Neuroendocrine tumour of the descending part of the duodenum complicated with schwannoma:A case report
lNTRODUCTlON
Neuroendocrine tumours(NETs)are rare tumours originating from neuroendocrine cells that account for approximately 2% of all malignant tumours,and approximately 50.6% of NETs are found in the digestive system;duodenal NETs are extremely rare,accounting for only 2%-3% of gastrointestinal NETs[1].Schwannoma is a benign tumour originating from the nerve fibre sheath,accounting for approximately 5% of all soft tissue tumours;it is mostly located in the body surface and auditory nerve,less often in the digestive tract,and even more rarely in the duodenum[2].
There was no conversation. Their soggy sandals left marks upon the hearthstone. I served them cocoa and toast with jam to fortify7 against the chill outside. Then I went back to the kitchen and started again on my household budget.
CASE PRESENTATlON
Chief complaints
One month of nausea and vomiting.
History of present illness
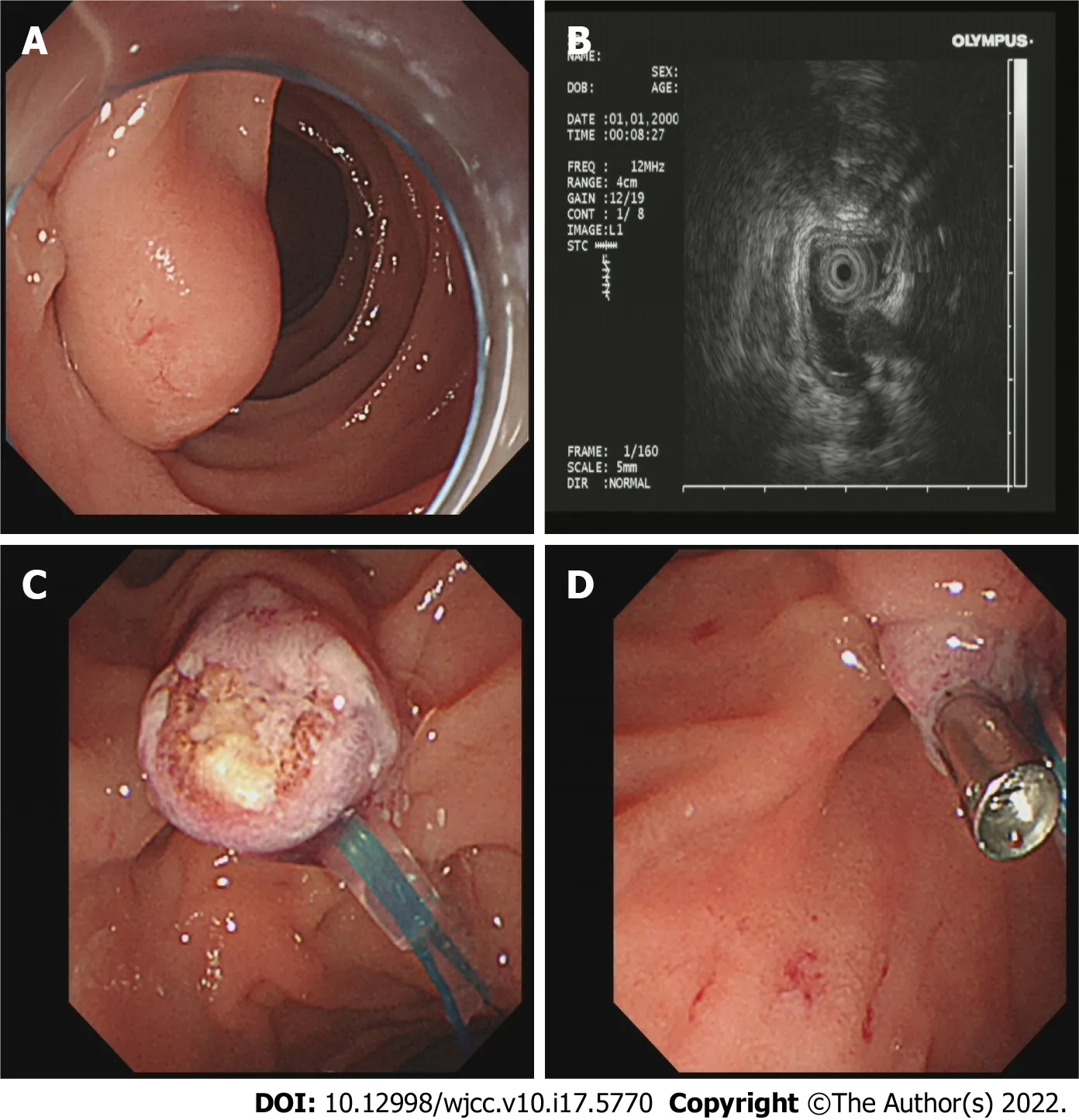
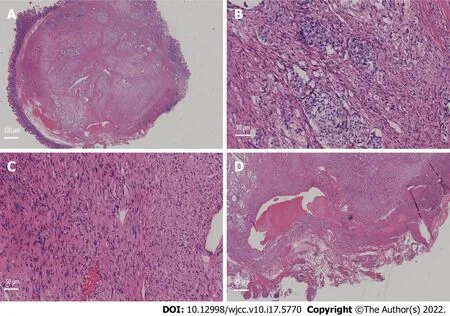
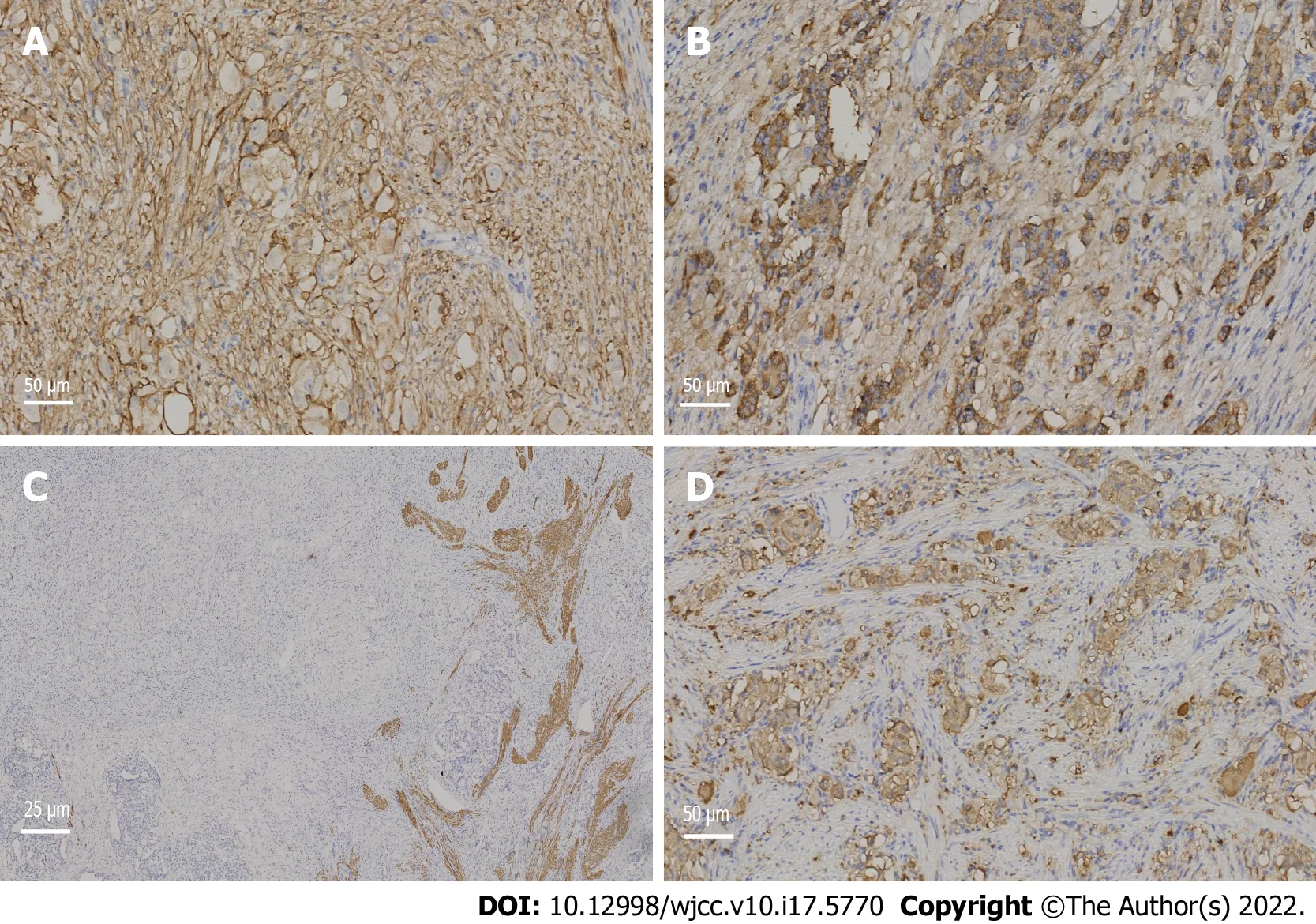
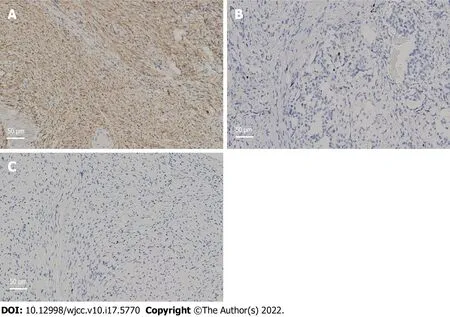
A 63-year-old female underwent upper gastrointestinal endoscopy at a local,grassroots hospital due to 1 mo of nausea and vomiting,and a large nipple was found in the descending part of the duodenum.The patient’s faecal occult blood test was positive.The patient had obvious symptoms of nausea and vomiting,often vomiting with no stomach contents and had lost 2 kg of weight within a month.Before the operation,we administered symptomatic treatment,such as replenishing gastric protective fluid.After excluding relevant surgical contraindications,endoscopic examination was performed on the patient in our hospital,and we found a protuberant mass above the nipple of the descending duodenum,with a smooth surface and a diameter of approximately 0.5 cm.A 12 MHz ultrasound probe showed that the tumour originated from the submucosa and showed low echo.We used a nylon noose to trap the tumour,cut the bottom of the base by snaring with an electrocurrent,and clamped the wound with a titanium clip to stop the bleeding(Figure 1).To confirm the diagnosis,the excised specimens were sent for pathological examination and immunohistochemistry.One week after the operation,the patient recovered smoothly and was discharged from the hospital.The pathological results showed that the tumour in the descending part of the duodenum was a NET(grade 1)with schwannoma,and the cutting edge was negative(Figure 2).The results of immunohistochemical staining indicated that the tumour cells were positive for antigen KI-67,broad-spectrum cytokeratin,CD56,synaptophysin(Syn),chromogranin A(CgA),S-100,nerve specific enolase,CD68,CD163,and myoglobin and were negative for CD34,succinate dehydrogenase B,CD117,DOG-1,smooth muscle actin,desmin,cytokeratin(CK)7,CK20,and myogenic differentiation 1(Figures 3 and 4).
Well, Heavens. Didn t you ever come down here to the station? He pointed14 across to his magazine stand. I ve been there all the time. I own it. I ve watched everybody that came up the stairs.
Immunohistochemical results showed that the mass was a rare NET with neurilemmoma.
History of past illness
To the best of our knowledge,this is the first publication of a neuroendocrine tumour of descending duodenum complicated with schwannoma.We removed the tumour by electrocoagulation completely and the patient recovered and was discharged.
Personal and family history
Parents have a history of hypertension.
Physical examination
Mild tenderness in the abdomen,no rebound pain.
Laboratory examinations
Then the Queen began to cry and sob5 so bitterly that the little man was sorry for her, and said: I ll give you three days to guess my name, and if you find it out in that time you may keep your child
Holy Communion. The church was large and handsome, and had been built centuries before by Scotchmen and Dutchmen; it stood some little way out of the town. It was rather ruinous certainly, and the road to it was heavy, through deep sand, but the people gladly surmounted these difficulties to get to the house of God, to sing psalms and to hear the sermon. The sand had heaped itself up round the walls of the church, but the graves were kept free from it.It was the largest church north of the Limfjorden. The VirginMary, with a golden crown on her head and the child Jesus in her arms, stood lifelike on the altar; the holy Apostles had been carved inthe choir, and on the walls there were portraits of the oldburgomasters and councillors of Skjagen; the pulpit was of carvedwork. The sun shone brightly into the church, and its radiance fell onthe polished brass chandelier and on the little ship that hung fromthe vaulted roof.
Imaging examinations
Mediastinal computed tomography(CT)showed no tumour metastasis.
MULTlDlSClPLlNARY EXPERT CONSULTATlON
Because this patient does not have other systemic diseases,multidisciplinary experts were not invited to discuss it.
the National Natural Science Foundation of China,No.82074214;and the Research Fund Project of Zhejiang Chinese Medical University,No.2019ZY02.
FlNAL DlAGNOSlS
NET of the descending part of the duodenum complicated with schwannoma.
TREATMENT
Zhang L and Zhang S were involved in the conception of the study;Zhang L and Zhang C were involved in writing the article;Zhang L,Ma PP,Feng SY,Wang QQ and Zhang S critically revised the manuscript;all authors read and approved the final manuscript.
OUTCOME AND FOLLOW-UP
Mediastinal CT showed no tumour metastasis,and the prognosis of the patient is good.
DlSCUSSlON
There may be rare cases of NETs with schwannoma in the descending part of the duodenum worldwide,but there are no clinical reports.To the best of our knowledge,this is the first clinical case report of a duodenal NET complicated with schwannoma,which has high clinical value.Endoscopic NETs and schwannomas of the duodenum do not have specific features and are often mistaken for enlarged duodenal papilla,resulting in missed diagnosis and worsening of the disease.Endoscopic ultrasonography(EUS)is of high value in the diagnosis of these two kinds of tumours.Under EUS,most of the lesions are hypoechoic lesions originating from the submucosa,with clear boundaries and homogeneous internal echoes,which is consistent with our ultrasound results[3].Duodenal schwannoma is extremely rare in gastrointestinal mesenchymal tumours,and only a few cases have been reported thus far.Duodenal neurilemmoma is often found by accident and is difficult to diagnose before surgery.There was no typical duodenal schwannoma under ordinary endoscopy.Due to the rare nature of duodenal schwannoma,no typical endoscopic ultrasonographic features have been reported[4].The immunohistochemical results of the specimen remain the gold standard for diagnosis.NET cells are often positive for CgA,CD56,CK,and Syn,while schwannoma cells are often positive for S-100[5],which is consistent with our immunohistochemical results.Endoscopic treatment is usually the first choice for gastrointestinal NETs or schwannomas with diameters less than 1 cm,as it does not invade the lamina propria and because endoscopic treatment has the characteristics of less trauma,less cost,good prognosis,and easy follow-up after the operation[6].It has been reported that snare polypectomy has a very high complete resection rate of gastrointestinal NETs(93.8%),and this rate may be high for several reasons.First,decoy polypectomy is more commonly used in smaller tumours(< 5.2 mm),and the appearance of polyps is more likely to be limited to the mucosa.The second reason is that electrosurgical devices,such as argon plasma coagulators,damage a larger field of vision during treatment.Therefore,for some small gastrointestinal NETs with specific shapes,the use of decoy electrocoagulation is completely effective[7].In this case,we used EUS to determine the lesion level and endoscopic electrocoagulation for R0 resection,suggesting the feasibility and broad prospect of early endoscopic diagnosis and treatment of the tumour.The KI-67 index of the specimen was approximately 1%,suggesting that the NET phase was G1.In addition,we examined the vertical edge of the specimen with a high-power microscope.The vertical edge was negative,and there was no lymphatic invasion,which proved that we successfully removed the tumour completely.Mediastinal CT showed no tumour metastasis,and the prognosis of the patient is good.
The authors declare that they have no conflict of interest.
CONCLUSlON
The patient has a history of infection with tuberculosis 40 years ago.The history of surgical trauma was bronchiectasis in 2015,hysterectomy and minimally invasive hysteroptosis in 2020.
FOOTNOTES
We removed the tumour by electrocoagulation and gave the patient some other symptomatic treatment to help stopping vomiting and protect the stomach.
One time, there was a couple came to buy fish from me, the gentleman is a good fish keeper with much knowledge about fish, we talked about fish behaviour, colour, size, feeding and so on.
The prince prostrated105 himself in thanks to heaven and Jamila, and said: O delicious person! O Chinese Venus! how shall I excuse myself for giving you so much trouble? With what words can I thank you? Then she called for a clothes-wallet and chose out a royal dress of honour
Informed written consent was obtained from the patient for publication of this report and any accompanying images.
She was the loveliest young princess, red and white, like milk and blood, with clear blue eyes and golden hair, but right in the middle of her forehead there was a little tuft of brown hair
The authors have read the CARE Checklist(2016),and the manuscript was prepared and revised according to the CARE Checklist(2016).
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial(CC BYNC 4.0)license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
China
Lu Zhang 0000-0001-7726-4846;Chi Zhang 0000-0002-8983-206X;Shu-Yan Feng 0000-0003-4787-2765;Pan pan Ma 0000-0003-1193-9454;Shuo Zhang 0000-0003-1120-5872;Qian-Qian Wang 0000-0002-5889-5316.
Guo XR
Filipodia
Guo XR
1 Oronsky B,Ma PC,Morgensztern D,Carter CA.Nothing But NEt:A Review of Neuroendocrine Tumors and Carcinomas.
2017;19: 991-1002[PMID: 29091800 DOI: 10.1016/j.neo.2017.09.002]
2 Madero Velázquez L,Uceda F,Buendía L.Duodenal schwannoma,an infrequent entity.
2021;113: 548-549[PMID: 33244978 DOI: 10.17235/reed.2020.7371/2020]
3 De Angelis C,Manfrè SF,Bruno M,Pellicano R.Hegemony and cost-effectiveness of endoscopic ultrasound(EUS)in the field of gastroenteropancreatic-neuroendocrine tumors(GEP-NETs).
2014;105: 363-370[PMID: 25325565]
4 Mori Y,Kurita A,Yazumi S.Gastrointestinal: Schwannoma of the duodenum.
2020;35: 1855[PMID: 32390278 DOI: 10.1111/jgh.15075]
5 Bellizzi AM.Immunohistochemistry in the diagnosis and classification of neuroendocrine neoplasms: what can brown do for you?
2020;96: 8-33[PMID: 31857137 DOI: 10.1016/j.humpath.2019.12.002]
6 Scherübl H,Cadiot G.Early Gastroenteropancreatic Neuroendocrine Tumors: Endoscopic Therapy and Surveillance.
2017;33: 332-338[PMID: 29177161 DOI: 10.1159/000459404]
7 Sun W,Wu S,Han X,Yang C.Effectiveness of Endoscopic Treatment for Gastrointestinal Neuroendocrine Tumors: A Retrospective Study.
2016;95: e3308[PMID: 27082572 DOI: 10.1097/MD.0000000000003308]
 World Journal of Clinical Cases2022年17期
World Journal of Clinical Cases2022年17期
- World Journal of Clinical Cases的其它文章
- Repetitive transcranial magnetic stimulation for post-traumatic stress disorder:Lights and shadows
- Response to dacomitinib in advanced non-small-cell lung cancer harboring the rare delE709_T710insD mutation:A case report
- Loss of human epidermal receptor-2 in human epidermal receptor-2+breast cancer after neoadjuvant treatment:A case report
- Tumor-like disorder of the brachial plexus region in a patient with hemophilia:A case report
- High-frame-rate contrast-enhanced ultrasound findings of liver metastasis of duodenal gastrointestinal stromal tumor:A case report and literature review
- Gitelman syndrome:A case report
