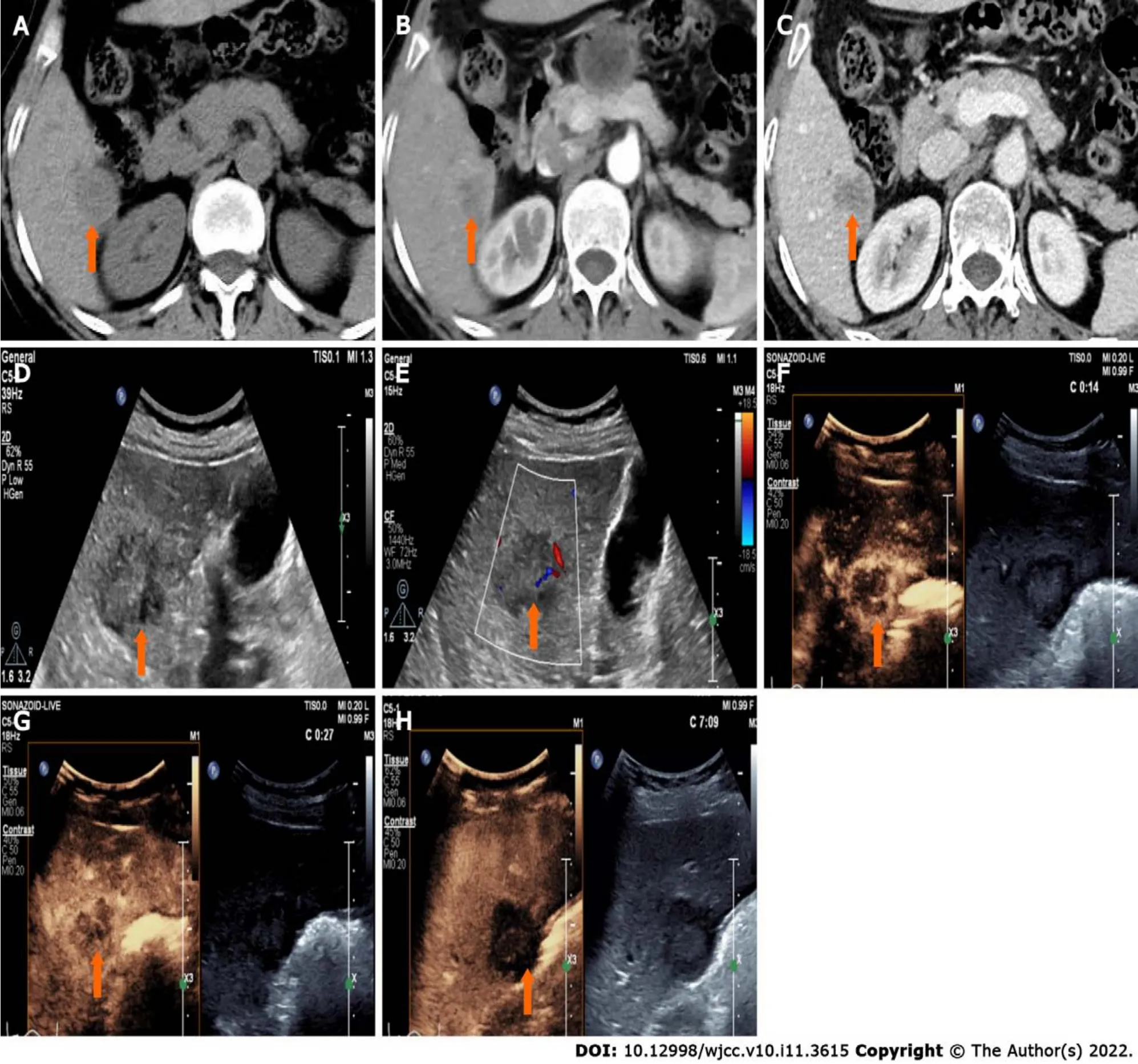
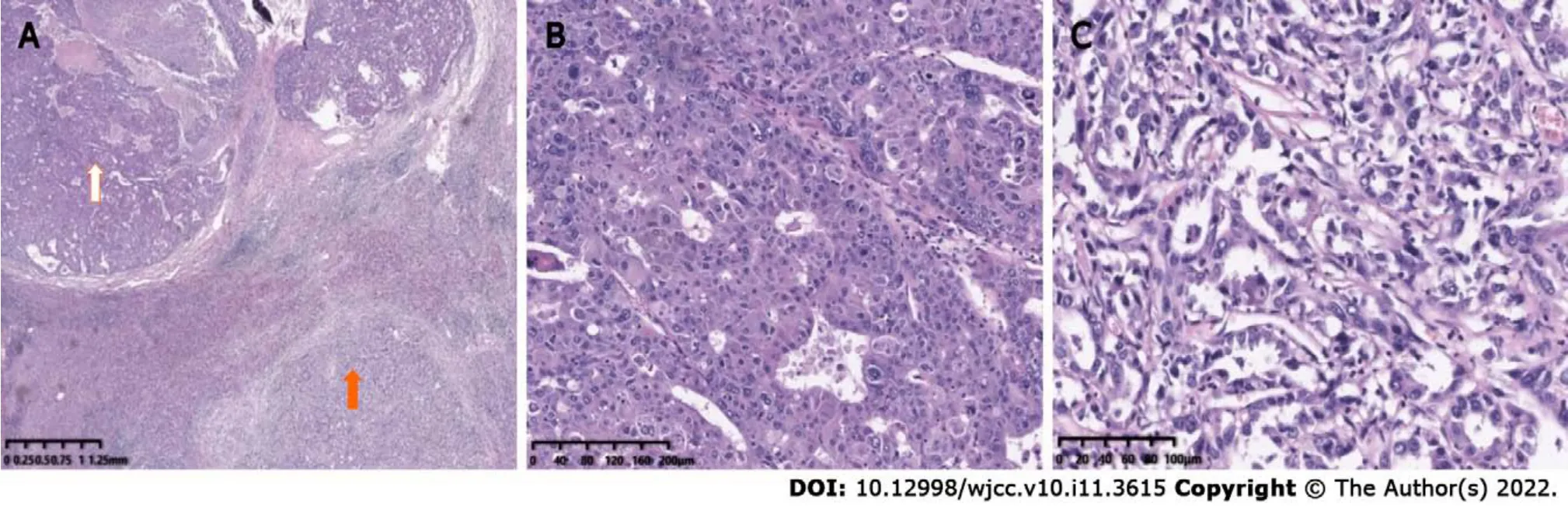
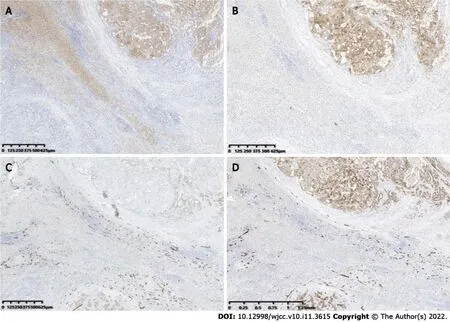
Postoperative pathology confirmed the S4 nodule a HCC (Figure 1I) and the S6 nodule a CHC(Figure 3). As to the S6 lesion, positive expression of Arginase 1 (Arg 1) (Figure 4A) and Glypican-3(GPC-3) (Figure 4B) in the hepatocellular carcinoma component, and Cytokeratin 7 (CK7) (Figure 4C)and Cytokeratin 19 (CK19) (Figure 4D) in the cholangiolocarcinoma components were confirmed by immunohistochemical analysis. No metastasis was found in the gallbladder or in the right adrenal gland.
There were other horses and their infants on our ranch10, and Sprite sometimes watched them, on one of her forced outings into the field, with a look of longing11. Then she would sigh, a long, plaintive12 snort, slowly turn her head away and refuse to look until we delivered her back to her stable.
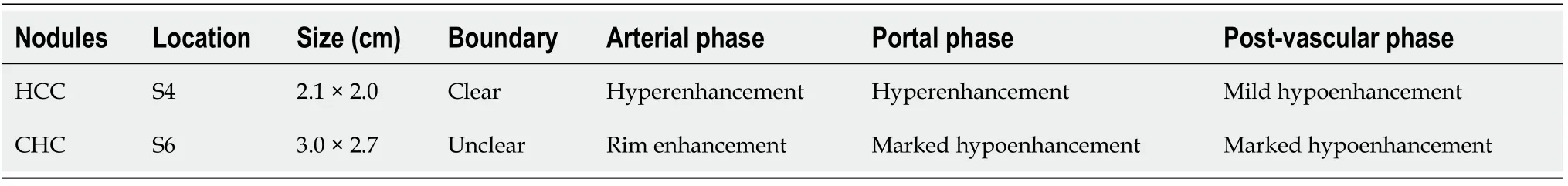
Although the CEUS features of CHC partially overlap with those of HCC and ICC, CHC still possesses its own clinical characteristics. HCC usually occurs in patients with chronic hepatitis B or cirrhosis. On CEUS images, rapid arterial phase hyperenhancement (APHE) resulted from the formation of neoangiogenesis, and washout during postarterial phases due to reduced or absent of normal structure of portal triads, are identified as characterics of HCC[12]. According to the criteria of CEUS LIRADS V2017 and related research[13,14], typical HCC is characterized by APHE (in whole or in part,not rim or peripheral discontinuous globular enhancement) with mild and late washout (> 60 s). Rimlike hyperenhancement, early (< 60 s) washout and marked washout within 120 s are specific enhancement patterns of ICC on CEUS. Arterial rim hyperenhancement pattern of ICC is associated with a high degree of malignant cell proliferation in the periphery while necrosis or fibrosis in the center of the tumor on pathology[15,16]. The ultrasound manifestations of CHC are related to the proportion of HCC and ICC components in the mass. The enhancement pattern of HCC-dominant lesions is similar to that of HCC, whereas those of ICC-dominant lesions is similar to that of ICC. The amount of the HCC component may be the main determinant of radiologic LI-RADS categories of hepatocellular-cholangiocarcinoma; tumors of LR-4 or LR-5 categories were associated with a larger proportion of the HCC component and smaller or none proportion of the cholangiocarcinomas component[17]. According to the CEUS LI-RADS criteria, most CHCs are diagnosed as LR-M, and studies have showed that the disease-free survival rate of these patients is low[18-20]. The enhancement pattern of CHC on CEUS is also associated with nodule size. When the nodule is smaller than or equal to 3 cm, the enhancement pattern is similar to that of HCC; when the nodule is larger than 3 cm, the enhancement mode is similar to that of ICC. With an increase in lesion diameter, the manifestations of CHC in enhanced images change from HCC-like to ICC-like[21]. On CECT, CHC commonly shows central delayed enhancement in the delayed phase, whereas it shows marked washout on CEUS images. This heterogeneity rarely appears in HCC, which is helpful in distinguishing between the two entities. In our case, the S4 nodule showed rapid and hyperenhancement in the arterial phase followed by mild and late washout in the delayed phase, a typical manifestation of CEUS LR-5 category. The S6 nodule displayed peripheral rimlike hyperenhancement in the arterial phase,followed by early washout,which should be classified as a LR-M nodule. Both of the nodules were differ in enhancement pattern, and onset and degree of washout. The discrepancy between the simultaneously elevated level of AFP and CA19-9 and the CEUS patterns (, the CEUS mode of ICC presents upon the increase in AFP and the CEUS mode of HCC presents upon the increase in CA19-9) have been reported to be the diagnostic criteria that can improve the accurate diagnostic rate of CHC[22]. Although some of the previously described features can help us distinguish CHC from HCC, accurate diagnosis of some cases remained tough before operations.Alternatively, ultrasound-guided puncture biopsy is necessary in such circumstances.
TREATMENT
The patient underwent a complex liver cancer resection, cholecystectomy and partial resection of the right adrenal gland.
And when the King had ridden off she took the little shirts and went into the wood, and the reel showed her the way. The children, who saw someone coming in the distance, thought it was their dear father coming to them, and sprang to meet him very joyfully. Then she threw over each one a little shirt, which when it had touched their bodies changed them into swans,21 and they flew away over the forest. The Queen went home quite satisfied, and thought she had got rid of her step-children; but the girl had not run to meet her with her brothers, and she knew nothing of her.
OUTCOME AND FOLLOW-UP
Postoperative pathology
Synchronous CHC and HCC.
Examination results
In summary, the CEUS manifestations of HCC and CHC are different. CEUS combined with clinical information (history of chronic hepatitis B and the synchronously elevated level of AFP and CA19-9)may indicate synchronous CHC and HCC, which help in effective diagnosis, clinical decision-making and better prognosis.
Gao L reviewed the literature and drafted the article; Lu Q conceived the article; Lu Q and Huang JY provided critical revision to the manuscript; Lu ZJ contributed pathological data; and all authors issued final approval for the version to be submit.

DlSCUSSlON
Synchronous CHC and HCC is an uncommon condition that very few literatures had reported previously. Though rarely occurs, this disorder typically has a poor prognosis. Because of overlapping imaging features with HCC and atypical clinical manifestation, effective diagnosis of this disease can be challenging[6]. Patients afflicted with synchronous CHC and HCC has little or no response to therapeutic drugs due to unique fiber components of ICC in CHC. Therefore, a series of local treatments, including TACE and chemotherapy, cannot significantly benefit these patients[6]. Previous studies showed that the survival rate of patients with CHC, who underwent liver transplantation showed inferior survival in comparison to those with HCC alone, and the role and indications of liver transplantation in combined tumor have yet to be defined[7-9]. Therefore, surgery is currently the best treatment choice, but the prognosis is poor due to a high incidence of vascular invasion and lymph node metastasis; additionally, the average relapse time after radical resection is only 5.4 mo[10,11]. Thus, an accurate preoperative diagnosis is of great significance for clinical decision-making and good prognosis.
Vicki and Cindy replied that they had closed their eyes and run down the hill, holding hands, in the opposite direction from Edward. And what did you do? my mother asked me.
CONCLUSlON
The patient underwent follow-up examinations at 7 mo after the operation. A newly found liver lesion located in S1 showing internal hypoenhancement and mild peripheral hyperenhancement was detected by contrast-enhanced computed tomography (CECT) (Figure 5A). The lesion manifested peripherial hyperenhancement (Figure 5B) in the arterial phase followed by early washout in the portal venous phase (Figure 5C) on CEUS. Both CECT and CEUS considered this lesion a malignancy.
CT showed a slightly enlarged spleen. S4 showed a hypoattenuating mass (Figure 1A) (approximately 2.1 cm × 2.0 cm), which presented with marked enhancement in the arterial phase (Figure 1B) and isoenhancement in the portal venous phase (Figure 1C). S6 revealed a hypoattenuating mass (Figure 2A)(an area of approximately 3.0 cm × 2.7 cm), which presented with an annular weak enhancement in the arterial phase (Figure 2B) and mild hypoenhancement in the portal venous phase (Figure 2C). The diagnosis was considered to be cirrhosis with a malignant tumor of the liver. Ultrasound indicated that the liver parenchyma was thickened and uneven. A quasicircular hypoechoic nodule with a size of approximately 2.1 cm × 2.0 cm was found in S4 alongside the gallbladder (Figure 1D); it had a clear boundary and a regular shape and pushed and squeezed the gallbladder. The gallbladder wall was continuous and complete, and a mild blood flow signal was observed inside of the nodule (Figure 1E).S6 indicated a hypoechoic nodule with a size of approximately 3.9 cm × 3.5 cm (Figure 2D), with an irregular shape and an unclear boundary. The nodule protruded outward and pushed and squeezed the right kidney. The capsule of the right kidney was intact. Additionally, short-line blood flow signals could be observed inside of the nodule (Figure 2E). No enlarged lymph nodes were found in the abdominal cavity. On contrast-enhanced ultrasound (CEUS) (Sonazoid 0.6 mL bolus injection, Philips EPIQ7, and C5-1 convex array probe), the S4 nodule showed rapid hyperenhancement in the arterial phase (Figure 1F), mild hyperenhancement in the portal venous phase (Figure 1G) and mild hypoenhancement in the post vascular phase (Figure 1H). The S6 nodule indicated rim hyperenhancement in the arterial phase (Figure 2F); in addition, washing out began in the late arterial phase (27 s) (Figure 2G),the portal phase showed hypoenhancement, and the post vascular phase showed marked hypoenhancement (Figure 2H). The ultrasound suggested liver cirrhosis; additionally, the S4 hypoechoic nodule was considered to be HCC, and the S6 hypoechoic nodule was considered to be a malignant liver tumor (the ultrasound manifestations of the two intrahepatic nodules are shown in Table 1).
The King grew as white as a sheet when he heard the Prince s story, and said, Woe19 is me, my son! The time has come when we must part, and with a heavy heart he told the Prince what had happened at the time of his birth
Informed written consent was obtained from the patient’s daughter for publication of this report and any accompanying images.
The authors declare that they have no conflict of interest.
The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See:https://creativecommons.org/Licenses/by-nc/4.0/
China
Ling Gao 0000-0003-3683-2207; Jia-Yan Huang 0000-0002-1918-2874; Zi-Jian Lu 0000-0001-9660-9002;Qiang Lu 0000-0002-4057-1997.
Fan JR
A
Fan JR
 World Journal of Clinical Cases2022年11期
World Journal of Clinical Cases2022年11期
- World Journal of Clinical Cases的其它文章
- Pleomorphic adenoma of the left lacrimal gland recurred and transformed into myoepithelial carcinoma after multiple operations:A case report
- Thyrotoxicosis after a massive levothyroxine ingestion:A case report
- Papillary thyroid microcarcinoma with contralateral lymphatic skip metastasis and breast cancer:A case report
- Del(5q) and inv(3) in myelodysplastic syndrome:A rare case report
- Ultrasound-guided local ethanol injection for fertility-preserving cervical pregnancy accompanied by fetal heartbeat:Two case reports
- Successful apatinib treatment for advanced clear cell renal carcinoma as a first-line palliative treatment:A case report
