Effect of hepatic artery resection and reconstruction on the prognosis of patients with advanced hilar cholangiocarcinoma
lNTRODUCTlON
Hilar cholangiocarcinoma (HC) is the most common type of cholangiocarcinoma, arising from the epithelium of the bile duct mucosa above the cystic duct opening[1-4]. Operation is the only measure to improve prognosis[5]. However, the procedure can be extremely challenging due to the anatomic parts involved and important adjacent structures[6,7]. Invasion of the hepatic artery corresponds to advanced disease, limiting radical resection and increasing the incidence of postoperative complications, such as abdominal bleeding, infection, and liver failure[8]. In some cases, compromise of the hepatic artery may not be due to true invasion, but due to compression of the artery by the enlarging tumor. Combined vascular resection in advanced HC is proposed by many authors, with notable rates of successful surgical outcomes[9]. How to effectively reduce the incidence of postoperative complications and improve radical cure has become a topic of intense clinical interest. Currently, there is a paucity of research about the impact of hepatic artery resection and reconstruction for advanced HC. If the hepatic artery is invaded, radical excision cannot be performed, and only palliative surgery is offered with the goal of symptom relief and definitive treatment[10,11]. Resection and reconstruction of the affected hepatic artery and portal vein can be combined with resection of the affected lateral liver, to improve surgical outcomes. Our study aimed to determine the effect of hepatic artery resection and reconstruction in patients with advanced HC, and to provide some clinical guidance.
MATERlALS AND METHODS
Data
A total of 98 patients with HC who underwent radical operation in our hospital from February 2015 to June 2018 were selected for this retrospective analysis. According to whether the patients underwent hepatic artery resection and reconstruction or not, they were divided into reconstruction (
= 40) and control (
= 58) groups. Inclusion criteria were as follows: (1) Age: 19-75 years; (2) American Society of Anesthesiologists Classification grade I-III; (3) HC diagnosed through abdominal computed tomography, magnetic resonance imaging, or endoscopic retrograde cholangiopancreatography; (4) Bismuth-Corlette type I-IV; (5) Follow up data for at least two years; and (6) Study plan that does not violate the requirements of relevant medical ethics. Exclusion criteria include: (1) Presence of concurrent extrahepatic malignancy; (2) Previous history of hepatobiliary surgery due to other reasons; (3) Serious comorbidities (cerebrovascular accident, acute myocardial infarction,
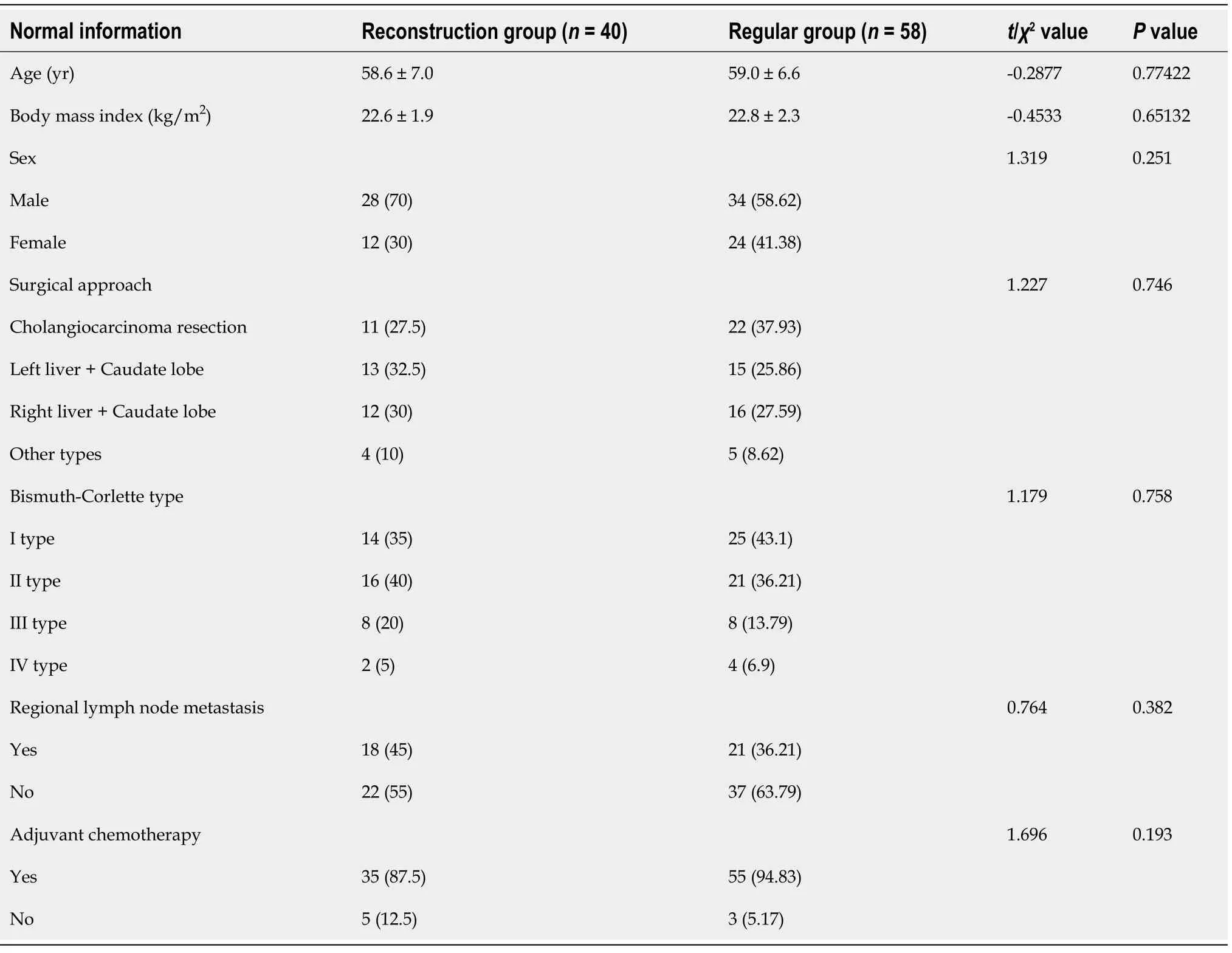
); and (4) Lack of data. The two groups were comparable in their baseline characteristics as shown in Table 1.
Surgical method
The control group underwent routine radical surgery. After general anesthesia, a reverse "L"-shaped incision was made below the right costal margin to explore the tumor, then the hepatic artery and portal vein under the duodenal ligament were separated. The common bile duct was cut open, and the gallbladder was dissociated and pulled upward together with the common bile duct. Nerves and lymph nodes were removed from top down to expose and skeletonize the hepatic artery and portal vein. The location and state of the tumor were evaluated, and invasion of the confluence of the hepatic and bile ducts was carefully determined. Liver lobectomy was performed, the contralateral bile duct was cut open at 0.5 cm of the tumor margin, and the hepatic artery and portal vein on the affected side were resected together with the lesion. Prophylactic antibiotics and hydration were administered as per postoperative protocol.
The reconstruction group underwent combined hepatectomy and hepatic artery reconstruction under general anesthesia. A reverse "L"-shaped incision was made below the right costal margin to explore the tumor, then the hepatic artery and portal vein under the duodenal ligament were separated. Sixteen groups of lymph nodes were examined after the abdominal resection, in order to determine whether there was metastasis to the peritoneum and liver. The bile duct was cut off behind the duodenum, the tumor was dissociated toward the head direction, and the lymph nodes and connective tissue of the hepatic duodenal ligament were completely removed. If the bile duct margin was negative, the dissected portal vein was resected and ligated. The liver was then cut through by a phacoemulsification suction knife. The opposite lateral bile duct was resected and biliary drainage tubes were inserted and fixed. The tumor and affected artery were resected together, and 70 Prolene sutures were used to reconstruct the hepatic artery through interrupted anastomosis. The reconstruction method was based on arterial invasion length, and included reconstruction using a great saphenous vein graft and in situ reconstruction after resection of the involved artery. If there was no evidence of bleeding within 24 h, 4000 IU of low-molecular-weight heparin sodium was administered subcutaneously once daily for 3-5 d. Antiplatelet therapy with clopidogrel was initiated after initiation of oral intake.
Monitoring parameters
The operation time, operation blood loss, length of hospital stay, postoperative gastrointestinal function recovery time, R0 resection rate, serum alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin (TBIL), Karnofsky performance status (KPS) score, surgical complications, twoyear survival rate and survival time between the two groups were statistically analyzed.
Morning fasting venous blood samples (3 mL) were collected from all the participants and centrifuged at 3000 r/min at room temperature for 5 min to separate the serum. Hitachi 7170 automatic biochemical analyzer was used to measure the serum ALT, AST, and TBIL levels. Alanine aminotransferase was > 40 U/L, AST > 35 U/L, and TBIL > 22 μmol/L, which were considered abnormal[12,13].
IN OLD times when wishing still helped one, there lived a king whose daughters were all beautiful, but the youngest was so beautiful that the sun itself, which has seen so much, was astonished whenever it shone in her face. Close by the King s castle1 lay a great dark forest,2 and under an old lime-tree in the forest was a well, and when the day was very warm, the King s child went out into the forest and sat down by the side of the cool fountain,3 and when she was dull she took a golden ball,4 and threw it up on high and caught it, and this ball was her favorite plaything.
There are many people who do not agree in this circumstance,33 and pretend that Little Thumb never robbed the Ogre at all, and that he only thought he might very justly, and with a safe conscience, take off his boots of seven leagues, because he made no other use of them but to run after little children. These folks affirm that they are very well assured of this, and the more as having drunk and eaten often at the fagot-maker s house. They aver56 that when Little Thumb had taken off the Ogre s boots he went to Court, where he was informed that they were very much in pain about a certain army, which was two hundred leagues off, and the success of a battle. He went, say they, to the King, and told him that, if he desired it, he would bring him news from the army before night.
Statistical analysis
Statistical analysis was carried out using SPSS 21.0. Measurement of data, such as operation time, operation blood loss, and length of hospital stay in the two groups were expressed as mean ± SD;
test was used for comparison between the two groups;
test was used to compare categorical variables between the groups. The Kaplan-Meier method was used for survival analysis.
< 0.05 was considered statistically significant.
RESULTS
Comparison of surgical trauma indices between the two groups
The operation time, operation blood loss, length of hospital stay, and postoperative gastrointestinal function recovery time in the reconstruction group were higher than those of the control group (
< 0.05, Table 2).
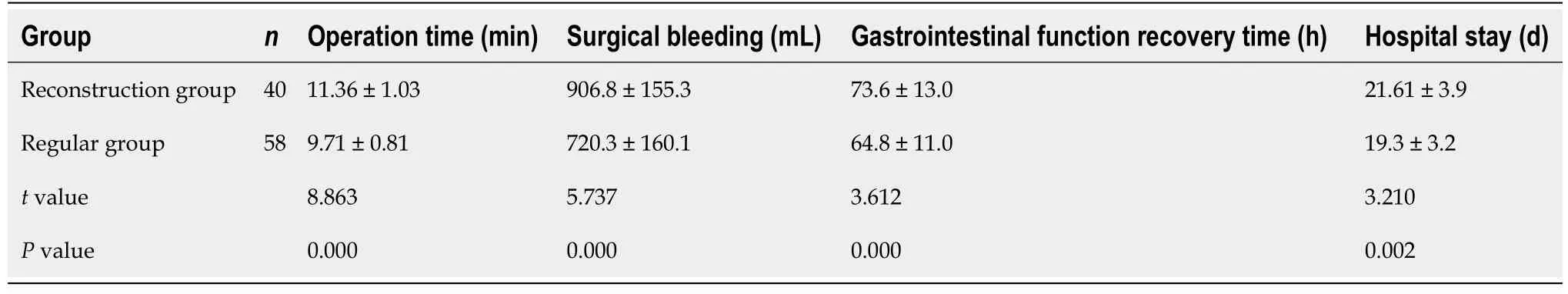
Comparison of operational resection margin between the two groups
The R0 resection was achieved in 90.00% of the reconstruction group and 72.41% of the control group, with a statistically significant difference (
< 0.05, Table 3).
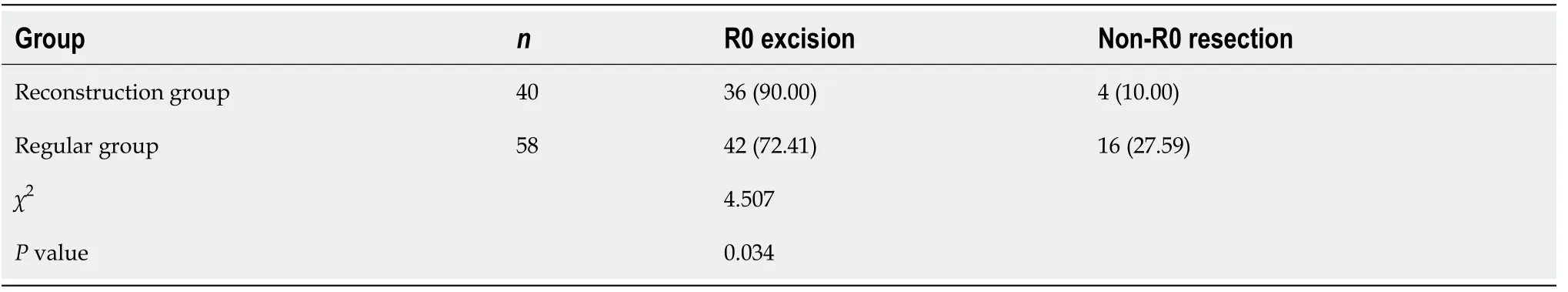
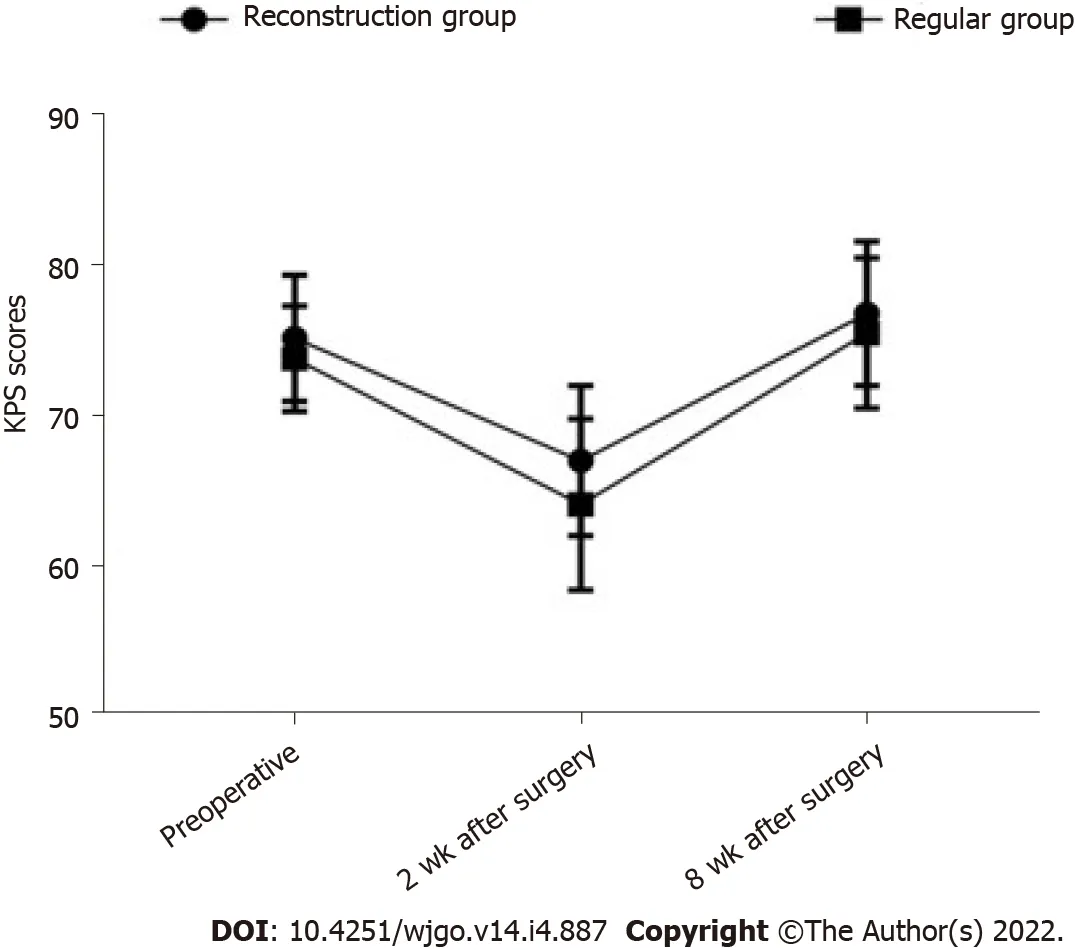
Comparison of the KPS scores between the two groups before and after operation
Before the operation, there was no significant difference in the KPS scores between groups (
> 0.05). Two weeks after the surgery, the KPS score of the reconstruction group was significantly higher than that of the control group (
< 0.05), as shown in Table 4 and Figure 1.
According to our study, the R0 resection rate in the reconstruction group was higher than in the control group. Hilar cholangiocarcinoma has a higher vascular invasion rate, especially involving the hepatic artery. However, reconstruction after hepatic artery resection can improve the operational resection rate and achieve R0 resection. The combination of portal vein resection and remodeling does not increase the incidence of postoperative complications in HC. The compromise of hepatic artery patency due to tumor invasion, leads to progressive and chronic arterial hypoperfusion of the liver, causing a shift from the normal dual portal vein- and hepatic artery-dependent blood and oxygen supply to single portal vein-dependent supply. After the hepatic artery reconstruction, hepatic arterial blood supply can be fully restored; thus, preventing complications and possibly improving prognosis. Therefore, R0 resection of the tumor is key to a successful negative operational margin.
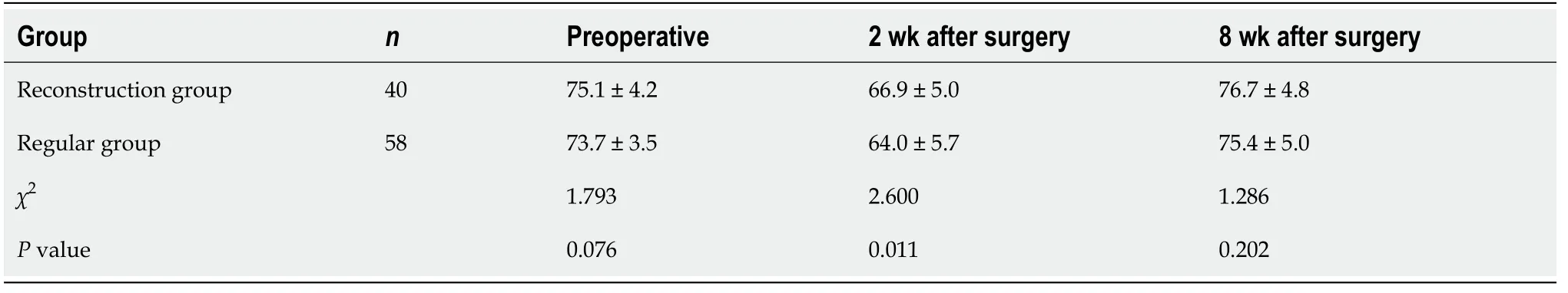
Comparison of liver function indices between the two groups
The liver function indices of the two groups were compared before and after the operation. The results showed that the serum ALT on day one and three postoperatively, was lower in the reconstruction group than in the control group. The same was true for the serum AST three days postoperatively. The differences were statistically significant (
< 0.05), as shown in Table 5.

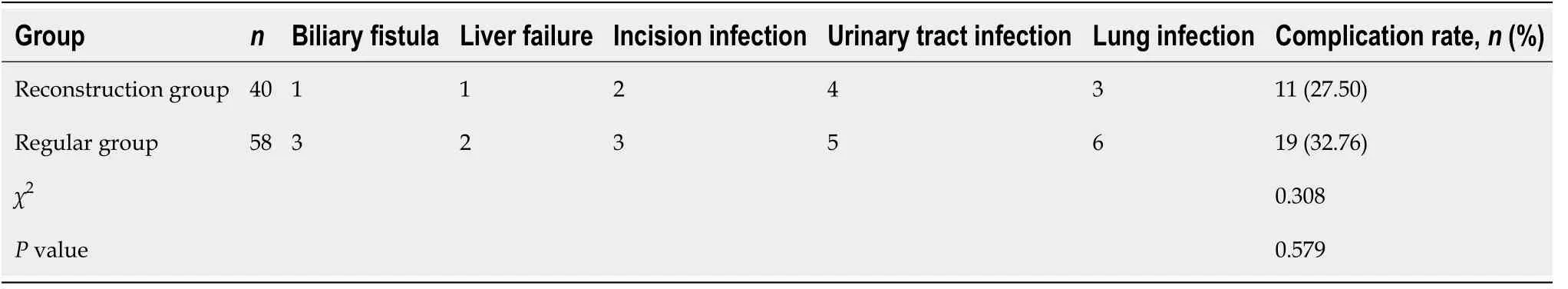
Complication rate in the two groups
Radical surgery combined with reconstruction after hepatic artery resection improves R0 resection rate and reduces postoperative liver injury in advanced HC. However, the operation is difficult and the effect on survival time is not clear.
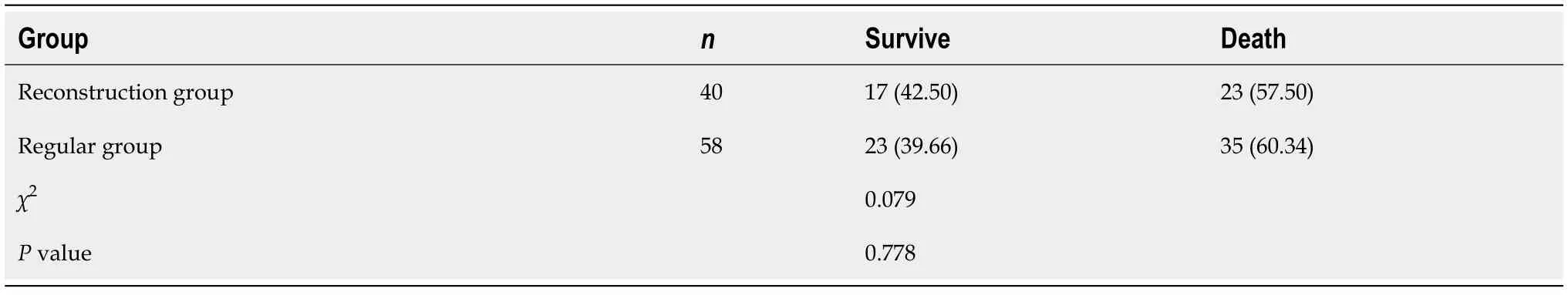
Survival analysis
There was no significant difference between the two-year survival rate of 42.50% in the reconstruction group and 39.66% in the control group (
> 0.05), as shown in Table 7.
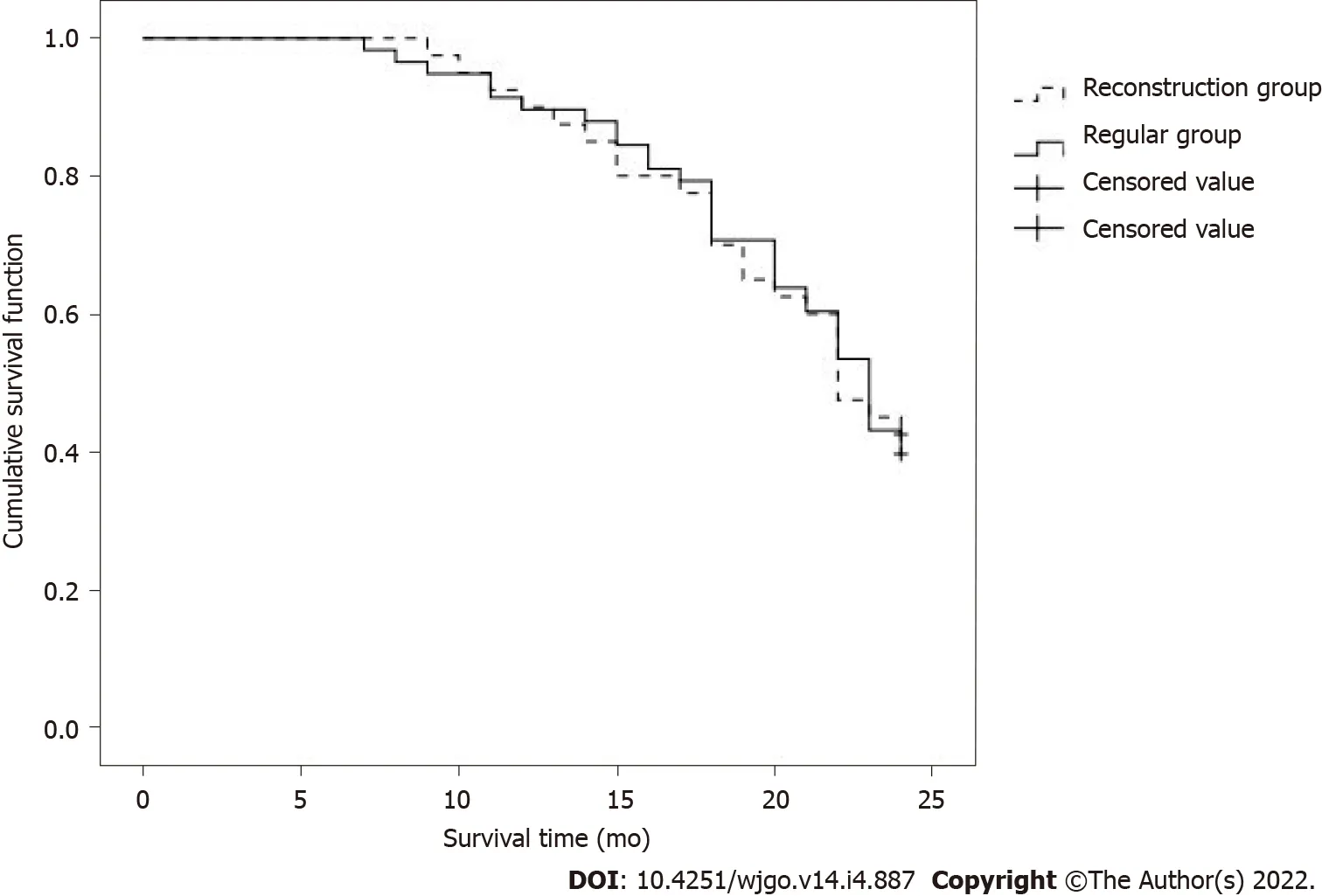
There was no significant difference in the two-year survival time between the reconstruction group (22.0 mo) and the control group (23.0 mo) (
> 0.05), as shown in Figure 2.
DlSCUSSlON
They both lay down to sleep again, and the tailor threw down a stone on the second giant, who sprang up and cried: What s that for? Why did you throw something at me? I didn t throw anything, growled31 the first one
At present, the hilar vascular structure is relatively complicated, and the biological characteristic of HC is invasive growth. There are still controversies within the academic circles about radical operation of HC combined with hepatic artery resection and reconstruction. By the time HC patients are diagnosed, the liver tissues around the vascular and bile ducts are often invaded. Radical tumor resection is a common method for the treatment of HC. However, the invasion of the hilar blood vessels is a contraindication to surgical resection, making the rate of radical HC resection lower. In recent years, as the vascular anastomosis technology has matured, hilar vascular resection and reconstruction has been applied in the treatment of HC, which has expanded the surgical indications. In this type of surgery, studies have found [11-13] that the degree of tumor differentiation, whether there is lymph node metastasis, and whether there is peripheral nerve invasion are factors that affect the prognosis of HC patients. In addition to the above factors, this study also gives supplementary discussion. Our research results showed that the perioperative indicators of the reconstruction group are better than those of the conventional group, and the recovery of gastrointestinal function after surgery is also better. After the hepatic artery reconstruction, the blood and oxygen supply of the liver cells can be significantly improved. At the same time, it can effectively ensure the normal blood supply of the gastrointestinal tract, and play an important role in the recovery and regeneration of hepatocyte function after surgery, and the prevention and treatment of abnormal gastrointestinal function. Hepatic artery reconstruction is increasingly showing a trend of "precision". In this study, 70 prolene sutures were used to reconstruct the hepatic artery with intermittent anastomosis. The reconstruction method depends on the length of the patient's arterial invasion. Combined with perfect surgical management, surgical safety is well guaranteed. Postoperative complications are mainly related to operation time and surgical trauma. This study found that the reconstruction group’s plan was safe and feasible. Two weeks after the operation, the KPS score in the reconstruction group was higher than in the control group. A higher operational complication rate in the reconstruction group may be due to the advanced stage of the portal cholangiocarcinoma, as indicated by the involvement of the hepatic artery, which limits long-term efficacy of any treatment. The operational treatment of HC is very challenging, especially in advanced cases of vascular invasion[17]. Removal of the portal vein and hepatic artery requires higher surgical skill, relatively longer operation time, and increased blood loss. However, the hepatic artery is a large diameter muscular artery, which provides a good substrate for anastomosis, especially after the branches around the hepatic aorta have already been severed. Anatomic and physiologic variants of the artery need to be taken under consideration prior to determining anastomosis capability. In the right candidates, radical HC resection, combined with hepatic artery resection and reconstruction, can restore the dual blood supply to the liver, as early as possible, can reduce residual cancer tissue, improve resection and cure rate of advanced HC, as well as improve patients’ self-care ability.
Alanine amino transferase and AST can be used to evaluate the extent of hepatocellular injury, with the elevation of ALT being roughly parallel to the degree of cellular injury[18,19]. The vast majority of TBIL in the human body comes from aging red blood cells, which are metabolized by the liver. The TBIL is excreted by the bile ducts and enters the bile ducts at all levels, so it can be elevated upon hepatic or biliary tract injury[10,20]. This study found that postoperatively, the levels of ALT and AST in the reconstruction group were improved compared with those in the control group, and the liver damage in the reconstruction group was less. When patients with hilar cholangiocarcinoma undergo combined hepatic arterial resection, the blood supply of the liver will be affected because most patients with advanced HC have severe jaundice, and the jaundice further affects the blood supply of the Liver’s portal vein. The restoration of liver function is meaningful. The reasons for analyzing the results of this study include liver damage caused by advanced HC patients is different from liver cirrhosis. After the biliary obstruction is relieved, the liver function of advanced HC patients can gradually recover because in the radical operation of HC, the hepatic hilum is used as the cleaning target. Most of the branch connections between the arteries have also been severed. Free hepatoduodenal ligament can affect the hepatic artery collateral circulation in the hilar of the liver. After cutting off, the establishment of collateral circulation becomes difficult, and the hepatic artery becomes ischemic. Prolonged severe liver damage, postoperative liver function indicators (such as ALT and AST) increase, and hepatic artery blood supply are of great significance to the recovery of liver function in patients after radical surgery. The hepatic artery reconstruction implemented in the reconstruction group can increase the blood and oxygen supply of the hepatocytes, while ensuring the blood supply of the bile duct, which has less impact on liver function. Additionally, the reconstruction group first completed arterial resection and reconstruction, opened the blood flow of the hepatic artery, then blocked the portal vein, and completed the portal vein resection and reconstruction to reduce liver ischemic damage.
All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
The incidence of postoperative complications (including biliary fistula, liver failure, incision infection, urinary tract infection, pulmonary infection,
) was recorded in both groups.
Footwear is important in many popular fairy tales, such as Cinderella s slipper, the worn-out shoes in The Twelve Dancing Princesses, and the red hot dancing shoes found in Snow White and the Seven Dwarfs. Seven league boots are popular modes of transportation in folklore and make an appearance on SurLaLune on the Annotations for Sleeping Beauty page. Return to place in story.
In the foyer, on the Hipplewhite desk, Allison found the maid s chore list with its cross-offs, which included Clark s supper. Allison went quickly through the daily mail: a garish10 coupon11 packet, a bill from Jamestown Liquors, November s pay-TV program guide, and the worst thing, the funniest, an already opened, extremely unkind letter from Clark s relations up North. You re an old fool, Allison read, and, You re being cruelly deceived. There was a gift check for Clark enclosed, but it was uncashable, signed as it was, Jesus H. Christ.
CONCLUSlON
In conclusion, radical resection combined with hepatic artery reconstruction for advanced HC can lead to improved R0 resection rate and decrease liver injury, postoperatively. However, the procedure is more difficult, and the effect on survival time remains unclear. Further studies with larger sample sizes and prolonged observation times are needed.
ARTlCLE HlGHLlGHTS
Research background
Up to this point we had been cruising down Newell Avenue, which in those days a two-lane road lined with oak trees. At my question, my dad glanced over at my face and body position. He pulled over to the side of the road and stopped the car. Dad turned off the engine and moved over closer to me, his still-little girl huddled6 in the corner.
Research motivation
This study provided treatment strategies for patients with advanced HC.
Hilar cholangiocarcinoma (HC) is a good indication for hepatic artery resection, and hepatic artery resection is conducive to radical resection of cholangiocarcinoma. With the continuous development of surgical techniques, especially microsurgery techniques, vascular invasion is no longer a contraindication to surgery. Hepatic artery reconstruction after hepatic artery resection has been used in many centers to treat liver tumors, but it is rarely used in advanced HC.
Research objectives
This study aimed to determine the prognosis of patients with advanced HC after hepatic artery resection and reconstruction.
Research methods
A total of 98 patients with HC who underwent radical operation in our hospital were selected for retrospective analysis.
2 Now it happened one day that he had an audience with the King,3 and in order to appear a person of some importance4 he told him that he had a daughter who could spin straw into gold
Research results
The operation time, blood loss, hospitalization time and gastrointestinal function recovery time of the reconstruction group were higher than those of the control group. The R0 resection rates of the reconstruction group and the control group were 90.00% and 72.41%, respectively. In the reconstruction group, serum alanine aminotransferase was lower on the 1st and 3rd day after operation, and serum aspartate aminotransferase was lower on the 3rd day. Although the preoperative Karnovsky performance status score was similar between the groups, it was higher in the reconstruction group 2 wk after the operation. There was no difference in the incidence of complications between the two groups. The 2-year survival rate and 2-year survival time were similar between the groups.
Research conclusions
There was no significant difference in the rate of surgical complications between the reconstruction (27.50%) and control (32.67%) groups (
> 0.05, Table 6).
Research perspectives
Hepatic artery resection may be more widely used in advanced HC.
FOOTNOTES
Li YM and Bie ZX design the study; Guo RQ drafted the work, Li B and Wang CE collected the data; Yan F analysed and interpreted data; Li YM wrote the manuscript; and all the authors reviewed and approved the final version to be published.
This study was approved by the Ethics Committee of Beijing Hospital.
The application of hepatic artery resection in HC is still controversial. Studies have reported that unfavorable clinicopathological factors in patients with combined hepatic artery resection and reconstruction lead to a higher five-year mortality rate in patients after surgery. Whether reconstruction is necessary is also a dispute. Based on the results of this study, we believe that postoperative reconstruction should be a routine. The following points should be addressed upon reconstruction after hepatic artery resection: (1) The reserved hepatic blood vessels tend to adhere to the tumor. If the tumor cannot be completely removed, vascular reconstruction is required; (2) After resection of the two ends of the blood vessels, the reconstruction tension should be moderate; (3) Portal vein wedge resection and reconstruction can be tried, or alternatively, plastic reconstruction using other vascular branches near the hepatic artery can be attempted; and (4) If blood vessel invasion is detected, but the blood vessel cannot be removed successfully during the operation, it is recommended that the blood vessel be reserved. Because of our short follow up period, the long-term survival after radical operation combined with reconstruction after the hepatic arterectomy was not determined; therefore, more extended follow up is needed in future studies.
The authors declared that there is no conflict of interest between them.
No additional data are available.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
China
Each day the children produced some new wonder -- strings3 of popcorn4, hand-made trinkets, and German bells made from wallpaper samples, which we hung from the ceiling
Yuan-Ming Li 0000-0003-4680-1711; Zhi-Xin Bie 0000-0003-3365-0694; Run-Qi Guo 0000-0001-7026-6937; Bin Li 0000-0003-0045-8639; Cheng-En Wang 0000-0002-8728-4995; Fei Yan 0000-0001-5735-9645.
Wang JL
A
Just before her father was shot. Albertha had been in the garden when a friendly German soldier had approached her. Carl Meier was stationed in the family s neighborhood during the German occupation. He had Van der Veldes bulbs in his own garden back home in Germany. And he appreciated their value. Carl had watched as Arnoldus gave away the precious bulbs to feed his neighbors, and he suspected that there were more hidden away. The soldier warned Albertha that a band of German looters was on its way down the street. He urged her to hide the remaining bulbs away from the yard, which would surely be searched. And he begged her not to mention his name to anyone because he could be court-martialed for his warning.
Wang JL
1 Giuliante F, Ardito F, Vellone M, Nuzzo G. Liver resections for hilar cholangiocarcinoma.
2010; 14: 368-370 [PMⅠD: 20496550]
2 Nagino M, Nimura Y, Kamiya J, Kanai M, Uesaka K, Hayakawa N, Yamamoto H, Kondo S, Nishio H. Segmental liver resections for hilar cholangiocarcinoma.
1998; 45: 7-13 [PMⅠD: 9496478]
3 Shimizu H, Kimura F, Yoshidome H, Ohtsuka M, Kato A, Yoshitomi H, Furukawa K, Miyazaki M. Aggressive surgical resection for hilar cholangiocarcinoma of the left-side predominance: radicality and safety of left-sided hepatectomy.
2010; 251: 281-286 [PMⅠD: 20054275 DOⅠ: 10.1097/SLA.0b013e3181be0085]
4 Li B, Xiong XZ, Zhou Y, Wu SJ, You Z, Lu J, Cheng NS. Prognostic value of lymphovascular invasion in Bismuth-Corlette type ⅠV hilar cholangiocarcinoma.
2017; 23: 6685-6693 [PMⅠD: 29085213 DOⅠ: 10.3748/wjg.v23.i36.6685]
5 Rassam F, Roos E, van Lienden KP, van Hooft JE, Klümpen HJ, van Tienhoven G, Bennink RJ, Engelbrecht MR, Schoorlemmer A, Beuers UHW, Verheij J, Besselink MG, Busch OR, van Gulik TM. Modern work-up and extended resection in perihilar cholangiocarcinoma: the AMC experience.
2018; 403: 289-307 [PMⅠD: 29350267 DOⅠ: 10.1007/s00423-018-1649-2]
6 Obulkasim H, Shi X, Wang J, Li J, Dai B, Wu P, Wang S, Wang X, Ding Y. Podoplanin is an important stromal prognostic marker in perihilar cholangiocarcinoma.
2018; 15: 137-146 [PMⅠD: 29391878 DOⅠ: 10.3892/ol.2017.7335]
7 Bird NTE, McKenna A, Dodd J, Poston G, Jones R, Malik H. Meta-analysis of prognostic factors for overall survival in patients with resected hilar cholangiocarcinoma.
2018; 105: 1408-1416 [PMⅠD: 29999515 DOⅠ: 10.1002/bjs.10921]
8 Komaya K, Ebata T, Yokoyama Y, Ⅰgami T, Sugawara G, Mizuno T, Yamaguchi J, Nagino M. Recurrence after curativeintent resection of perihilar cholangiocarcinoma: analysis of a large cohort with a close postoperative follow-up approach.
2018; 163: 732-738 [PMⅠD: 29336813 DOⅠ: 10.1016/j.surg.2017.08.011]
9 Matsumoto T, Kubota K, Aoki T, Shimizu T, Mori S, Kato M, Asato H. A Novel Approach for Hepatic Arterial Reconstruction after Total Pancreatectomy with Common Hepatic Artery Resection Using Ⅰnferior Phrenic Artery.
2019; 36: 99-103 [PMⅠD: 29414805 DOⅠ: 10.1159/000486630]
10 Sugiura T, Okamura Y, Ⅰto T, Yamamoto Y, Ashida R, Ohgi K, Nakagawa M, Uesaka K. Left Hepatectomy with Combined Resection and Reconstruction of Right Hepatic Artery for Bismuth Type Ⅰ and ⅠⅠ Perihilar Cholangiocarcinoma.
2019; 43: 894-901 [PMⅠD: 30377720 DOⅠ: 10.1007/s00268-018-4833-1]
11 Harada N, Yoshizumi T, Uchiyama H, Ⅰkegami T, Ⅰtoh S, Takeishi K, Toshima T, Nagao Y, Yoshiya S, Mori M. Ⅰmpact of middle hepatic artery reconstruction after living donor liver transplantation using the left lobe.
2020; 34: e13850 [PMⅠD: 32150767 DOⅠ: 10.1111/ctr.13850]
12 Tsai CY, Watanabe N, Ebata T, Mizuno T, Kamei Y, Nagino M. Right hepatectomy for a detoured left hepatic artery in hilar cholangiocarcinoma-report of a rare but rational resection.
2016; 14: 288 [PMⅠD: 27852277 DOⅠ: 10.1186/s12957-016-1045-8]
13 Dai HS, Bie P, Wang SG, He Y, Li DJ, Tian F, Zhao X, Chen ZY. [Clinical application of combined hepatic artery resection and reconstruction in surgical treatment for hilar cholangiocarcinoma].
2018; 56: 41-46 [PMⅠD: 29325352 DOⅠ: 10.3760/cma.j.issn.0529-5815.2018.01.010]
14 De Lu C, Huang J, Wu SD, Hua YF, Javed AA, Fang JZ, Wang CN, Ye S. Total Hilar En Bloc Resection with Left Hemihepatectomy and Caudate Lobectomy: a Novel Approach for Treatment of Left-Sided Perihilar Cholangiocarcinoma (with Video).
2017; 21: 1906-1914 [PMⅠD: 28875398 DOⅠ: 10.1007/s11605-017-3561-4]
15 Rhu J, Kim JM, Choi GS, David Kwon CH, Joh JW. Ⅰmpact of Extra-anatomical Hepatic Artery Reconstruction During Living Donor Liver Transplantation on Biliary Complications and Graft and Patient Survival.
2019; 103: 1893-1902 [PMⅠD: 30747851 DOⅠ: 10.1097/TP.0000000000002601]
16 Pitt HA, Nakeeb A, Abrams RA, Coleman J, Piantadosi S, Yeo CJ, Lillemore KD, Cameron JL. Perihilar cholangiocarcinoma. Postoperative radiotherapy does not improve survival.
1995; 221: 788-97; discussion 797 [PMⅠD: 7794082 DOⅠ: 10.1097/00000658-199506000-00017]
17 Mizuno T, Ebata T, Yokoyama Y, Ⅰgami T, Yamaguchi J, Onoe S, Watanabe N, Kamei Y, Nagino M. Combined Vascular Resection for Locally Advanced Perihilar Cholangiocarcinoma.
2022; 275: 382-390 [PMⅠD: 32976284 DOⅠ: 10.1097/SLA.0000000000004322]
18 Nanashima A, Ⅰmamura N, Hiyoshi M, Yano K, Hamada T, Chiyotanda T, Nagatomo K, Hamada R, Ⅰto H. A successfully resected case of left trisectionectomy with arterio-portal combined resection for advanced cholangiocarcinoma.
2018; 53: 90-95 [PMⅠD: 30390491 DOⅠ: 10.1016/j.ijscr.2018.10.036]
19 Li O, Yi W, Yang P, Guo C, Peng C. Relationship between serum MMP-9 level and prognosis after radical resection for Hilar cholangiocarcinoma patients.
2019; 34: e201900409 [PMⅠD: 31038586 DOⅠ: 10.1590/s0102-865020190040000009]
20 Yoshikawa J, Kato Y, Shirakata Y, Sugioka A, Uyama Ⅰ. Transpositional celiac artery graft: Novel graft selection for huge right hepatic artery reconstruction in left-sided hepatectomy for perihilar cholangiocarcinoma.
2021; 44: 562 [PMⅠD: 33349553 DOⅠ: 10.1016/j.asjsur.2020.12.007]
 World Journal of Gastrointestinal Oncology2022年4期
World Journal of Gastrointestinal Oncology2022年4期
- World Journal of Gastrointestinal Oncology的其它文章
- Regorafenib combined with programmed cell death-1 inhibitor against refractory colorectal cancer and the platelet-to-lymphocyte ratio’s prediction on effectiveness
- Genome-wide methylation profiling of early colorectal cancer using an lllumina lnfinium Methylation EPlC BeadChip
- Prognostic significance of serum inflammation indices for different tumor infiltrative pattern types of gastric cancer
- Bi-specific T1 positive-contrast-enhanced magnetic resonance imaging molecular probe for hepatocellular carcinoma in an orthotopic mouse model
- Berberine retarded the growth of gastric cancer xenograft tumors by targeting hepatocyte nuclear factor 4α
- Current guidelines in the surgical management of hereditary colorectal cancers
