Prevention of late complications of endoscopic resection of colorectal lesions with a coverage agent:Current status of gastrointestinal endoscopy
TO THE EDITOR
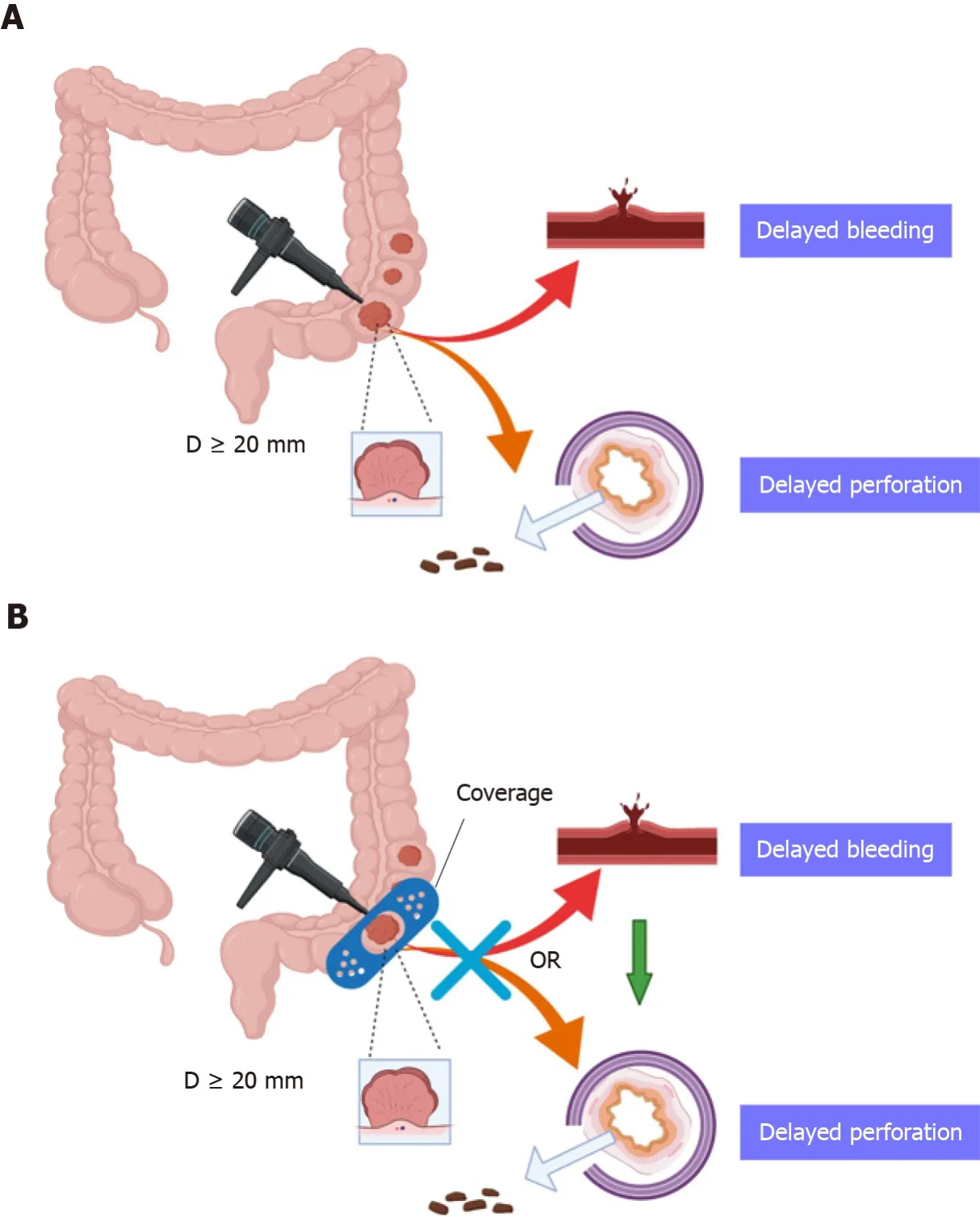
We read the paper by Lorenzo-Zú?iga[1] with great interest. The authors reviewed the currently available literature on preventing delayed perforation (DP) and delayed bleeding (DB) with overlays after endoscopic mucosal excision or endoscopic submucosal resection.
The visits to the church were festive occasions, but among thefisherman s house one was especially looked forward to; this was, infact, the visit of the brother of Jurgen s foster-mother, theeel-breeder from Fjaltring, near Bovbjerg. He came twice a year in acart, painted red with blue and white tulips upon it, and full ofeels; it was covered and locked like a box, two dun oxen drew it,and Jurgen was allowed to guide them.
This systematic collection and review of the present literature on prevention of DP and DB with coverage bandages after endoscopic submucosal dissection or endoscopic mucosal resection (EMR) of large nonpedunculated colorectal lesions (LNPCLs)indicated several interesting outcomes; however, there are some deficiencies. First, the database for literature selection should not be limited to PubMed. Other common medical databases should also be selected, such as Medline, Ovid, Embase, and Web of Science. The data obtained in this way will be more comprehensive, and the results will be more meaningful.
The European Society of Gastrointestinal Endoscopy (ESGE) recommends hot snare polypectomy for pedunculated polyps. To stem bleeding from pedunculated colorectal polyps with stalk diameters ≥ 10 mm or heads ≥ 20 mm, the ESGE recommends pretreatment of the stalk with injectable diluted epinephrine and/or mechanical hemostasis (moderate quality evidence, highly recommended)[2].
We agree with Lorenzo-Zú?iga[1], who reported that the conventional utilization of prophylactic clipping has not diminished the overall risk of postprocedural bleeding, and focus on the economic efficiency ratio is needed. A cohort study of 8366 colonoscopies involving polypectomy conducted by Forbes[3] yielded 95 delayed postpolypectomy bleeding (DPPB) incidents. Preventive clipping was not related to reduced DPPB (adjusted odds ratio 1.27; 0.83-1.96). Other efficacy and costeffectiveness studies are needed for patients with proximal lesions ≥ 20 mm, in whom prophylactic clipping might be useful. Another multicenter cohort study was conducted on patients with nontruncated lesions ≥ 20 mm resected by EMR and found that DB occurred in 45 of 1034 EMRs (4.5%)[4]. Tsutsumi[5] performed a systematic review and meta-analysis to identify whether endoscopic prophylaxis procedures reduced delayed adverse events. They found that the preventive process significantly decreased the risk of delayed adverse events (DB and DP) by more than 80%. We drew a schematic diagram to give an overview of this paper. Endoscopic removal of LNPCLs might lead to significant adverse events, such as DP and DB,despite the closure of mucosal lesions with clips (Figure 1A). Coverage of the defects after endoscopic excision supplies shielding protection to prevent delayed complications (Figure 1B). The above results confirm that the work done by Lorenzo-Zú?iga[1] is worthy of recognition and that our findings can serve as a complement to their research. In the future, we should re-evaluate the efficacy of prophylactic clipping of LNPCLs and further explore the role of coverage agents in preventing delayed adverse events.
I will ride on it, said the prince; but with that the witch dragged it away again, and came back with an old, wrinkled, toothless hag, whose hands trembled with age
Yan-Dong Miao especially thanked Wu-Xia Quan for her care, patience, and support over the years.
 World Journal of Gastrointestinal Oncology2022年2期
World Journal of Gastrointestinal Oncology2022年2期
- World Journal of Gastrointestinal Oncology的其它文章
- Endoscopic ultrasound-guided ablation of solid pancreatic lesions:A systematic review of early outcomes with pooled analysis
- Predictive value of serum alpha-fetoprotein for tumor regression after preoperative chemotherapy for rectal cancer
- Chemotherapy predictors and a time-dependent chemotherapy effect in metastatic esophageal cancer
- Association and prognostic significance of alpha-L-fucosidase-1 and matrix metalloproteinase 9 expression in esophageal squamous cell carcinoma
- Comprehensive molecular characterization and identification of prognostic signature in stomach adenocarcinoma on the basis of energy-metabolism-related genes
- Multimodal treatment in oligometastatic gastric cancer
