Immune checkpoint inhibitors in head and neck squamous cell carcinoma: A systematic review of phase-3 clinical trials
Jissy Vijo Poulose, Cessal Thommachan Kainickal
Jissy Vijo Poulose, National Fellowship in Palliative Medicine (Training Program), Institute of Palliative Medicine, Calicut 673008, Kerala, India
Cessal Thommachan Kainickal, Department of Radiation Oncology, Regional Cancer Centre,Thiruvananthapuram 695011, Kerala, India
Abstract BACKGROUND The outcomes of patients diagnosed with head and neck squamous cell carcinoma (HNSCC) who are not candidates for local salvage therapy and of those diagnosed with recurrent or metastatic disease are dismal. A relatively new systemic therapy option that emerged in recent years in the treatment of advanced HNSCC is immunotherapy using immune checkpoint inhibitors (ICIs). The safety profile and anti-tumor activity of these agents demonstrated in early phase clinical trials paved the way to the initiation of several promising phase-3 trials in the field.AIM To evaluate the evidence on the effectiveness of ICIs in HNSCC, based on published phase-3 clinical trials.METHODS We searched PubMed, Cochrane Library, Embase, and Scopus to identify published literature evaluating immunotherapy using ICIs in recurrent or metastatic HNSCC (R/M HNSCC) and locally advanced head and neck squamous cell carcinoma (LAHNSCC). We used a combination of standardized search terms and keywords including head and neck squamous cell carcinoma, recurrent, metastatic, locally advanced, immunotherapy, immune checkpoint inhibitors, monoclonal antibodies, programmed cell death protein-1 (PD-1), programmed death-ligand 1 (PD-L1), cytotoxic T- lymphocyte associated protein-4 (CTLA-4), and phase-3 clinical trial. A sensitive search filter was used to limit our results to randomized controlled trials.RESULTS Five phase-3 clinical trials have reported the data on the effectiveness of immunotherapy in HNSCC so far: Four in R/M HNSCC and one in LAHNSCC. In patients with R/M HNSCC, anti-PD-1 agents nivolumab and pembrolizumab demonstrated improved survival benefits in the second-line treatment setting compared to the standard of care (standard singleagent systemic therapy). While the net gain in overall survival (OS) with nivolumab was 2.4 mo [hazard ratio (HR) = 0.69, P = 0.01], that with pembrolizumab was 1.5 mo (HR = 0.80 nominal P = 0.0161). The anti-PD-L1 agent durvalumab with or without the anti-cytotoxic T- lymphocyte associated protein-4 agent tremelimumab did not result in any beneficial outcomes. In the first-line setting, in R/M HNSCC, pembrolizumab plus platinum-based chemotherapy resulted in significant improvement in survival with a net gain in OS of 2.3 mo (HR = 0.77, P = 0.0034) in the overall population and a net gain in OS of 4.2 mo in the PD-L1 positive (combined positive score > 20) population compared to standard of care (EXTREME regime). In patients with PD-L1 positive R/M HNSCC, monotherapy with pembrolizumab also demonstrated statistically significant improvement in survival compared to EXTREME. In LAHNSCC, immunotherapy using avelumab (an anti-PD-L1 agent) along with standard chemoradiation therapy did not result in improved outcomes compared to placebo plus chemoradiation therapy.CONCLUSION Anti-PD-1 agents provide survival benefits in R/M HNSCC in the first and second-line settings, with acceptable toxicity profiles compared to standard therapy. There is no proven efficacy in the curative setting to date.
Key Words: Head and neck squamous cell carcinoma; Recurrent/metastatic head and neck squamous cell carcinoma; Locally advanced head and neck squamous cell carcinoma; Immune checkpoint inhibitors;Immunotherapy; Monoclonal antibody
INTRODUCTION
Head and neck squamous cell carcinoma (HNSCC) is one of the major causes of cancer-associated morbidity and mortality globally[1-3]. Treatment approaches for HNSCC vary according to the stage of the disease at presentation. Around 40% of HNSCCs present at an early stage and are treated by a single treatment modality, either radical radiotherapy or surgery. The remaining 60% of cases present as locally advanced disease, and treatment options include chemoradiation or surgery followed by adjuvant therapy. However, within 3 years, over 50% of these patients relapse locally or at distant sites. Salvage approaches for the locally recurrent disease include surgery, surgery followed by re-irradiation, or re-irradiation with or without concurrent chemotherapy[4,5]. For a recurrent disease that is not amenable to salvage approach and for metastatic disease, platinum-based chemotherapy was the only available treatment option until recently. While the median survival of recurrent/metastatic HNSCC (R/M HNSCC) patients receiving platinum-based chemotherapy is 7.4 mo, some patients become refractory to platinum and die within a period of 4 mo[6-12]. Subsequently, the addition of the antiepidermal growth factor receptor (EGFR) targeted agent cetuximab to platinum-based chemotherapy showed improvement in survival compared to platinum-based chemotherapy alone, as demonstrated in a landmark phase-3 trial in 2008[12-16].
A relatively new systemic therapy option that emerged in recent years in the treatment of advanced HNSCC is immunotherapy using immune checkpoint inhibitors (ICIs). The checkpoint pathways in the tumor microenvironment are responsible for immune escape and T cell exhaustion related to the survival of the cancer cells. ICIs are monoclonal antibodies that can block these pathways by inhibiting the binding of checkpoint proteins on the T cells to similar proteins on the tumor cells. Thus, these agents act by reinvigorating the immune cells and re-establishing the anti-tumor immune responses that promote the elimination of cancer cells. Programmed cell death protein-1 (PD-1) receptors, programmed death-ligand 1 (PD-L1) receptors, and cytotoxic T- lymphocyte associated protein-4 (CTLA-4) are the major established targets for cancer immunotherapy with ICIs, and the therapeutic effects of ICIs result from blockade of these receptors[17-20].
In recent years, many interventional studies have evaluated ICI therapy for the treatment of HNSCC. The objective of this systematic review is to gather the evidence from published phase-3 randomized controlled trials (RCTs) comparing immunotherapy with the standard of care (SOC), among patients with R/M HNSCC or locally advanced HNSCC (LAHNSCC). We aimed to evaluate and synthesize the evidence from the published phase-3 studies investigating immunotherapy in advanced head and neck cancer using checkpoint inhibitors, either alone or in combination with chemotherapy, radiation therapy, or another checkpoint inhibitor.
MATERIALS AND METHODS
Data sources and literature search
The study followed the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines[21]. We systematically searched PubMed, SCOPUS, EMBASE, and COCHRANE Library without any language limit. We used a combination of standardized search terms and keywords including head and neck squamous cell carcinoma, recurrent, metastatic, locally advanced, immunotherapy, checkpoint inhibitors, monoclonal antibodies, PD-1, PD-L1, CTLA-4, and phase-3 clinical trial. A sensitive search filter was used to limit our results to RCTs reported from January 2000 till February 2021. The initial search was conducted in February 2021. We also looked for any updates on the selected studies till April 2021. The search syntax is given in the Supplementary file.
Inclusion/exclusion criteria and study selection
Studies were included if they were completed phase-3 RCTs conducted among patients with R/M HNSCC or LAHNSCC, in which the intervention patients received ICI either alone or in combination with chemotherapy, radiation therapy, or with another IO and the control patients received SOC. Anatomical sites of primary tumors were oral cavity, oropharynx, hypopharynx, and larynx in the included studies. Early phase trials and observational studies were excluded. Studies involving patients with nasopharyngeal carcinoma were also excluded.
Titles generated from the initial search results were exported to EndNote. Duplicates were removed, and the remaining titles were scanned for relevance. Abstracts of articles pertaining to potentially eligible studies were independently reviewed by both authors and uncertainties were resolved through discussion. Potentially eligible studies were further evaluated for relevance, trial status (completed/ ongoing/withdrawn), and availability of results.
The following descriptive data were extracted from the included studies: Study design, population, details of the intervention, details of treatment received by the control arm, and the primary and secondary endpoints. Information on adverse events and statistical data on the outcomes were also extracted, which included, overall survival (OS), progression-free survival (PFS), overall response rate (ORR), biomarker effect, and patient-reported outcomes. The flow chart of study selection (PRISMA) is given in Figure 1.
RESULTS
The original literature search generated 565 titles altogether, of which 100 titles were eventually selected for abstract review for identification of potentially eligible studies. Others were excluded as they were related to phase-1 or phase-2 studies or not precisely relevant to the topic of the review. Through the abstract review, we identified 56 references (including one conference abstract) pertaining to potentially eligible studies. Through full-text review of these references, we selected five original phase-3 RCTs to be included in the systematic review[22-26]. In four of the trials[22-25], participants were patients with R/M HNSCC, while in one trial, participants were patients diagnosed with LAHNSCC[26,27]. All four studies among patients with R/M HNSCC were open-label RCTs; three of them investigated the effectiveness of ICI as second-line treatment[22-24], while in one study[25], ICI was evaluated as first-line treatment. The study among LAHSCC patients was a double-blinded placebo-controlled RCT[26,27].
ICIs assessed in these studies were nivolumab, pembrolizumab, durvalumab, tremelimumab, and avelumab. While nivolumab and pembrolizumab are anti-PD-1 monoclonal antibodies, durvalumab and avelumab are anti-PD-L1 antibodies. The monoclonal antibody tremelimumab is an anti-CTLA-4 agent[28-31].
We classified the studies into three groups based on the disease status and the treatment setting. The details of these studies in terms of the study population, intervention, comparator, outcomes, and adverse events are given in Table 1.
Phase-3 studies evaluating ICI as second-line treatment in R/M HNSCC (three RCTs: CheckMate 141,KEYNOTE 040, and EAGLE)
So far, three phase-3 RCTs have compared the effectiveness of ICI against the existing SOC (single-agent systemic therapy with methotrexate, docetaxel, or cetuximab) in the second-line treatment setting[22-24] (Table 1).
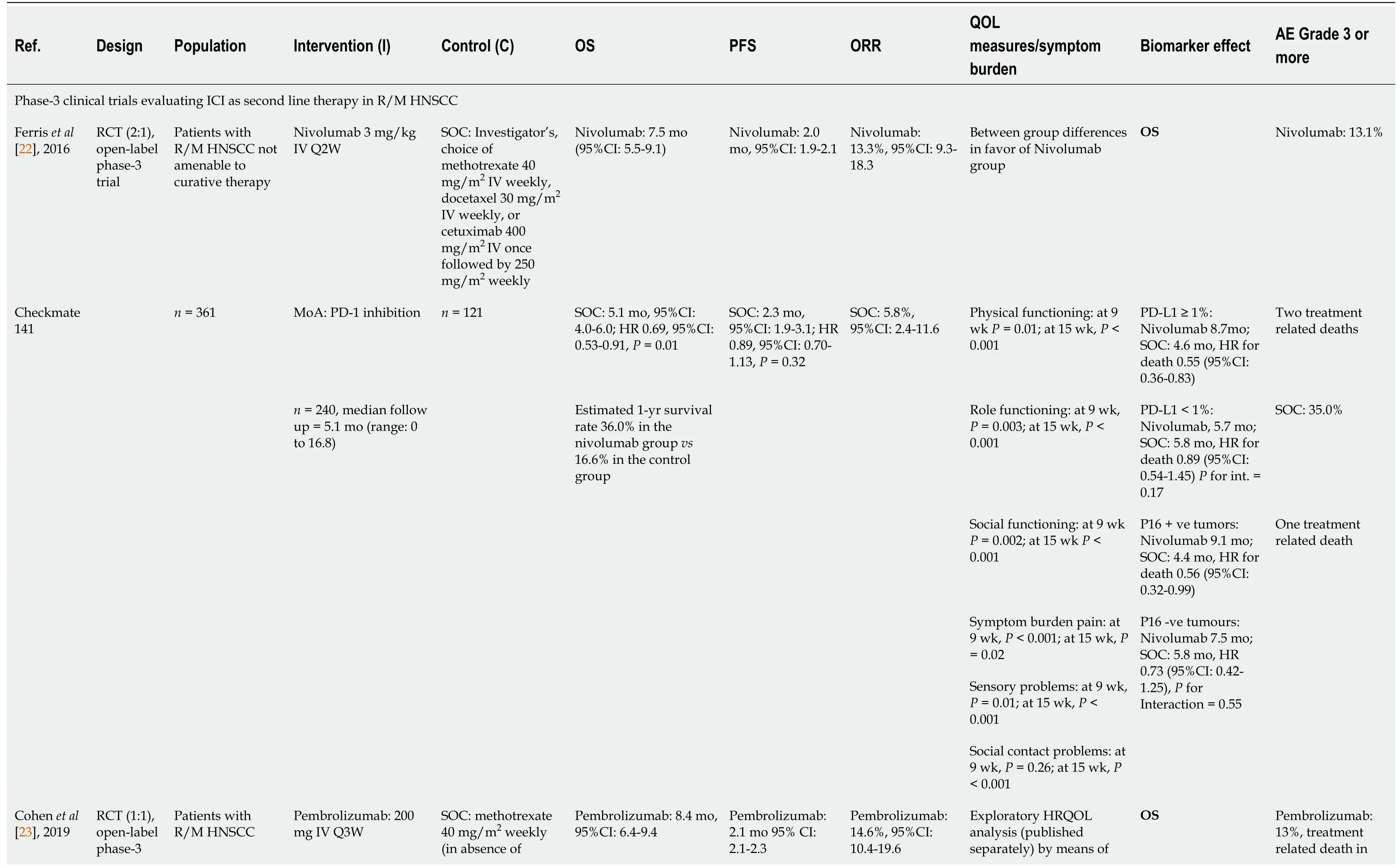
Table 1 Studies included in the systematic review
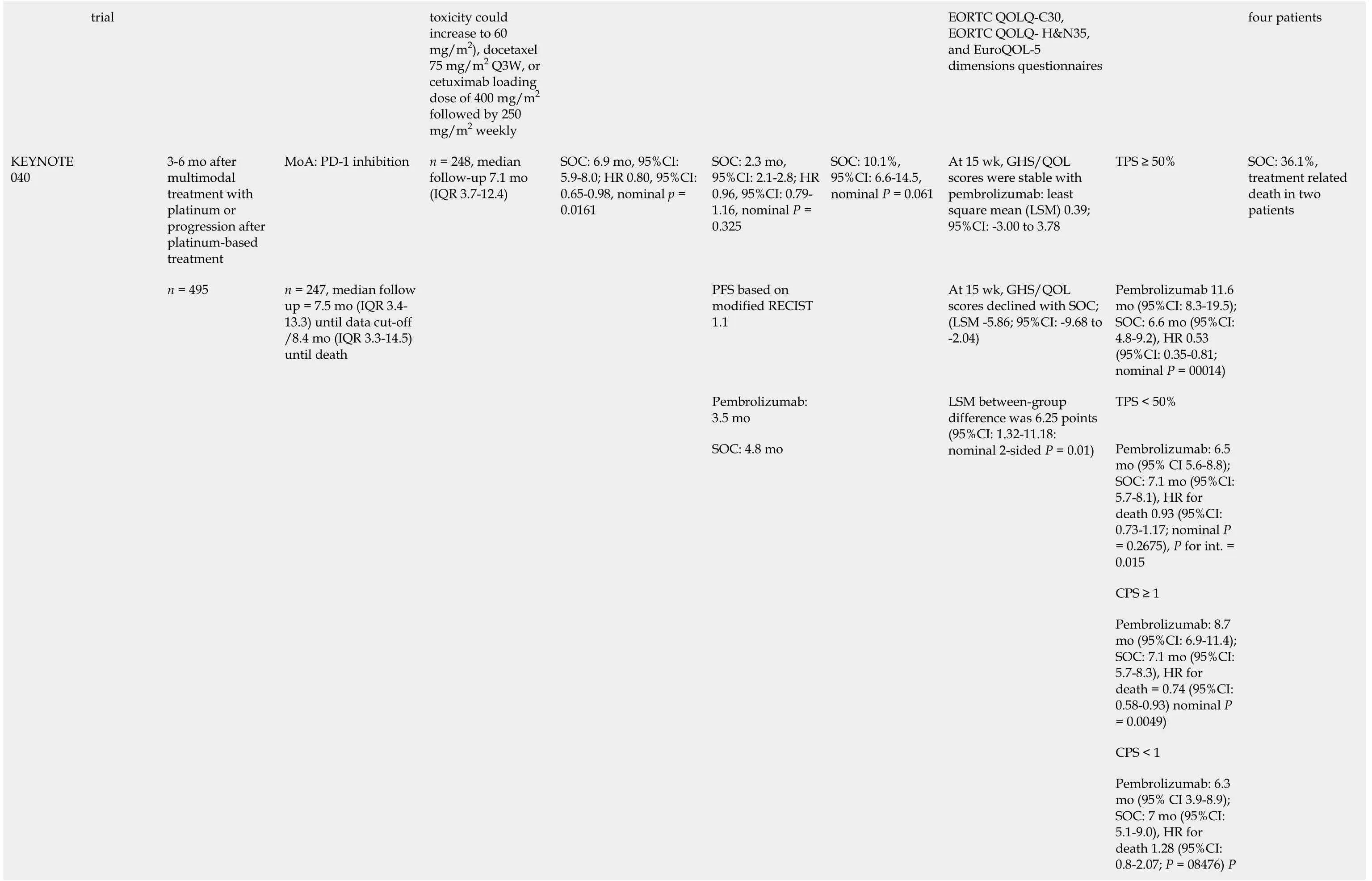
toxicity could increase to 60 mg/m2), docetaxel 75 mg/m2 Q3W, or cetuximab loading dose of 400 mg/m2 followed by 250 mg/m2 weekly EORTC QOLQ-C30, EORTC QOLQ- H&N35, and EuroQOL-5 dimensions questionnaires four patients 3-6 mo after multimodal treatment with platinum or progression after platinum-based treatment MoA: PD-1 inhibition SOC: 2.3 mo, 95%CI: 2.1-2.8; HR 0.96, 95%CI: 0.79-1.16, nominal P = 0.325 At 15 wk, GHS/QOL scores were stable with pembrolizumab: least square mean (LSM) 0.39; 95%CI: -3.00 to 3.78 TPS ≥ 50%PFS based on modified RECIST 1.1 At 15 wk, GHS/QOL scores declined with SOC; (LSM -5.86; 95%CI: -9.68 to -2.04)Pembrolizumab 11.6 mo (95%CI: 8.3-19.5); SOC: 6.6 mo (95%CI: 4.8-9.2), HR 0.53 (95%CI: 0.35-0.81; nominal P = 00014)Pembrolizumab: 3.5 mo TPS < 50%Pembrolizumab: 6.5 mo (95% CI 5.6-8.8); SOC: 7.1 mo (95%CI: 5.7-8.1), HR for death 0.93 (95%CI: 0.73-1.17; nominal P= 0.2675), P for int. = 0.015 CPS ≥ 1 Pembrolizumab: 8.7 mo (95%CI: 6.9-11.4); SOC: 7.1 mo (95%CI: 5.7-8.3), HR for death = 0.74 (95%CI: 0.58-0.93) nominal P= 0.0049)CPS < 1 Pembrolizumab: 6.3 mo (95% CI 3.9-8.9); SOC: 7 mo (95%CI: 5.1-9.0), HR for death 1.28 (95%CI: 0.8-2.07; P = 08476) P KEYNOTE 040 trial n = 495 n = 247, median follow up = 7.5 mo (IQR 3.4-13.3) until data cut-off /8.4 mo (IQR 3.3-14.5) until death n = 248, median follow-up 7.1 mo (IQR 3.7-12.4)SOC: 6.9 mo, 95%CI: 5.9-8.0; HR 0.80, 95%CI: 0.65-0.98, nominal p = 0.0161 SOC: 4.8 mo SOC: 10.1%, 95%CI: 6.6-14.5, nominal P = 0.061 LSM between-group difference was 6.25 points (95%CI: 1.32-11.18: nominal 2-sided P = 0.01)SOC: 36.1%, treatment related death in two patients
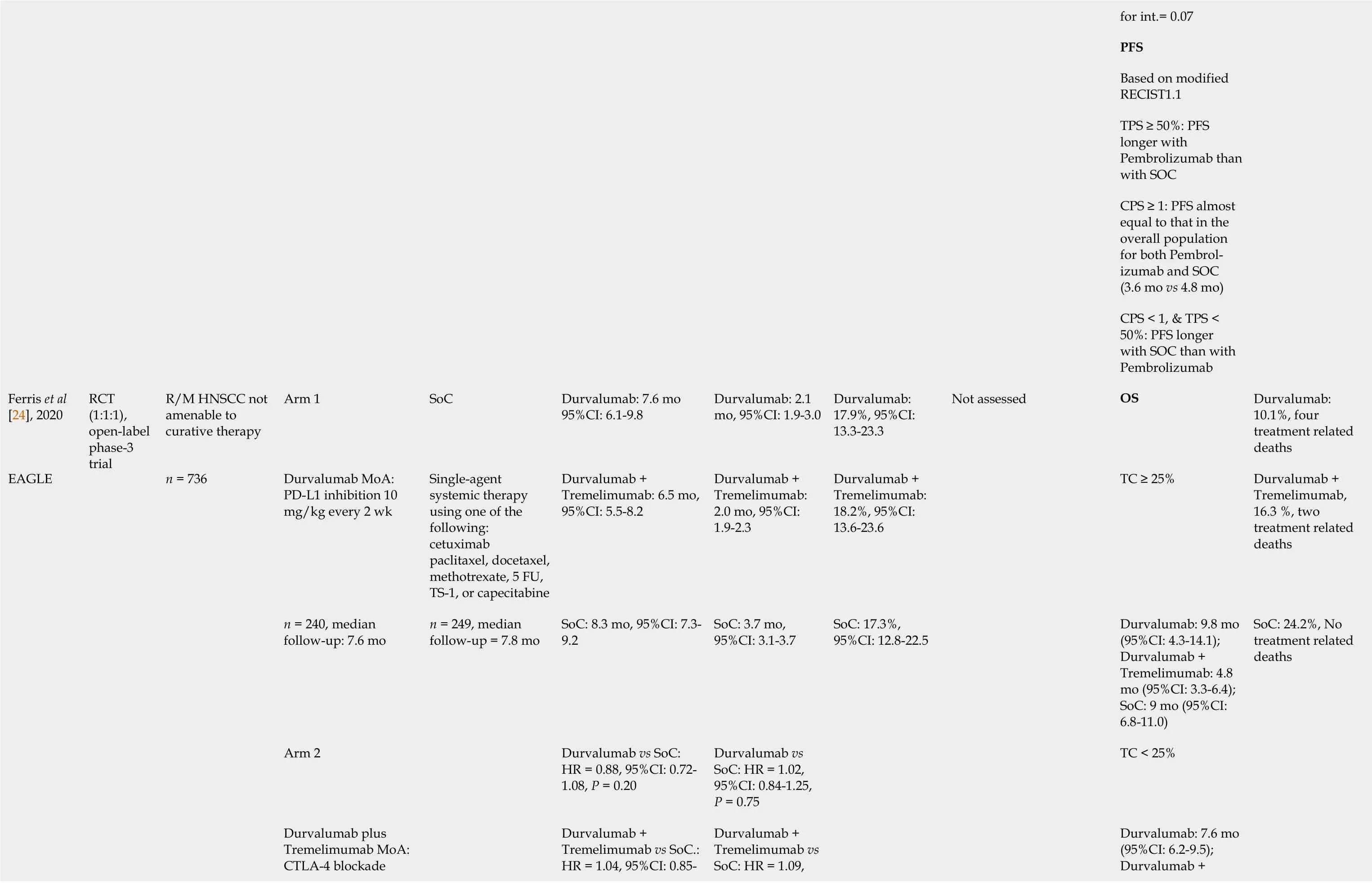
for int.= 0.07 PFS Based on modified RECIST1.1 TPS ≥ 50%: PFS longer with Pembrolizumab than with SOC CPS ≥ 1: PFS almost equal to that in the overall population for both Pembrolizumab and SOC (3.6 mo vs 4.8 mo)CPS < 1, & TPS < 50%: PFS longer with SOC than with Pembrolizumab Ferris et al[24], 2020 R/M HNSCC not amenable to curative therapy Arm 1 SoC Durvalumab: 7.6 mo 95%CI: 6.1-9.8 Durvalumab: 2.1 mo, 95%CI: 1.9-3.0 Durvalumab: 17.9%, 95%CI: 13.3-23.3 Not assessed OS Durvalumab: 10.1%, four treatment related deaths Durvalumab MoA: PD-L1 inhibition 10 mg/kg every 2 wk Single-agent systemic therapy using one of the following: cetuximab paclitaxel, docetaxel, methotrexate, 5 FU, TS-1, or capecitabine Durvalumab + Tremelimumab: 6.5 mo, 95%CI: 5.5-8.2 Durvalumab + Tremelimumab: 2.0 mo, 95%CI: 1.9-2.3 Durvalumab + Tremelimumab: 18.2%, 95%CI: 13.6-23.6 TC ≥ 25%Durvalumab + Tremelimumab, 16.3 %, two treatment related deaths n = 240, median follow-up: 7.6 mo SoC: 8.3 mo, 95%CI: 7.3-9.2 SoC: 3.7 mo, 95%CI: 3.1-3.7 SoC: 17.3%, 95%CI: 12.8-22.5 Durvalumab: 9.8 mo (95%CI: 4.3-14.1); Durvalumab + Tremelimumab: 4.8 mo (95%CI: 3.3-6.4); SoC: 9 mo (95%CI: 6.8-11.0)Arm 2 Durvalumab vs SoC: HR = 0.88, 95%CI: 0.72-1.08, P = 0.20 Durvalumab vs SoC: HR = 1.02, 95%CI: 0.84-1.25, P = 0.75 TC < 25%Durvalumab + Tremelimumab vs SoC.: HR = 1.04, 95%CI: 0.85-Durvalumab + Tremelimumab vs SoC: HR = 1.09, Durvalumab: 7.6 mo (95%CI: 6.2-9.5); Durvalumab + EAGLE RCT (1:1:1), open-label phase-3 trial n = 736 Durvalumab plus Tremelimumab MoA: CTLA-4 blockade n = 249, median follow-up = 7.8 mo SoC: 24.2%, No treatment related deaths
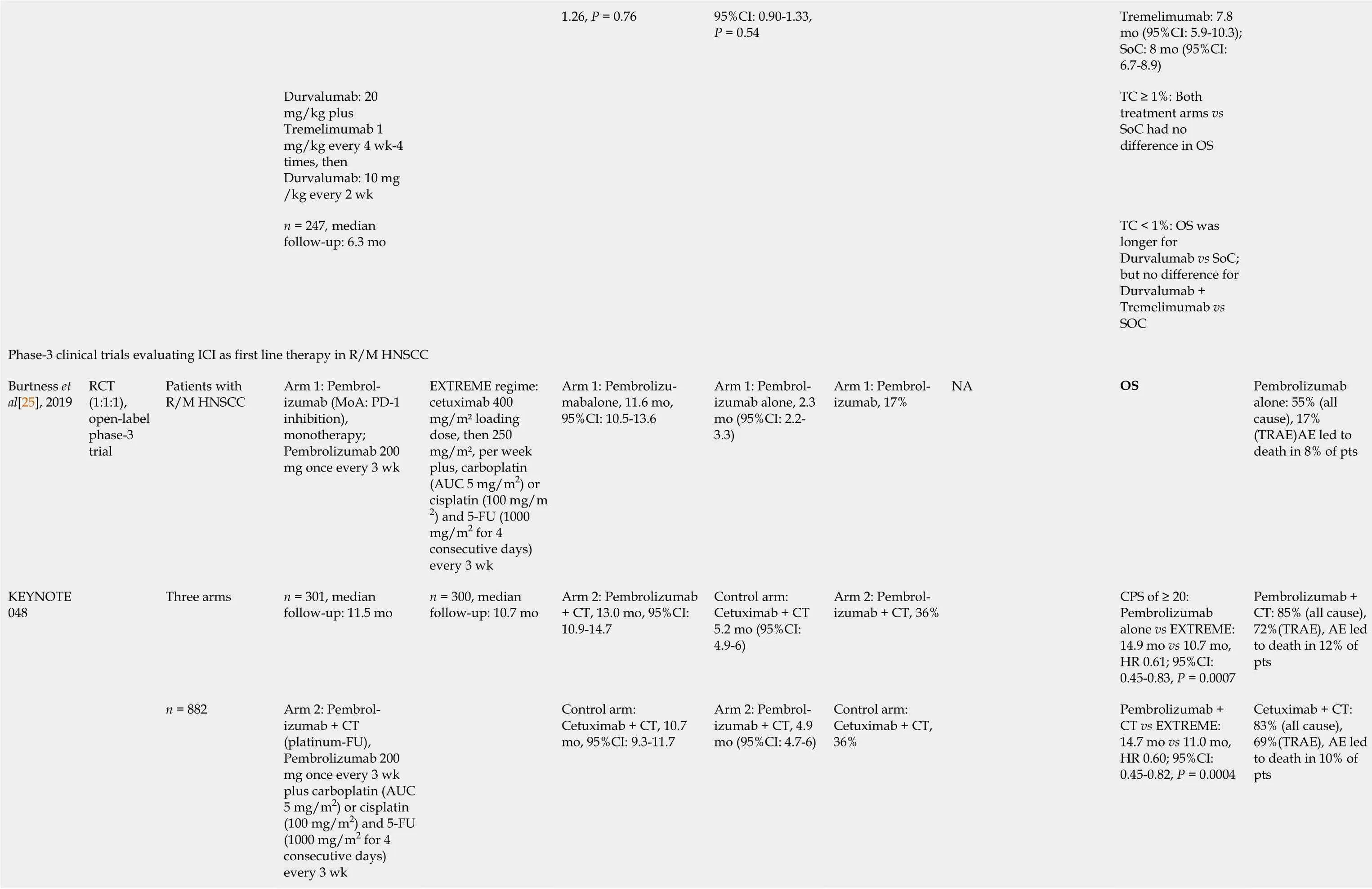
Tremelimumab: 7.8 mo (95%CI: 5.9-10.3); SoC: 8 mo (95%CI: 6.7-8.9)Durvalumab: 20 mg/kg plus Tremelimumab 1 mg/kg every 4 wk-4 times, then Durvalumab: 10 mg /kg every 2 wk TC ≥ 1%: Both treatment arms vs SoC had no difference in OS n = 247, median follow-up: 6.3 mo 1.26, P = 0.76 95%CI: 0.90-1.33, P = 0.54 TC < 1%: OS was longer for Durvalumab vs SoC; but no difference for Durvalumab + Tremelimumab vs SOC Phase-3 clinical trials evaluating ICI as first line therapy in R/M HNSCC Burtness et al[25], 2019 Patients with R/M HNSCC Arm 1: Pembrolizumab (MoA: PD-1 inhibition), monotherapy; Pembrolizumab 200 mg once every 3 wk EXTREME regime: cetuximab 400 mg/m2 loading dose, then 250 mg/m2, per week plus, carboplatin (AUC 5 mg/m2) or cisplatin (100 mg/m 2) and 5-FU (1000 mg/m2 for 4 consecutive days) every 3 wk Arm 1: Pembrolizumabalone, 11.6 mo, 95%CI: 10.5-13.6 Arm 1: Pembrolizumab alone, 2.3 mo (95%CI: 2.2-3.3)Arm 1: Pembrolizumab, 17%OS Pembrolizumab alone: 55% (all cause), 17% (TRAE)AE led to death in 8% of pts Three arms n = 301, median follow-up: 11.5 mo Arm 2: Pembrolizumab + CT, 13.0 mo, 95%CI: 10.9-14.7 Control arm: Cetuximab + CT 5.2 mo (95%CI: 4.9-6)Arm 2: Pembrolizumab + CT, 36%CPS of ≥ 20: Pembrolizumab alone vs EXTREME: 14.9 mo vs 10.7 mo, HR 0.61; 95%CI: 0.45-0.83, P = 0.0007 Pembrolizumab + CT: 85% (all cause), 72%(TRAE), AE led to death in 12% of pts Arm 2: Pembrolizumab + CT (platinum-FU), Pembrolizumab 200 mg once every 3 wk plus carboplatin (AUC 5 mg/m2) or cisplatin (100 mg/m2) and 5-FU (1000 mg/m2 for 4 consecutive days) every 3 wk Control arm: Cetuximab + CT, 10.7 mo, 95%CI: 9.3-11.7 Arm 2: Pembrolizumab + CT, 4.9 mo (95%CI: 4.7-6)Pembrolizumab + CT vs EXTREME: 14.7 mo vs 11.0 mo, HR 0.60; 95%CI: 0.45-0.82, P = 0.0004 KEYNOTE 048 RCT (1:1:1), open-label phase-3 trial n = 882 n = 300, median follow-up: 10.7 mo Control arm: Cetuximab + CT, 36%NA Cetuximab + CT: 83% (all cause), 69%(TRAE), AE led to death in 10% of pts
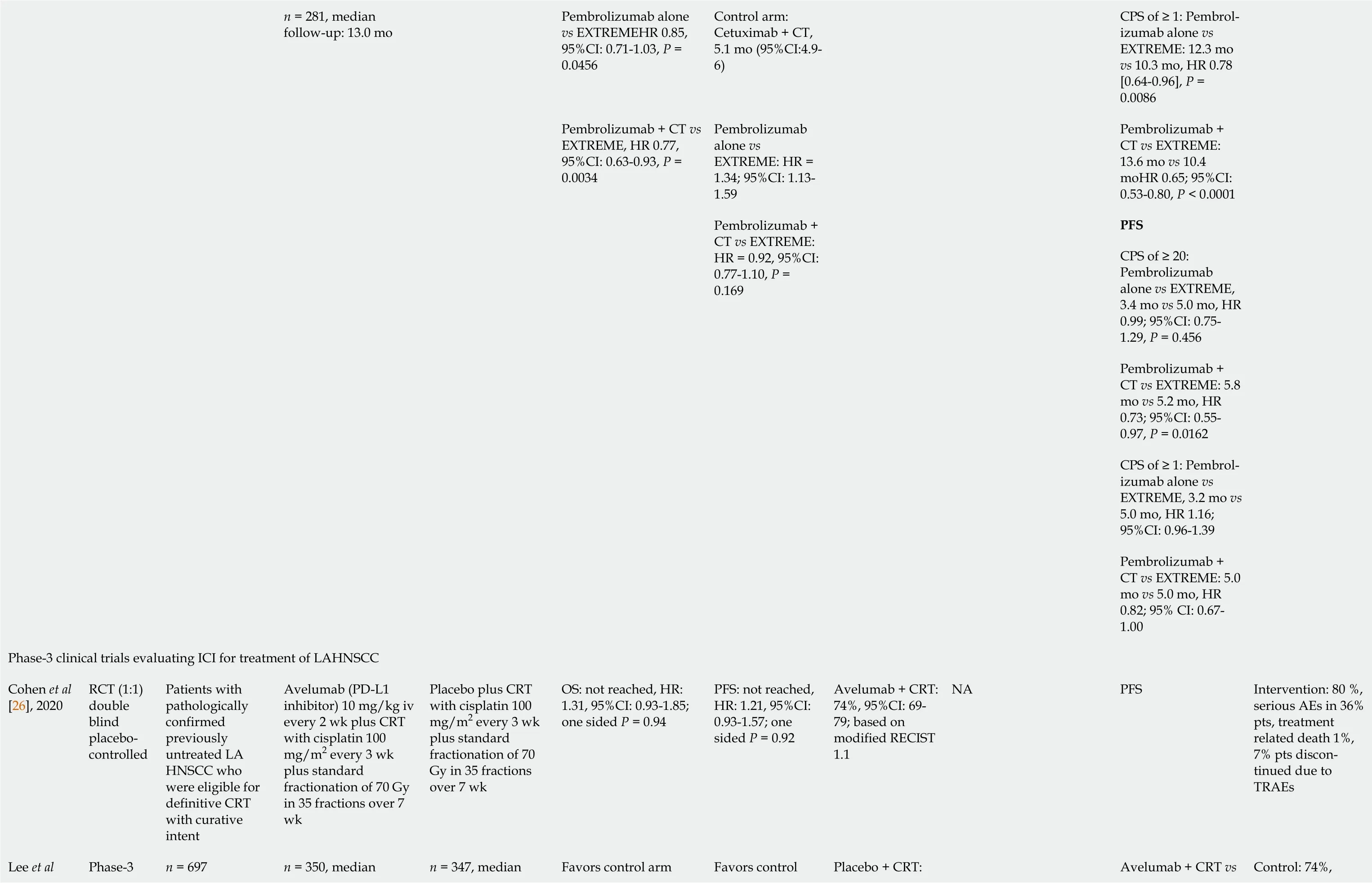
Pembrolizumab alone vs EXTREMEHR 0.85, 95%CI: 0.71-1.03, P = 0.0456 Control arm: Cetuximab + CT, 5.1 mo (95%CI:4.9-6)CPS of ≥ 1: Pembrolizumab alone vs EXTREME: 12.3 mo vs 10.3 mo, HR 0.78 [0.64-0.96], P = 0.0086 Pembrolizumab alone vs EXTREME: HR = 1.34; 95%CI: 1.13-1.59 Pembrolizumab + CT vs EXTREME: 13.6 mo vs 10.4 moHR 0.65; 95%CI: 0.53-0.80, P < 0.0001 PFS CPS of ≥ 20: Pembrolizumab alone vs EXTREME, 3.4 mo vs 5.0 mo, HR 0.99; 95%CI: 0.75-1.29, P = 0.456 Pembrolizumab + CT vs EXTREME: 5.8 mo vs 5.2 mo, HR 0.73; 95%CI: 0.55-0.97, P = 0.0162 CPS of ≥ 1: Pembrolizumab alone vs EXTREME, 3.2 mo vs 5.0 mo, HR 1.16; 95%CI: 0.96-1.39 n = 281, median follow-up: 13.0 mo Pembrolizumab + CT vs EXTREME, HR 0.77, 95%CI: 0.63-0.93, P = 0.0034 Pembrolizumab + CT vs EXTREME: HR = 0.92, 95%CI: 0.77-1.10, P = 0.169 Pembrolizumab + CT vs EXTREME: 5.0 mo vs 5.0 mo, HR 0.82; 95% CI: 0.67-1.00 Phase-3 clinical trials evaluating ICI for treatment of LAHNSCC Cohen et al[26], 2020 RCT (1:1) double blind placebocontrolled Patients with pathologically confirmed previously untreated LA HNSCC who were eligible for definitive CRT with curative intent Avelumab (PD-L1 inhibitor) 10 mg/kg iv every 2 wk plus CRT with cisplatin 100 mg/m2 every 3 wk plus standard fractionation of 70 Gy in 35 fractions over 7 wk Placebo plus CRT with cisplatin 100 mg/m2 every 3 wk plus standard fractionation of 70 Gy in 35 fractions over 7 wk OS: not reached, HR: 1.31, 95%CI: 0.93-1.85; one sided P = 0.94 PFS: not reached, HR: 1.21, 95%CI: 0.93-1.57; one sided P = 0.92 Avelumab + CRT: 74%, 95%CI: 69-79; based on modified RECIST 1.1 PFS Intervention: 80 %, serious AEs in 36% pts, treatment related death 1%, 7% pts discontinued due to TRAEs Lee et al Phase-3 n = 350, median n = 347, median Favors control Placebo + CRT: Avelumab + CRT vs Control: 74%, n = 697 Favors control arm NA
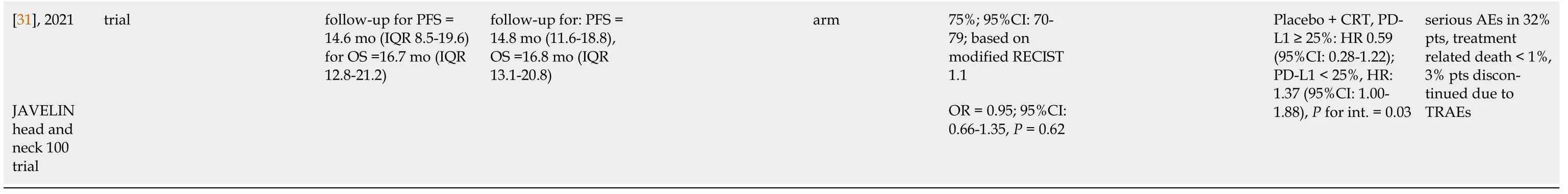
QOL: Quality of life; HRQOL: Health-related QOL; CRT: Chemoradiation therapy; OS: Overall survival; PFS: Progression-free survival; ORR: Objective response rate; ICI: Immune checkpoint inhibitors; R/M HNSCC: Recurrent or metastatic head and neck squamous cell carcinoma; LAHNSCC: Locally advanced head and neck squamous cell carcinoma; RCT: Randomized controlled trial; PD-1: Programmed cell death protein-1; PD-L1: Programmed death-ligand 1; CTLA-4: Cytotoxic T- lymphocyte associated protein-4; AE: Adverse event; TRAE: Treatment-related AEs; SOC: Standard of care; CPS: Combined positive score; CI: Confidence interval; IV: Intravenously; MoA: Mechanism of action; HR: Hazard ratio; IQR: Interquartile range; LSM: Least mean square; TPS: Tumor proportion score; Mab: Monoclonal antibody; CT: Chemotherapy.
CheckMate 141 (nivolumab vs standard single-agent systemic therapy)
Ferriset al[22] conducted a randomized, open-label, phase-3 study (n= 361) among patients with platinum-refractory recurrent HNSCC (recurrence within 6 mo after platinum-based chemotherapy) to investigate the effectiveness of the anti-PD-1 checkpoint inhibitor agent nivolumab. The intervention arm (n= 240) received nivolumab at a dose of 3 mg/kg body weight every 2 wk, while the control patients (n= 121) received SOC in the form of standard single-agent systemic therapy with methotrexate [40 mg/m2intravenously (IV) weekly], docetaxel (30 mg/m2IV weekly), or cetuximab (400 mg/m2IV once followed by 250 mg/m2weekly). OS was the primary endpoint of the study. Secondary endpoints included PFS, ORR, and biomarker effects on survival, safety, and quality of life assessments. The median duration of follow-up was 5.1 mo (range, 0 to 16.8).
Outcomes
OS:The median OS was 7.5 mo [95% confidence interval (CI): 5.5-9.1] with nivolumabvs5.1 mo (95%CI: 4.0-6.0) with SOC [hazard ratio (HR) = 0.69; 97.73%CI: 0.53-0.91;P= 0.01]. The estimated 1-year survival rate was 36.0% in the nivolumab groupvs16.6% in the control group.
PFS:PFS was reported as 2 mo (95%CI: 1.9-2.1) with nivolumab vs 2.3 mo (95%CI: 1.9-3.1) with SOC (HR = 0.89; 95%CI: 0.70-1.13; P = 0.32).
ORR:ORR was 13.3% (95%CI: 9.3-18.3) in the intervention arm with nivolumab, whereas it was 5.8% (95%CI: 2.4-11.6) in the control arm (SOC).
Patient-reported outcomes (quality of life):Physical, role, and social functioning (assessed by means of EORTC QOLQ-C30) as well as symptom burden (assessed using EORTC QLQ-H&N35) remained stable or slightly improved with nivolumab, while SOC patients had a decline in QOL. Statistical analysis showed significant between-group differences in physical functioning (P = 0.01 at 9 wk; P < 0.001 at 15 wk), role functioning (P = 0.003 at 9 wk; P < 0.001 at 15 wk), social functioning (P = 0.002 at 9 wk; P < 0.001 at 15 wk), pain (P < 0.001 at 9 wk; P = 0.02 at 15 wk), sensory problems (P = 0.01 at 9 wk; P < 0.001 at 15 wk), and social contact problems (P = 0.26 at 9 wk; P < 0.001 at 15 wk).
Biomarker effect:Biomarker effect on OS was evaluated after stratifying patients based on their PD-L1 expression status (≥ 1% vs < 1%). Among patients with PD-L1 ≥ 1%, median OS was 8.7 mo with nivolumab vs 4.6 mo with SOC (HR = 0.55; 95%CI: 0.36-0.83), whereas in patients with PD-L1 < 1%, median OS was 5.7 mo with nivolumab vs 5.8 mo with SOC (HR for death = 0.89; 95%CI: 0.54-1.45; P for interaction = 0.17). Post-hoc exploratory subgroup analysis based on p16 status was also done in this study. Among patients with p16 positive tumors, the median OS was 9.1 mo with nivolumab vs 4.4 mo with SOC (HR for death 0.56; 95%CI: 0.32-0.99), whereas, among patients with p16 negative tumors, the median OS was 7.5 mo with nivolumab vs 5.8 mo with SOC (HR =0.73; 95%CI: 0.42-1.25; P for interaction = 0.55).
Adverse events:In CheckMate 141, adverse events of grade 3 or more occurred in 13.1% of patients with nivolumab vs 35% with SOC. Two patients in the nivolumab arm and 1 patient in the control arm had treatment-related death. The most common adverse events (of any grade) with nivolumab were fatigue, nausea, decreased appetite, pruritis, and rash. Gastrointestinal side effects (primarily diarrhea) were less in the nivolumab group (6.8%) compared to SOC patients (14.4%), whereas adverse events of skin (rash and pruritus) were more common in the nivolumab group (15.7%) than in the SOC patients (12.6%). Endocrine system-related side effects (hypothyroidism) were also more with nivolumab (7.6%) compared to SOC (0.9%)[22].
KEYNOTE 040 (Pembrolizumab vs standard single-agent systemic therapy)
In this open-label phase-3 RCT, the investigators tested the efficacy and safety of the immune checkpoint inhibitor pembrolizumab (an anti-PD-1 monoclonal antibody) compared to standard therapy for the treatment of metastatic/recurrent head and neck cancer[23]. This was a multi-center study involving 97 medical centers across 20 countries. There were 247 patients in the intervention arm, while the control arm included 248 patients. Patients with platinum-refractory recurrent or metastatic (or both) HNSCC were included in this study. PD-L1 expression was assessed and categorized according to the tumor proportion score (≥ 50%vs< 50%) as well as the combined positive score (≥ 1vs< 1) The intervention arm received pembrolizumab 200 mg every 3 wk, while the control arm received investigator’s choice of standard doses of methotrexate (40 mg/m2IV weekly), docetaxel (75 mg/m2IV every 3 wk) or cetuximab (250 mg/m2IV weekly following a loading dose of 400 mg/m2).
Outcomes
OS:Primary outcome of the study was OS. The median OS was 8.4 mo (95%CI: 6.4-9.4) with pembrolizumabvs6.9 mo (95%CI: 5.9-8.0) with SOC (HR = 0.80; 95%CI: 0.65-0.98; nominalP =0.0161).
PFS:PFS was 2.1 mo (95%CI: 5.9-8.0) with pembrolizumabvs2.3 mo (95%CI: 2.1-2.8) with SOC (HR = 0.96; 95%CI: 0.79-1.16; nominalP =0.325).
ORR:ORR was 14.6% (95%CI: 10.4-19.6) with pembrolizumabvs10.1% (95%CI: 6.6-14.5) with SOC (nominalP =0.061).
Patient-reported outcomes:Results (published separately in another article) of an exploratory healthrelated quality of life analysis showed that at 15 wk, global health status/quality of life (GHS/QOL) scores were stable with pembrolizumab with a least square mean (LSM) of 0.39; 95%CI: -3.00-3.78), while GHS/QOL scores declined with SOC (LSM -5.86; 95%CI: -9.68 to -2.04). LSM between-group difference was 6.25 points (95%CI: 1.32-11.18: nominal 2-sidedP= 0.01)[32].
Biomarker effect:Cohenet al[23] found statistically significant interaction between PD-L1 expression [in terms of tumor proportion score (TPS) and combined positive score (CPS)] and treatment effect in KEYNOTE 040. Among patients with TPS ≥ 50%, median OS was 11.6 mo (95%CI: 8.3-19.5) with pembrolizumabvs6.6 mo (95%CI: 4.8-9.2) with SOC (HR = 0.53;95%CI: 0.35-0.81; nominalP= 00014). Among patients with TPS < 50%, OS was 6.5 mo (95%CI: 5.6-8.8) with pembrolizumabvs7.1 mo (95%CI: 5.7-8.1) with SOC (HR = 0.93;95%CI: 0.73-1.17; nominalP= 0.2675;Pfor interaction = 0.015). Similarly, among patients with CPS ≥ 1, median OS was 8.7 mo (95%CI: 6.9-11.4) with pembrolizumabvs7.1 mo (95%CI: 5.7-8.3) with SOC (HR = 0.74; 95%CI: 0.58-0.93; nominalP= 0.0049). Among patients with CPS < 1, OS was 6.3 mo (95%CI: 3.9-8.9) with pembrolizumabvs7.0 mo (95%CI: 5.1-9.0) with SOC (HR = 1.28; 95%CI: 0.8-2.07;P= 08476;Pfor interaction = 0.07). In terms of PFS, based on the modified RECIST1.1, for patients with TPS ≥ 50%, PFS was longer with pembrolizumab than with SOC, whereas for patients with CPS ≥ 1, PFS was slightly lower (3.6 mo) with pembrolizumab compared to SOC (4.8 mo). Among patients with CPS < 1 and those with TPS < 50%, PFS was longer for SOC compared to pembrolizumab[23].
Adverse events:In KEYNOTE 040, adverse events of grade 3 or more occurred in 13% of patients with pembrolizumabvs36.1% with SOC. Four patients in the pembrolizumab arm and 2 patients in the control arm had treatment-related death. While hypothyroidism was the most common treatmentrelated adverse event with pembrolizumab (13%), fatigue was the most common adverse event with SOC (18%)[23].
EAGLE study (durvalumab with or without tremelimumab vs standard single-agent systemic therapy)
Ferriset al[24] conducted an open-label phase-3 RCT among 736 patients with R/M HNSCC not amenable to curative therapy[24]. In this three-arm study (1:1:1), one of the intervention arms (n= 240, median follow-up 7.6 mo) received the anti PD-L1 agent durvalumab (10mg/kg every 2 wk), and the other intervention arm (n= 247, median follow-up 6.3 mo) received durvalumab (20 mg/kg every 4 wk-4 times followed by 10 mg /kg every 2 wk) plus the anti CTLA-4 agent tremelimumab (1 mg/kg every 4 wk-4 times). The control arm (n= 240 median follow-up 7.8 mo) received investigator’s choice of a standard single-agent [cetuximab, paclitaxel, docetaxel, methotrexate, 5-fluorouracil (5-FU), TS-1, or capecitabine] systemic therapy (SOC) dosed and administered according to local regulations.
Outcomes
OS:Primary outcome of the EAGLE study was OS. The median OS was reported as 7.6 mo (95%CI: 6.1-9.8) with durvalumabvs8.3 mo (95%CI: 7.3-9.2) with SOC (HR = 0.88; 95%CI: 0.72-1.08,P =0.20), whereas it was 6.5 mo (95%CI: 5.5-8.2) with durvalumab plus tremelimumabvs8.3 mo with SOC (HR = 1.04; 95%CI: 0.85-1.26,P =0.76).
PFS:PFS was 2.1 mo with durvalumab (95%CI: 1.9-3.0)vs3.7 mo (95%CI: 3.1-3.7) with SOC (HR = 1.02; 95%CI: 0.84-1.25,P =0.75). PFS with durvalumab plus tremelimumab was 2.0 mo (95%CI: 1.9-2.3)vs3.7 mo (95%CI: 3.1-3.7) with SOC (HR = 1.09; 95%CI: 0.90-1.33,P =0.54).
ORR:ORRs were 17.9% (95%CI: 13.3-23.3) with durvalumab monotherapy, 18.2% (95%CI: 13.6-23.6) with durvalumab plus tremelimumab, and 17.3% (95%CI: 12.8-22.5) with SOC.
Patient-reported outcomes:QOL measures were not assessed in the study.
Biomarker effect:In the EAGLE study, investigators measured PD-L1 expression in terms of percentage of tumor cell (TC). Among patients with TC ≥ 25%, the median OS was 9.8 mo (95%CI: 4.3-14.1) with durvalumab and 4.8 mo (95%CI: 3.3-6.4) with durvalumab plus tremelimumab, while SOC patients had an OS of 9.0 mo (95%CI: 6.8-11.0). Among patients with TC < 25%, the median OS with SOC was 8.0 mo (95%CI: 6.7-8.9), whereas it was 7.6 mo (95%CI: 6.2-9.5) with durvalumab and 7.8 mo (95%CI: 5.9-10.3) with durvalumab plus tremelimumab. In patients with TC ≥ 1%, both intervention groups had no difference in OS compared to SOC. In patients with TC < 1%, OS was higher with durvalumab compared to SOC, but no difference in OS was found between the durvalumab plus tremelimumab arm and the SOC arm.
Adverse events:In the EAGLE study, 10.1% of patients in the durvalumab arm, 16.3% patients in the durvalumab plus tremelimumab arm, and 24.2% patients in the control arm developed adverse events of grade 3 or more. Six patients died due to treatment-related issues: 4 with durvalumab, 2 with durvalumab plus tremelimumab, and 0 with SOC. Hypothyroidism was the most common treatmentrelated adverse event (of any grade) in the durvalumab (11.4%) arm as well as in the durvalumab plus tremelimumab arm (12.2%). Anemia was the most common treatment-related adverse event in the SOC arm (17.5%)[24].
Phase-3 studies evaluating ICI as first-line treatment in R/M HNSCC (I RCT: Keynote 048)
Prior to immunotherapy, the standard first-line treatment option for R/M HNSCC was the EXTREME regime, a combination of cetuximab, platinum (carboplatin or cisplatin), and 5-FU[13]. So far, one phase-3 trial has evaluated immunotherapy against the EXTREME regime in the first-line treatment setting for patients diagnosed with R/M HNSCC.
KEYNOTE 048 (pembrolizumab monotherapy vs EXTREME, pembrolizumab plus platinum-based CT vs EXTREME)
In this large three-arm RCT (n= 882), one of the intervention arms (n= 301, median follow-up: 11.5 mo) received pembrolizumab as monotherapy (pembrolizumab 200 mg once every 3 wk), while the second intervention arm (n= 281, median follow-up: 13.0 mo) received pembrolizumab (200 mg once every 3 wk) along with platinum-based chemotherapy {carboplatin [area under the curve (AUC) 5 mg/m2] or cisplatin (100 mg/m2) and 5-FU (1000 mg/m2for 4 consecutive d) every 3 wk}. The control arm (n= 300, median follow-up: 10.7 mo) received the EXTREME regime [cetuximab 400 mg/m2 loading dose, then 250 mg/m2 per week plus carboplatin (AUC 5 mg/m2) or cisplatin (100 mg/m2) and 5-FU (1000 mg/m2for 4 consecutive days) every 3 wk][25] (Table 1).
Outcomes
OS:The median OS (primary end point) was 11.6 mo (95%CI: 10.5-13.6) with pembrolizumab monotherapyvs10.7 mo (95%CI: 9.3-11.7) with EXTREME (HR = 0.85; 95%CI: 0.71-1.03;P =0.0456). In the pembrolizumab plus chemotherapy arm, median OS was 13.0 movs10.7 mo (95%CI: 9.3-11.7) in the EXTREME arm (HR = 0.77; 95%CI: 0.63-0.93;P =0.0034).
PFS:PFS was assessed as a primary outcome and was reported as 2.3 mo (95%CI: 2.2-3.3) with pembrolizumab monotherapyvs5.2 mo (95%CI: 4.9-6.0) with EXTREME (HR = 1.34; 95%CI: 1.13-1.59). In the pembrolizumab plus chemotherapy arm PFS was 4.9 mo (95%CI: 4.7-6.0)vs5.1 mo (95%CI: 4.9-6) in the EXTREME arm (HR = 0.92; 95%CI: 0.77-1.10;P= 0.169).
ORR:The pembrolizumab monotherapy arm had an ORR of 17% compared to 36% in the EXTREME arm. With pembrolizumab plus chemotherapy, ORR was similar to that with EXTREME (36%).
Biomarker effect:In KEYNOTE 048, PD-L1 expression was measured as CPS. For patients with CPS ≥ 20, median OS with pembrolizumab monotherapy was 14.9 movs10.7 mo with EXTREME (HR = 0.61; 95%CI: 0.45-0.83;P= 0.0007), while median OS with pembrolizumab plus chemotherapy was 14.7 movs11.0 mo with EXTREME (HR = 0.60; 95%CI: 0.45-0.82;P= 0.0004). Similarly, for patients with CPS ≥ 1, median OS with pembrolizumab monotherapy was 12.3 movs10.3 mo with EXTREME (HR = 0.78; 95%CI: 0.64-0.96;P= 0.0086), whereas OS was 13.6 mo in the pembrolizumab plus chemotherapy armvs10 .4 mo with EXTREME (HR = 0.65; 95%CI: 0.53-0.80;P< 0.0001).
For patients with CPS ≥ 20, median PFS with pembrolizumab monotherapy was 3.4 movs5.0 mo with EXTREME (HR = 0.99; 95%CI: 0.75-1.29;P= 0.456). Median PFS with pembrolizumab plus chemotherapy was 5.8 movs5.2 mo with EXTREME (HR = 0.73; 95%CI: 0.55-0.97;P= 0.0162). Similarly, for patients with CPS ≥ 1, median PFS with pembrolizumab monotherapy was 3.2 movs5.0 mo with EXTREME (HR = 1.16; 95%CI: 0.96-1.39), whereas PFS was 5.0 mo with pembrolizumab plus chemotherapyvs5.0 mo with EXTREME (HR = 0.82; 95%CI: 0.67-1.00).
Adverse events:In KEYNOTE 048, 55% patients in the pembrolizumab arm, 85% patients in the pembrolizumab plus chemotherapy arm, and 83% patients in the control arm developed grade 3 or more adverse events of any cause. Of these, treatment-related adverse events consisted of 17% in the pembrolizumab alone group, 72% in the pembrolizumab plus chemotherapy group, and 69% in the control group. While adverse events led to death in 8% of patients in the pembrolizumab arm and 12% of patients in the pembrolizumab plus chemotherapy arm, 10% in the control arm also died of adverse events.Major adverse events (of any grade) in the intervention groups were anemia, fatigue, hypothyroidism, and nausea[25].
Phase-3 studies evaluating ICI for treatment of LAHNSCC (I RCT: JAVELIN head and neck 100 trial)
The current SOC for the treatment of LAHNSCC is concurrent chemoradiation therapy (CRT)[33]. So far, only one phase-3 trial has investigated the usefulness of adding an ICI to concurrent CRT.
JAVELIN head and neck 100 trial (avelumab plus CRT vs placebo plus CRT)
The preliminary results of the study were presented in the 2020 European Society for Medical Oncology annual meeting by Cohenet al[26] followed by a recent journal publication[27].
This study (n= 697) was conducted among patients with previously untreated LA HNSCC who were eligible for definitive CRT with curative intent. The intervention arm (n= 350; median follow-up for PFS 14.6 mo, for OS 16.7 mo) received the PD-L1 inhibitor avelumab (10 mg/kg IV every 2 wk) plus CRT, which consisted of cisplatin (100 mg/m2every 3 wk) concurrently with intensity-modulated radiotherapy (standard fractionation of 70 Gy in 35 fractions over 7 wk). The control arm (n= 347; median follow-up for PFS 14.8 mo, for OS 16.8 mo) received placebo plus CRT (Table 1).
Outcomes
PFS:Median PFS (primary endpoint) was not reached in the intervention group or the control group. Statistical reports showed that hazard ratio (HR= 1.21; 95%CI: 0.93-1.5;one-sidedP =0.92) did not favor the avelumab plus CRT arm.
OS:OS was one of the secondary endpoints in this trial. Median OS was not reached in either study group. Statistical reports showed that the hazard ratio for death (HR = 1.31; 95%CI: 0.93-1.85; one-sidedP =0.937) did not favor the avelumab plus CRT arm.
ORR:Based on modified RECIST 1.1, ORR in the intervention arm was 74% (95%CI: 69-79) and that in the control arm was 75% (95%CI: 70-79) with an OR of 0.95 (95%CI: 0.66-1.35,P= 0.62).
Biomarker:Exploratory subgroup analysis of PFS based on PD-L1 expression showed that patients with PD-L1 ≥ 25% had an HR of 0.59 (95%CI: 0.28-1.22), while patients with PD-L1 < 25% had an HR of 1.37 (95%CI: 1.00-1.88) with avelumab plus CRT compared to placebo plus CRT (Pfor interaction = 0.03).
Adverse events:Treatment-related adverse events of grade 3 or more occurred in 80% of patients in the avelumab arm and in 74% of patients in the control arm. Serious adverse events occurred in 36% of patients in the intervention arm and in 32% of patients in the control arm. In the intervention arm, 7% of patients discontinued due to treatment-related adverse eventsvs3% in the control arm[27].
DISCUSSION
ICIs have emerged as a novel treatment strategy for HNSCC in recent years. The safety profile and antitumor activity of these agents demonstrated in early phase clinical trials paved the way for the initiation of several promising phase-3 trials in the field. Safety profile and clinical activity of pembrolizumab were first reported in KEYNOTE 012, an open-label phase 1b trial among patients with R/M HNSCC[34]. KEYNOTE 055, a phase-2 trial conducted among patients with platinum-resistant R/M HNSCC also reported manageable toxicity and an acceptable safety profile of pembrolizumab[35]. The study demonstrated a clinically meaningful anti-tumor activity of the agent in terms of ORRs and survival. These findings led to the initiation of KEYNOTE 040, the phase-3 trial investigating pembrolizumab for treating patients with platinum-refractory R/M HNSCC, and KEYNOTE 048, the phase-3 trial investigating pembrolizumab as first-line therapy in R/M HNSCC[23,25]. Similarly, two phase-2 trials, the HAWK study (a single-arm study investigating durvalumab monotherapy in R/M HNSCC with > 25% tumor PD-L1 expression) and the CONDOR phase-2 trial (an RCT investigating durvalumab with or without tremelimumab in PD-L1 Low/negative R/M HNSCC) served as the rationale for investigating combination immunotherapy regimens in platinum-refractory R/M HNSCC and to initiate the EAGLE study[24,36,37]. Studies on the effectiveness of nivolumab in other solid tumors supported the initiation of CheckMate 141 trial, the first phase-3 trial of nivolumab among patients with platinum-resistant R/M HNSCC[22,38]. Chemotherapy and radiotherapy, alone or in combination, have demonstrated potential synergetic effects when combined with immunotherapy in early phase studies. This phenomenon and the proven effectiveness of the anti-PD-L1 agent avelumab in other advanced solid tumors paved the way to the JAVELIN head and neck 100 trial, the first phase-3 RCT to investigate the effectiveness of combining ICI with chemoradiation in locally advanced head and neck cancer[27,39,40].
In this systematic review, we included the published phase-3 clinical trials evaluating the effectiveness of ICIs in HNSCC. Five studies met our eligibility criteria. Three studies (CheckMate 141, KEYNOTE 040, and EAGLE study) evaluated ICI as second-line treatment for R/M HSCC, one study (KEYNOTE 048) evaluated ICI as first-line treatment for R/M HSCC, while one phase-3 trial (JAVELIN head and neck 100 trial) evaluated the effectiveness of immunotherapy in LAHNSCC[22-27].
Effectiveness of ICI for R/M HNSCC in the second-line treatment setting
In the second-line treatment setting, nivolumab in CheckMate 141 and pembrolizumab in KEYNOTE 040 demonstrated promising outcomes among patients with platinum-refractory R/M HNSCC[22,23]. In CheckMate 141, the anti-PD-1 agent nivolumab showed a statistically significant 31% reduction in risk of death (HR = 0.69,P =0.01) and a net gain of 2.4 mo in terms of OS. A 2.3-fold increase in ORR was also reported with nivolumab compared to SOC. A favorable toxicity profile was another finding with nivolumab, with lower rates of treatment-related adverse events of grade 3 or more compared to SOC (13.1%vs35%). Patient-reported QOL measures remained stable with nivolumab, while a decline in QOL occurred among the control patients. However, the study did not demonstrate any significant PFS benefits with nivolumab (HR = 0.89, 95%CI: 0.70-1.13;P =0.32). Regarding the impact of biomarkers, survival benefit with nivolumab was found to be irrespective of PD-L1 expression (Pfor int. = 0.17) in the subgroup analyses based on PD-L1 status, although patients with PD-L1 ≥ 1% had a better magnitude of effect (HR = 0.55) than those with PD-L1 < 1 (HR = 0.89)[22,41,42]. Similarly, based on the post-hoc exploratory subgroup analysis according to p16 status, the investigators concluded that the longer median OS with nivolumab was irrespective of the p16 status (Pfor interaction = 0.55).
In KEYNOTE 040, the anti-PD-1 agent pembrolizumab demonstrated statistically significant improvement in OS with a 20% reduction in risk of death (HR = 0.80,P= 0.016) compared to SOC in the overall study population[23]. Higher ORR (14.6%vs10.1%, nominalP= 0.061) and lower rates of adverse events of grade 3 or more (13%vs36.1%) were also demonstrated with pembrolizumab compared to SOC. At 15 wk, stable GHS/QOL scores were reported with pembrolizumab, while the control patients had a decline in QOL. The study did not, however, demonstrate any PFS benefits with pembrolizumab (HR = 0.96, nominalP= 0.325) compared to SOC. Exploratory subgroup analyses based on PD-L1 expression demonstrated statistically significant interactions between treatment effects and PD-L1 status. For patients with TPS ≥ 50% and CPS > 1, the treatment effects of pembrolizumabvsSOC were found to be higher than in those with TPS < 50% and CPS < 1[23]. For instance, in terms of OS, patients with TPS ≥ 50% had a net gain of 5 mo with a 47% reduction in risk of death with pembrolizumab compared to SOC (HR = 0.53, nominalP= 00014), suggesting PD-L1 expression may be explored as a predictive biomarker while selecting patients for pembrolizumab therapy. Based on the findings of CheckMate 141 and KEYNOTE 040, nivolumab and pembrolizumab were approved as standard second-line treatment options for platinum-resistant R/M HNSCC[22,23,43].
The EAGLE study did not detect any statistically significant improvements in OS with durvalumab (HR = 0.88,P= 0.20) or with durvalumab plus tremelimumab (HR = 1.04,P= 0.76) compared to SOC. Again, there were no significant benefits in terms of PFS with durvalumab or with durvalumab plus tremelimumab, compared to SOC. However, investigators of EAGLE have postulated that control patients in the study had an unexpectedly high OS as the data were confounded by discrepancies in performance status favoring the control arm. Option of using paclitaxel as SOC (paclitaxel was not an option in the other two studies in the second-line setting), and subsequent immunotherapy after discontinuation of SOC treatment by control patients were also mentioned as reasons for this finding[24]. Although the primary objectives were not met, one positive finding was that the rates of adverse events of grade 3 or more were lower with immunotherapy compared to SOC.
Effectiveness of ICI for R/M HNSCC in the first-line treatment setting
In the first-line treatment setting, in KEYNOTE 048, pembrolizumab with platinum-based chemotherapy demonstrated statistically significant improvements in OS (13.0vs10.7 mo) with a 23% reduction in risk of death (HR = 0.77, P= 0.0034) compared to cetuximab plus platinum-based chemotherapy (EXTREME) in the total population. Pembrolizumab monotherapy was found to be noninferior to EXTREME (HR = 0.85; 95%CI: 0.71-1.03;P= 0.0456) in terms of OS (11.6 movs10.7 mo) in the total population. No significant impact on PFS was detected with pembrolizumab alone or pembrolizumab with chemotherapy compared to EXTREME in the overall population. Pembrolizumab alone had a lower ORR (17%) compared to EXTREME (36%), while pembrolizumab plus chemotherapy had an ORR (36%) like that of EXTREME. Interestingly, biomarker (PD-L1) based stratified analysis demonstrated superiority in terms of OS in the CPS ≥ 20 and CPS ≥ subgroups with pembrolizumab alone as well as with pembrolizumab plus chemotherapy compared to EXTREME. For instance, within the CPS ≥ 20 population, pembrolizumab monotherapy compared to EXTREME resulted in a net gain of 4.2 mo in terms of OS (14.9 movs10.7 mo) with a highly significant 39% reduction in risk of death (HR = 0.61,P= 0.0007). In the CPS ≥ subgroup pembrolizumab monotherapy also demonstrated superiority in terms of OS (12.3 movs10.3 mo) compared to EXTREME (HR = 0.78,P= 0.0086), indicating that pembrolizumab monotherapy is a suitable treatment option for PD-L1 positive R/M HNSCC. Similarly, in both subgroups, pembrolizumab with chemotherapy resulted in statistically significant improvements in OS compared to EXTREME. For instance, R/M HNSCC patients with CPS ≥ 20 had a highly significant 40% reduction in risk of death with pembrolizumab plus chemotherapy compared to EXTREME (HR = 0.60,P= 0.0004). Patients with CPS ≥ 1 also had a significant reduction in risk of death with pembrolizumab plus chemotherapy compared to EXTREME (HR = 0.65,P< 0.0001). These findings indicate that tumor PD-L1 expression can be a predictive biomarker for identifying patients who will benefit from pembrolizumab[25,44].
Based on the findings from KEYNOTE 048, pembrolizumab monotherapy was approved as an appropriate SOC for PD-L1 positive R/M HNSCC, and pembrolizumab plus platinum-based chemotherapy became the new SOC for the treatment of R/M HNSCC in the first-line setting[25,43]. In this study, rates of treatment-related adverse events of grade 3 or more were lower with pembrolizumab monotherapy (17%) compared to EXTREME (69%). However, rates of treatment-related adverse events of grade 3 or more were noticeably high (72%) in the combination therapy arm[25]. This finding highlights the importance of weighing up the survival benefits of the pembrolizumab plus chemotherapy regime against its adverse events profile while making treatment decisions for patients with R/M HNSCC.
Effectiveness of ICI in LAHNSCC
Regarding immunotherapy in LAHNSCC, there is no definite evidence of benefit according to the primary results of the JAVELIN study[26,27]. The combination of avelumab and CRT did not demonstrate any beneficial outcomes in terms of PFS or OS over placebo plus CRT, and based on the modified RECIST 1.1, there were no ORR benefits (74%vs75%) either. Moreover, avelumab plus CRT resulted in slightly higher rates of adverse events of grade 3 or more compared to CRT plus placebo (80%vs74%). As an explanation for the absence of PFS benefits, the investigators postulated that the dysfunction of T cells or changes in the tumor microenvironment after radiotherapy might have reduced the ability of the immune system to eliminate the microscopic disease. A recent phase-2 randomized trial of pembrolizumab with radiation therapy against cetuximab with radiotherapy in LAHNSCC also failed to demonstrate significant treatment benefits, although the combination therapy had a favorable toxicity profile[45]. Similarly, a previous randomized phase-2 trial of nivolumab with stereotactic body radiotherapy compared to nivolumab alone did not result in tumor shrinkage in R/M HNSCC[46]. Interestingly, an exploratory subgroup analysis of patients with high PD-L1 expression in the JAVELIN study indicated a potential PFS benefit with avelumab plus CRT compared to placebo plus CRT. Although definite conclusions cannot be made based on this small subgroup analysis, this is a finding that should be explored further to understand the role of biomarker analysis to select patients for immunotherapy.
In terms of PFS, none of the studies included in this review demonstrated any beneficial outcomes. A recent meta-analysis by Gyawaliet al[47] found no correlation between median OS and median PFS in studies evaluating anti-PD-1 agents. Defining PFS based on the traditional RECIST criteria (developed in the pre-immunotherapy era) that do not properly capture the concept of disease progression with immunotherapy was hypothesized as a probable reason for the finding.
While immunotherapy involving anti-PD-1 checkpoint inhibitors resulted in significant improvements in survival, PD-L1 and CTLA-4 blockade did not demonstrate any encouraging outcomes. More studies are needed to build evidence on the role of anti-PD-L1 and CTLA-4 blocking agents in the treatment of advanced HNSCC. Again, in the first-line setting, the evidence on the effectiveness of immunotherapy for R/M HNSCC is based on one single phase-3 trial (KEYNOTE 048), and currently, pembrolizumab is the only ICI approved for treating this group of patients[25]. During our literature search, we identified some of the ongoing phase-3 clinical trials investigating various checkpoint inhibitor agents either alone or as part of combination therapy. Subsequently, we searched the ‘clinical trials.org’ database and identified the major ongoing clinical trials and confirmed the status of those trials.
Major ongoing clinical trials
Studies investigating the combination of two different ICI agents or ICI in combination with another immunomodulatory agent in R/M HNSCC in the first-line treatment setting[48-51]:An ongoing openlabel phase-3 trial (KESTREL) is currently evaluating anti-PDL-1 agent durvalumab alone and in combination with the anti-CTLA-4 agent tremelimumab for R/M HNSCC against the EXTREME regime in the first-line treatment setting[48]. Checkmate 651, another ongoing phase-3 study, is currently evaluating the anti-PD-1 agent nivolumab in combination with the CTLA-4 blocking agent ipilimumab for R/M HNSCC against the EXTREME regime in the first-line setting[49]. In a phase-3 trial among R/M HNSCC, patients with a PD-L1 biomarker expression of CPS ≥ 1, the combination of pembrolizumab and lenvatinib, an anti-vascular endothelial growth factor-multiple kinase inhibitor, is being investigated as first-line treatment against pembrolizumab plus placebo[50]. Similarly, ICI in combination with another immunomodulatory agent is being investigated in the ECHO-304/KEYNOTE 669 study[51]. In this phase-3 trial, the combination of pembrolizumab and epacadostat, an indoleamine 2,3-dioxygenase 1, inhibitor agent is being investigated against pembrolizumab monotherapy, and the EXTREME regime, in R/M HNSCC as first-line treatment[51].
Studies investigating ICI plus CRT vs CRT alone in LAHNSCC[52,53]:In KEYNOTE 412,the effectiveness of pembrolizumab given concurrently with CRT and as maintenance therapy is being evaluated against placebo plus standard CRT for the treatment of LAHNSCC[52]. In REACH, the superiority of avelumab in combination with RT-cetuximab compared to cisplatin -RT and/or to RT-cetuximab alone is being evaluated[53].
Studies investigating ICI plus RT vs cetuximab plus RT in platinum ineligible LAHNSCC[54,55]:In HN004, durvalumab plus RT is being compared to cetuximab plus RT in platinum ineligible patients[54]. In a recently completed phase-3 trial with no published results (CheckMate 9TM), cisplatinineligible patients received nivolumab plus RT as intervention while control patients received cetuximab plus RT[55].
Studies investigating ICI as neoadjuvant/adjuvant therapy[56-59]:In KEYNOTE 689, pembrolizumab with RT (with or without cisplatin) before and after surgery is compared to RT (with or without cisplatin) given after surgery[56]. Atezolizumab, an anti-PD-L1 agent, is being evaluated as an adjuvant therapy against placebo in the ongoing trial iMvoke010[57]. In IMSTAR-HN, nivolumab alone or in combination with the anti-CTLA-4 agent ipilimumab is evaluated as follow-up after adjuvant therapy against standard follow-up in surgically resectable LAHNSCC[58]. In NIVOPOSTOP, the efficacy of postoperative adjuvant nivolumab along with CRT is compared to post-operative CRT alone[59].
The details of these ongoing phase-3 studies are given in Table 2.
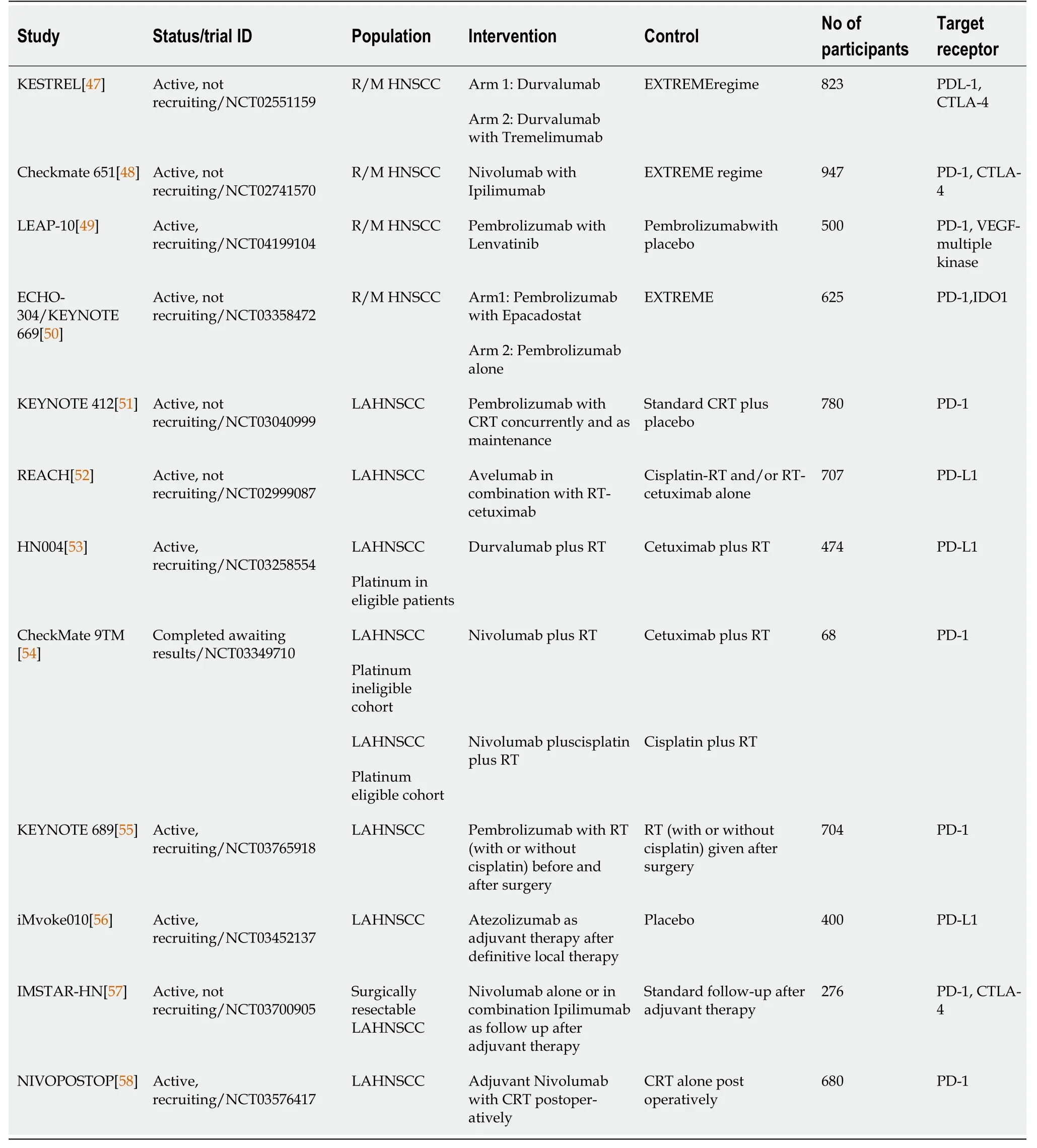
Table 2 Major ongoing phase-3 studies investigating immunotherapy in head and neck squamous cell carcinoma
Future directions
Novel combination strategies to potentiate and prolong the anti-tumor activity of ICI are being evaluated currently. Thus, several early phase clinical trials (phase 1/2) investigating combination strategies of ICIs and other novel immunomodulatory agents are in the pipeline[60,61]. For example, a randomized phase-2 trial to study the safety and tolerability of nivolumab administered alone or in combination with relatlimab (antibody targeting the novel immunomodulatory receptor lymphocyte activation gene-3) or the anti-CTLA-4 agent ipilimumab is currently ongoing among patients with locally advanced surgically resectable HNSCC[62]. Immune biomarker modulation in response to nivolumab given along with Toll-like receptor 8 agonist motolimod is being analyzed in an ongoing phase-1b pre-operative biomarker trial[63]. Combination of pembrolizumab and the vascular endothelial growth factor-multiple kinase inhibitor lenvatinib demonstrated good anti-tumor activity and manageable toxicity among R/M HNSCC patients in a phase-1b/2 trial, and LEAP 010, a phase-3 trial of this combination strategy is currently ongoing[50,64]. The combination of pembrolizumab and the anti-EGFR agent cetuximab had demonstrated encouraging outcomes in the interim analysis of an ongoing multi-arm phase-2 trial[65,66]. A recently completed study among R/M HNSCC patients investigating pembrolizumab in combination with epacadostat has shown clinically meaningful results, and a larger phase-3 trial (ECHO 304/KEYNOTE 669) of this combination strategy is ongoing currently[51,67]. Combination therapy of pembrolizumab with the EGFR-tyrosine kinase inhibitor afatinib, which also included predictive biomarker analysis, had been evaluated recently in a phase-2 clinical trial (the ALPHA study) in R/M HNSC[68]. The study demonstrated augmentation of the anti-tumor activity of pembrolizumab by afatinib, and the results of biomarker analysis suggested that PD-L1 and EGFR amplification could be predictive biomarkers for cancer immunotherapy. EACH, a randomized phase-2 trial among R/M HNSCC is investigating the superiority of avelumab and cetuximab combination compared to avelumab monotherapy[69]. Another recently completed early phase study on the combination of pembrolizumab with the therapeutic vaccine talimogene laherparepvec demonstrated a tolerable safety profile among patients with R/M HNSCC. However, this investigation did not progress into a phase-3 trial as the efficacy of the combination was found to be similar to pembrolizumab monotherapy[70].
Immunotherapy trials among patients with p16-positive head and neck cancer (oropharyngeal squamous cell carcinoma) are also currently underway. In this group of patients, p16 positivity is a known independent predictive biomarker for survival[71]. The efficacy and tolerability of the combination of ipilimumab (anti-CTLA-4) and nivolumab (anti-PD-1) along with RT in locoregionally advanced human papilloma virus-positive oropharyngeal squamous cell carcinoma are being evaluated in an ongoing phase-2 single-arm trial[72]. Another phase-2 randomized study (KEYCHAIN trial) is investigating RT along with concurrent and adjuvant pembrolizumab against concurrent chemoradiation among p16-positive HNSCC[73,74].
Regarding biomarkers, in addition to p-16 positivity and PD-L1 expression, other biomarkers like microsatellite instability (MSI) and tumor mutation burden were also found to be associated with favorable outcomes with ICI therapy in HNSCC[75]. Tardyet al[76] recently reported a case of complete response to anti-PD-L1 therapy in HNSCC in a patient with high tumor MSI (MSI-H) and a negative PD-L1 histochemical status. Similarly, Hannaet al[77] reported that higher tumor mutation burden predicted response to ICI and better treatment outcomes in virus-negative head and neck cancer. Again, some subtypes of tumor-infiltrating lymphocytes (TILs) such as PD-1+TIM-3+CD8+TILs and PD-1+LAG-3+CD8+TILs have also predicted treatment response to ICIs[75,77]. The data on these emerging predictive biomarkers is still not conclusive; therefore, further research is essential. PRECISION 01, an ongoing prospective observational study is currently evaluating biomarker signatures in tissue samples of platinum-refractory HNSCC patients who received nivolumab monotherapy; the findings may contribute to the knowledge on predictive biomarkers for ICIs[78].
In future studies, patient-reported outcomes like QOL should be evaluated meticulously since such outcomes are very crucial for advanced HNSCC patients and their families[79,80]. Cost-effectiveness is another issue to be considered before including ICIs in the routine treatment guidelines for patients from developing countries and resource-poor settings[81,82]. The impact of factors like age, comorbidities, and performance status on outcomes of patients receiving immunotherapy also needs to be determined[83].
Limitations/strengths
There are very few published phase-3 clinical trials evaluating checkpoint inhibitor immunotherapy among patients diagnosed with HNSCC, and the evidence we gathered in this review is based on the five phase-3 RCTs published so far. A previous systematic review on this topic included eight studies, of which two were phase-3 RCTs[84]. Wanget al[85] conducted a systematic review and meta-analysis of nine studies on the effectiveness of checkpoint inhibitors in HNSCC, of which two were phase-3 trials.
To our knowledge, this is the first systematic review conducted on the effectiveness of ICIs in HNSCC incorporating phase-3 trials alone. The evidence we presented based on the five studies in this review will help the practicing clinicians to make informed decisions. We further explored the literature and identified a variety of promising clinical studies that are ongoing currently focusing on combination strategies in enhancing and prolonging the anti-tumor effects of ICIs. We also identified the gaps in knowledge on some important issues such as predictive biomarkers and about the identification of patients who will benefit from immunotherapy based on biomarker assessment[86,87].
CONCLUSION
ICIs have shown improved survival outcomes with acceptable toxicity profile in R/MHNSCC in the first and second-line treatment settings. The marginal improvement in survival should be weighed against the cost of these therapeutic agents and the QOL of patients. While anti-PD-1 agents demonstrated efficacy, evidence on the effectiveness of anti-PD-L1 and anti-CTLA-4 agents is lacking. There is no proven efficacy in the curative setting to date. The ongoing clinical trials may better define the role of ICI in R/M HNSCC and LAHNSCC in the future.
ARTICLE HIGHLIGHTS
Research background
Head and neck squamous cell carcinoma (HNSCC) is one of the major causes of cancer-associated morbidity and mortality globally, especially in developing countries. Treatment approaches for HNSCC vary according to the stage of the disease at presentation. For recurrent/metastatic HNSCC (R/M HNSCC), platinum-based chemotherapy was the only available treatment option until recently. A relatively new systemic therapy option that emerged in recent years in the treatment of advanced HNSCC is immunotherapy using immune checkpoint inhibitors (ICI).
Research motivation
Advanced HNSCCs are often associat ed with significant functional limitations, and aggressive treatment may adversely affect the quality of life of these patients who are already suffering from the effect of advanced cancer. The median survival of R/M HNSCC patients receiving platinum-based chemotherapy is 7.4 mo. Some patients become refractory to platinum and die within a period of 4 mo.The safety profile and anti-tumor activity of ICIs demonstrated in early phase clinical trials paved the way to the initiation of several promising phase-3 trials in the field. Therefore, we decided to gather the current evidence on the effectiveness of these agents in advanced head and neck cancer based on the findings from phase-3 clinical trials of ICI published so far. We also wanted to examine the feasibility of incorporating these agents into routine clinical practice in resource-poor settings.
Research objectives
The objective of this systematic review was to gather the evidence from phase-3 randomized controlled trials (RCTs) evaluating the effectiveness of immunotherapy among patients with advanced HNSCC.We aimed to synthesize the evidence from the published phase-3 studies that investigated the efficacy and toxicity profile of ICIs administered either alone or in combination with chemotherapy, radiation therapy, or with another checkpoint inhibitor, in advanced HNSCC.
Research methods
We conducted this systematic review according to the PRISMA (preferred reporting items for systematic reviews and meta-analyses) guidelines. We searched four major databases including PubMed, Scopus, Embase, and COCHRANE library, without any language limit. A combination of standardized search terms and keywords including head and neck squamous cell carcinoma, recurrent, metastatic, locally advanced, immunotherapy, checkpoint inhibitors, monoclonal antibodies, programmed cell death protein-1 (PD-1), programmed death-ligand 1 (PD-L1), cytotoxic T- lymphocyte associated protein-4 (CTLA-4), and phase-3 clinical trial were used for searching the literature. Studies were included if they were completed phase-3 RCTs conducted among patients with R/M HNSCC or LAHNSCC, in which the intervention patients received ICI either alone or in combination with chemotherapy, radiation therapy, or with another ICI and the control patients received the standard of care treatment (SOC). Anatomical sites of primary tumors were oral cavity, oropharynx, hypopharynx, and larynx in the included studies.
Research results
Five phase-3 clinical trials have reported the data on the effectiveness of immunotherapy in HNSCC so far: Four in R/M HNSCC and one in LAHNSCC. In patients with R/M HNSCC, anti-PD-1 agents nivolumab and pembrolizumab demonstrated improvement in overall survival (OS) in the second-line treatment setting compared to the SOC. While the net gain in OS with nivolumab was 2.4 mo, that with pembrolizumab was 1.5 mo. However, the study that investigated the anti-PD-L1 agent durvalumab with or without the anti-CTLA-4 agent tremelimumab in the second-line treatment setting did not demonstrate any beneficial outcomes.
In the first-line setting, pembrolizumab together with platinum-based chemotherapy demonstrated statistically significant improvement in survival with a net gain in OS of 2.3 mo in the overall population and a net gain in OS of 4.2 mo in the population with a combined positive score of > 20 compared to the SOC treatment. Pembrolizumab monotherapy was found to be non-inferior to EXTREME in terms of OS (11.6 movs10.7 mo) in the total population. In patients with PD-L1 positive R/M HNSCC, monotherapy with pembrolizumab also demonstrated statistically significant improvement in survival compared to SOC. In LAHNSCC, immunotherapy using the anti-PD-L1 agent avelumab along with standard chemoradiation therapy did not result in improved outcomes compared to placebo plus chemoradiation therapy.
Research conclusions
This systematic review helped us to conclude that anti-PD-1 agents provide survival benefits in R/M HNSCC in the first and second-line settings with manageable toxicity profiles. However, it is important to weigh the marginal survival benefits provided by these therapeutic agents against their cost, especially in resource-poor settings. The review showed that the evidence on the effectiveness of anti-PD-L1 and anti-CTLA-4 agents in advanced head and neck cancer is lacking. To date, there is no evidence on the effectiveness of ICIs in the curative setting either. We believe that the ongoing clinical trials (discussed in the article) will help to define better the role of ICI in R/M HNSCC and LAHNSCC in the future.
Research perspectives
Novel combination strategies to potentiate and prolong the anti-tumor activity of ICI are being evaluated currently. Gaps in knowledge exist on some important issues such as predictive biomarkers, and about the identification of patients who will benefit from immunotherapy based on biomarker assessment. Future studies should focus on these issues.
ACKNOWLEDGEMENTS
The authors would like to thank Dr. Vijo Poulose for his assistance in searching the databases.
FOOTNOTES
Author contributions:Kainickal CT contributed to conceptualization; Poulose JV contributed to the methodology and literature search; Both authors participated in drafting and critically revising the manuscript.
Conflict-of-interest statement:Authors have nothing to disclose.
PRISMA 2009 Checklist statement:The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:India
ORCID number:Jissy Vijo Poulose 0000-0002-1773-8699; Cessal Thommachan Kainickal 0000-0003-3149-3074.
Corresponding Author's Membership in Professional Societies:Association of Radiation Oncologists of India, No. 1058.
S-Editor:Gong ZM
L-Editor:Filipodia
P-Editor:Gong ZM
 World Journal of Clinical Oncology2022年5期
World Journal of Clinical Oncology2022年5期
- World Journal of Clinical Oncology的其它文章
- Commentary: Evaluating potential glioma serum biomarkers, with future applications
- How to improve metastatic pancreatic ductal adenocarcinoma patients’ selection: Between clinical trials and the real-world
- Assessing optimal Roux-en-Y reconstruction technique after total gastrectomy using the Postgastrectomy Syndrome Assessment Scale-45
- Modified binding pancreaticogastrostomy vs modified Blumgart pancreaticojejunostomy after laparoscopic pancreaticoduodenectomy for pancreatic or periampullary tumors
- Survival characteristics of fibrolamellar hepatocellular carcinoma: A Surveillance, Epidemiology, and End Results database study
- Co-relation of SARS-CoV-2 related 30-d mortality with HRCT score and RT-PCR Ct value-based viral load in patients with solid malignancy
