How to improve metastatic pancreatic ductal adenocarcinoma patients’ selection: Between clinical trials and the real-world
Andrea Pretta, Dario Spanu, Stefano Mariani, Nicole Liscia, Pina Ziranu, Valeria Pusceddu, Marco Puzzoni,Elena Massa, Mario Scartozzi, Eleonora Lai
Andrea Pretta, Dario Spanu, Stefano Mariani, Pina Ziranu, Valeria Pusceddu, Marco Puzzoni, Elena Massa, Mario Scartozzi, Eleonora Lai, Medical Oncology Unit, University Hospital and University of Cagliari, Monserrato 09042, Cagliari, Italy
Nicole Liscia, Department of Oncology, IRCCS San Raffaele Scientific Institute Hospital, Vita-Salute San Raffaele University, Milano 20121, Italy
Abstract As underlined in the minireview by Blomstrand et al, given the poor prognosis and the paucity of data on a therapeutic sequence in pancreatic ductal adenocarcinoma (PDAC), additional randomized controlled trials and real-world evidence studies addressing current and novel regimens are needed. The real-world outcomes of first-line chemotherapy regimens such as FOLFIRINOX and gemcitabine/nab-paclitaxel are thoroughly reviewed and seem to be largely generalizable in a real-world context. Regarding second-line chemotherapy, the key question about the optimal sequence of regimens remains uncertain. Precisely in this setting, it is therefore useful to encourage the implementation of clinical studies that may contribute to the scarcity of data available up to now. We report our experience with a small group of patients treated with second-line liposomal irinotecan (nal-IRI) plus 5-fluorouracil and leucovorin. To improve the treatment of patients affected by PDAC, it is useful to identify subgroups of patients who may benefit from target treatments (e.g., BRCA mutant) and it is also important to focus on any prognostic factors that may affect the survival and treatment of these patients.
Key Words: Metastatic pancreatic ductal adenocarcinoma; Palliative chemotherapy; Realworld data; Molecular selection; Biomarkers; Second-line treatment
TO THE EDITOR
We read with great interest the review by Prettaet al[1], entitled “Real-world evidence on first- and second-line palliative chemotherapy in advanced pancreatic cancer”. This review provides a comprehensive overview on real-life data of metastatic pancreatic ductal adenocarcinoma (PDAC) patients treated in the first- and second-line setting. The authors critically compare the results obtained in a realworld population with those provided by randomised clinical trials (RCT), highlighting that the outcomes are consistent and similar, especially on first-line with FOLFIRINOX and gemcitabine -nabpaclitaxel.
We agree with the authors that PDAC patients enrolled in RCT represent a highly selected population and that despite real-world outcomes derive from different countries, with various regulatory agencies and health care systems, all data available in the literature seems to confirm the effectiveness and safety of chemotherapy regimens in real-life settings. Moreover, since no strong data on second-line settings are available, we greatly appreciate the authors’ effort to analyse this topic.
At our Centre, we conducted a retrospective analysis in a real-world population of metastatic PDAC patients treated with second-line liposomal irinotecan (nal-IRI) plus 5-fluorouracil and leucovorin (5FU/LV) in a compassionate use program, in order to assess clinical outcome, tolerability and potential prognostic factors. Statistical analysis was performed with the MedCalc package. The association between categorical variables was estimated by chi-square test. Survival distribution was estimated by the Kaplan-Meier method and survival curves comparison was evaluated with the log-rank test. The cut off value for laboratory parameters was identified with ROC curves. The study was approved by the Ethical Committee of the Cagliari University Hospital (Prot. PG /2018/7339, June 1, 2018) and was performed in accordance with the ethical principles stated in the Declaration of Helsinki and in the International Conference on Harmonization (ICH) Note for Guidance on Good Clinical Practice (GCP, ICH E6, 1995) and all applicable regulatory requirements.
Globally, 14 patients treated with nal-IRI and 5FU/LV from June 2016 to November 2018 were included in our analysis. Baseline characteristics are shown in Table 1. Median overall survival (OS) was 9.1 (95%CI: 5.8-13.1) mo. Median progression free survival (PFS) was 7.2 mo (95%CI: 3.0-33.8). Three patients achieved a partial response, two had stable disease, and nine developed progression. Median duration of treatment with nal-IRI plus 5FU/LV was 6 mo; treatment longer than 6 mo was related to improved OS [13.1 mo (95%CI: 9-17)vs7.1 mo (95%CI: 2.9-13.1),P= 0.0127, HR = 0.18] and PFS [9.1 mo (95%CI: 7.2-33.8)vs3.1 mo (95%CI: 2.2-7.7),P= 0.0011, HR = 0.08]. Baseline haemoglobin levels equal or lower than 10 g/dL were associated with worse prognosis [OS: 11 mo (95%CI: 1-15.9)vs3 mo,P= 0.0384, HR = 0.005; PFS: 7.6 mo (95%CI: 3.1-33.8)vs3 mo,P= 0.0384, HR = 0.005]. 64% of patients developed grade > 2 toxicity. The occurrence of grade > 2 anaemia was related to shorter OS [3 movs11 mo (95%CI: 7.1-15.9),P= 0.0384, HR = 0.005] and PFS [3 movs7.6 mo (95%CI: 3.1-33.8),P= 0.0384, HR = 0.005]. As shown in Figure 1, the need for erythropoietin administration was associated with poorer OS [3 movs10.7 mo (95%CI: 7.1-15.9),P= 0.0287, HR = 0.003] and PFS [3 movs7.6 mo (95%CI 3.1-33.8),P= 0.0287, HR = 0.003]. In our real-world retrospective analysis, nal-IRI plus 5FU/LV confirmed its efficacy and tolerability, consistently with NAPOLI-1 RCT[2,3]. Longer duration of treatment was related to improved survival, whereas lower baseline haemoglobin levels, anaemia occurrence and the necessity of erythropoietin were negative prognostic factors. These results are consistent with some findings of a previous Italian large real-world analysis[4].
As underlined by Blomstrandet al[1], there is an urgent need for prognostic and predictive biomarkers to improve the therapeutic management of PDAC patients and to prolong survival as well as more effective treatment strategies. Indeed, intensive research efforts and substantial progress in the understanding of the PDAC genetic background and molecular biology have not yet been matched either by the successful development of novel agents or by the identification of predictive biomarkers that could increase the effectiveness of existing therapies[5]. In contrast to other solid tumours, immunotherapy strategies have failed to yield any notable impact in PDAC. This is likely related to the critical role of the tumour microenvironment as a physical barrier and its inhibitory immune signalling. The most promising therapeutic strategy seems to be combination of immunotherapeutics with other targeted treatments[6].
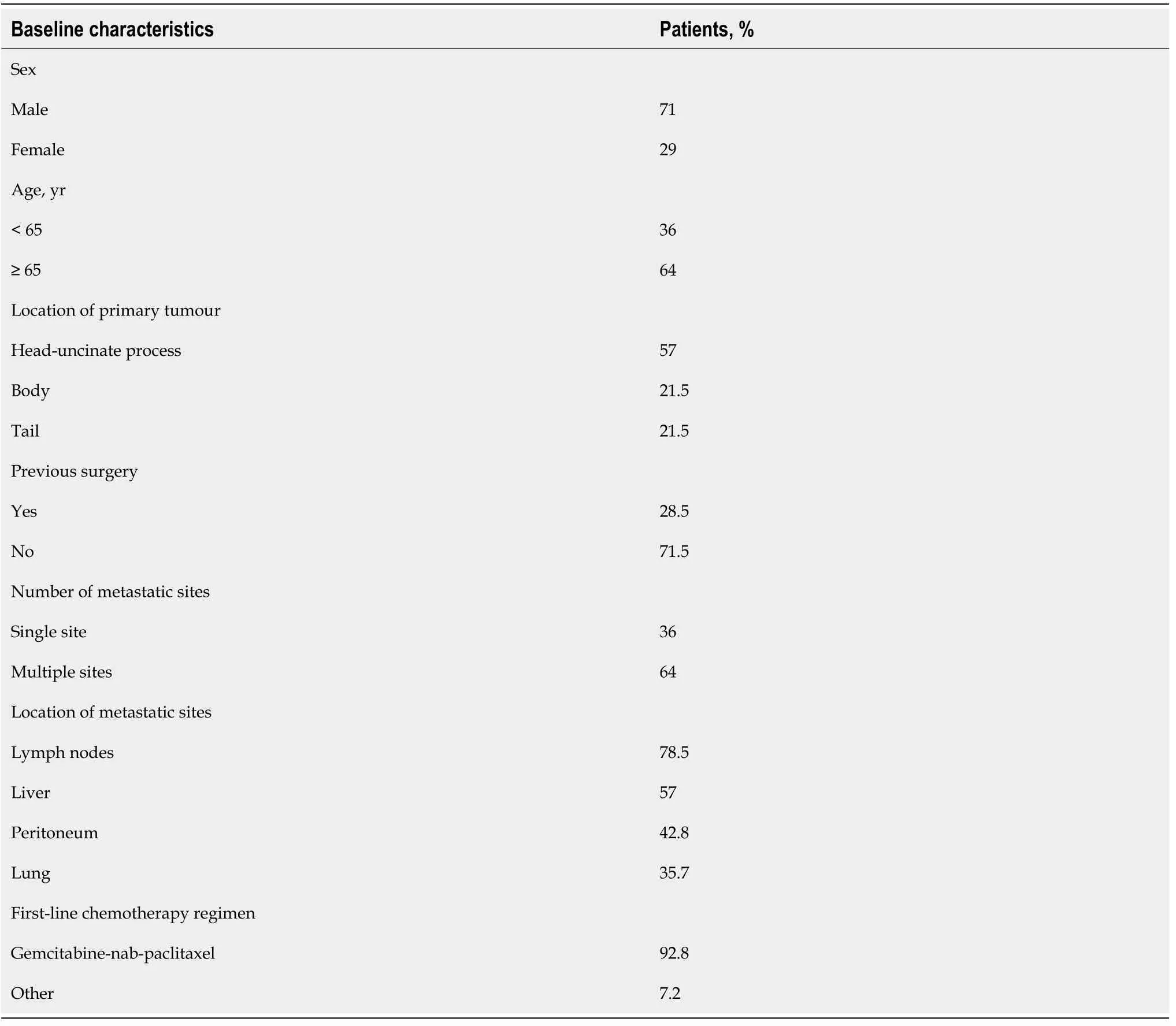
Table 1 Baseline characteristics of patients treated with second-line Nal-iri at the Medical Oncology Unit, University Hospital and University of Cagliari, Cagliari, Italy
To our knowledge, the only successful biomarker-driven phase III RCT so far is the POLO trial, which showed improved PFS with maintenance Olaparib, a PARP-inhibitor,vsplacebo in germline BRCAmutant PDAC not progressing after first-line platinum-based chemotherapy[7]. Notably, BRCA-mutant PDAC represents a unique entity with specific disease features that are still to be fully understood and BRCA1/2 alterations are the most explored targetable mutations. Moreover, in this patients’ setting, the sensitivity to platinum chemotherapy requires further research and confirmations. Recently, the concept of “BRCAness” has gained increasing importance. This term refers to high-grade genomic instability of non-BRCA-mutant cancers and represents a phenotype of defective homologous recombination to which somatic mutations in genes likeBRCA1/2,ATM,PALB2,CHEK1,RAD51, andFANCA, can contribute. For these reasons, “BRCAness” is under evaluation as a biomarker for DNA-damaging agents and PARP inhibitors[8].
Finally, we believe that in a real-life focusing-approach, a particular focus should be deserved to the assessment of the impact of comorbidities on the PDAC patients’ prognosis. In a retrospective analysis that we conducted on 164 advanced PDAC patients, we demonstrated a correlation between type II diabetes mellitus and improved OS, both in the exploratory and in the validation cohort at univariate analysis (16vs10 mo;P= 0.004 and 11vs6 mo;P= 0.01, respectively). Moreover, in multivariate analysis, insulin-treated patients compared with non-diabetic patients had a significantly increased survival of 4.6 mo (P= 0.03). Surely, the correlation between OS and insulin-treated type II diabetes mellitus should be confirmed in prospective clinical trials[9].
In conclusion, in the era of precision medicine, larger and prospective studies in the real-world population, with the focus on specific PDAC subtypes (e.g., BRCA-mutant), would further clarify the impact of available and innovative treatment strategies on PDAC patients and help identify potential biomarkers to improve patients’ selection and prognosis.
ACKNOWLEDGEMENTS
We acknowledge all the authors whose publications are referred in our article.
FOOTNOTES
Author contributions:All authors wrote and edited the manuscript.
Conflict-of-interest statement:Prof. Scartozzi reports associations with Amgen, Sanofi, MERCK SHARP DOHME, Eisai, Merck, and Bayer, outside the submitted work.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Italy
ORCID number:Andrea Pretta 0000-0002-0262-9270; Dario Spanu 0000-0003-2968-6811; Stefano Mariani 0000-0002-2513-1408; Nicole Liscia 0000-0002-0799-0209; Pina Ziranu 0000-0002-5659-7366; Valeria Pusceddu 0000-0003-4167-9091; Marco Puzzoni 0000-0001-5880-4309; Mario Scartozzi 0000-0001-5977-5546; Eleonora Lai 0000-0002-0275-8187.
S-Editor:Wu YXJ
L-Editor:Filipodia
P-Editor:Wu YXJ
 World Journal of Clinical Oncology2022年5期
World Journal of Clinical Oncology2022年5期
- World Journal of Clinical Oncology的其它文章
- Commentary: Evaluating potential glioma serum biomarkers, with future applications
- Immune checkpoint inhibitors in head and neck squamous cell carcinoma: A systematic review of phase-3 clinical trials
- Assessing optimal Roux-en-Y reconstruction technique after total gastrectomy using the Postgastrectomy Syndrome Assessment Scale-45
- Modified binding pancreaticogastrostomy vs modified Blumgart pancreaticojejunostomy after laparoscopic pancreaticoduodenectomy for pancreatic or periampullary tumors
- Survival characteristics of fibrolamellar hepatocellular carcinoma: A Surveillance, Epidemiology, and End Results database study
- Co-relation of SARS-CoV-2 related 30-d mortality with HRCT score and RT-PCR Ct value-based viral load in patients with solid malignancy
