A survey of anaesthetic preferences in cataract surgery
INTRODUCTION
Cataract surgery is one of the most common operations in the world.Significant advances in cataract surgery have occurred over the past few decades,with differing preferences and practices existing in different parts of the world.In terms of ophthalmic anesthesia,which is an essential component of the cataract surgery process,it originally began as cocaine drops topically applied to the ocular surface in 1884.Soon ophthalmologists had described the techniques of retrobulbarand sub-Tenon'sanesthesia.Over the course of the past century modifications of these techniques have been developedand in 1986 the first description of the peribulbar block was published.The ophthalmologist now has a range of anaesthesia techniques at their disposal.These include general anesthesia,topical anesthesia,local infiltration anesthesia or regional anesthesia in the form of facial nerve blocks.With such an array of options,applicable even in routine cases,it can be difficult to decide which technique to useand a knowledge of the practice of other colleagues can be useful in making an informed choice.
There have been several surveys conducted worldwide into cataract surgery trends that have incorporated the anesthesia used in surgery,with the most recent being by Tam,who in 2016 surveyed a cohort of Singaporean ophthalmologists.All known surveys in this area have been conducted in a country specific manner and thereby not allowed direct comparison of practices between regions.Given the absence of up-to-date data in this area,particularly from ophthalmologists practicing in the United States (US) and United Kingdom(UK),where the most recent anesthesia preference in cataract surgery surveys occurred in 2004and 2006respectively,we felt it was important to obtain updated data to identify any new changes or trends in practice,and subsequently make this information available to ophthalmologists worldwide.
SUBJECTS AND METHODS
The present study involved no major ethical issues.All participants were greeted with a consent form,which outlined the purpose of the study and asked the participants to confirm they were practicing ophthalmologists by providing an institutional email address to verify this.The respondents were given the assurance of complete confidentiality and assured that any personal details will not be shared with anyone outside of the research team.Overall,this study agreed with all the ethical guidelines set by Western Sussex Hospitals Trust and conducted in accordance with the principles of the Declaration of Helsinki.
Our survey provides a brief insight into current trends in anesthetic choice during cataract surgery.This survey is the first to include surgeons from multiple countries in one analysis and also ask regarding local anesthetic drug choice.Our survey was heavily dominated by respondents from the USA (43.6%) and the UK (32.4%) which significantly influenced our results;unsurprising given that the forums in which this survey was distributed were English-medium forums and predominantly used by western ophthalmologists.Compared to the most recent literature available,our results show a general concordance.In the US,Leamingsurveyed a cohort of US ophthalmologists and found that the most popular technique of anesthesia was topical anesthesia combined with intra-cameral injection,with 43.6% of participants preferring this technique.Topical anesthesia alone and peribulbar anesthesia ranked joint second with 17% of surgeons favoring this approach.Our survey showed similar findings with topical anesthesia with intracameral injection (47.8%) and topical anesthesia alone (40.8%) being the two most favored techniques.Peribulbar anesthesia however was not found to be very popular with only 1 participant preferring this.In terms of practice in the UK there was a noted difference between our results and the most recent survey of UK ophthalmologists,which had been carried out in 2001 and had showed that sub-Tenon's block was most popular anesthetic technique,with 46.9% of surgeons choosing it,followed thereafter by topical anesthesia alone (22.3% of surgeons).Our results found,in general,a low favorability of sub-Tenon's anesthesia with only 8.5% of surgeons preferring it.Moreover when the UK only participants (=23) were analyzed,56.5% preferred topical anesthesia alone,30.4% preferred topical anesthesia with intra-cameral injection and 13.0% preferred sub-Tenon's anesthesia.From this data it is possible that there is a move away from sub-Tenon's anesthesia in the UK with topical anesthesia beginning to predominate,however a study with a larger sample size of UK ophthalmologists is required to confirm this.There is also,interestingly,an indication from our data that topical anesthesia alone is more popular amongst UK surgeons,whereas topical anesthesia with intracameral injection is more popular amongst US surgeons.
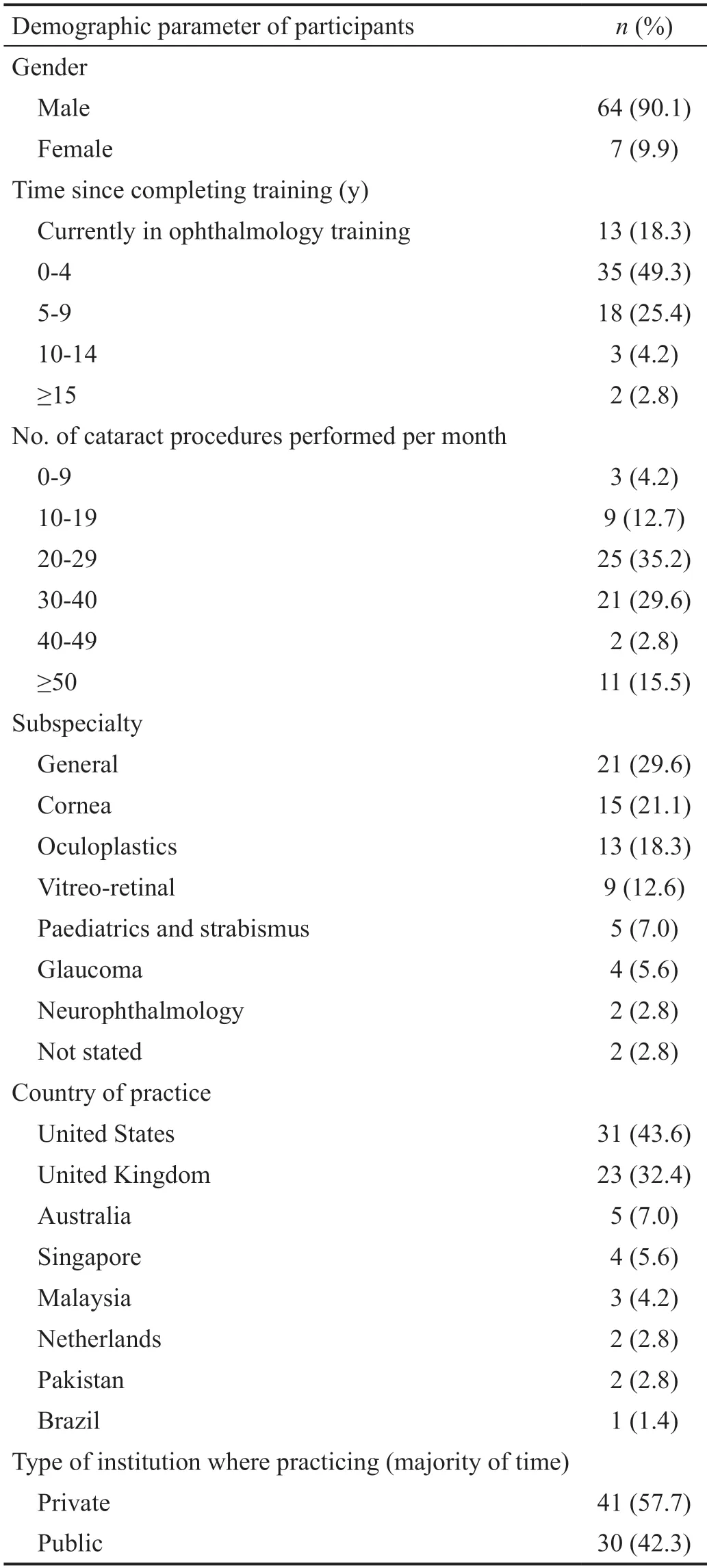
In total there were 93 eligible participants who were sent the survey.A total of 71 completed surveys were returned(response rate=76.3%),with 64 (90.1%) of respondents being male and 7 (9.9%) being female.The majority of the ophthalmologists surveyed were relatively recently qualified,being on average 4.5y post completion of ophthalmology training.Participants were well distributed between private(=30,42.3%) and public sector institutions (=41,57.7%)and the average number of cataracts performed per month by the participants was 31 (range 5-65).There was a significant number of general ophthalmologists (=21,29.6%)who responded to our survey,however the majority were subspecialists with cornea (=15,21.1%) and oculoplastics(=13,18.3% specialists being the most common.The 43.6% of survey participants practiced in the US,32.4%of participants practiced in the UK and 24% practiced in other countries.Table 1 shows the various demographic data collected from our survey participants.
RESULTS
A web-based survey was created in Google Forms (Alphabet Inc.,Mountain View,CA,USA) taking into account data obtained in previous similar studies.This was distributed electronically to 93 selected members of the following online websites which contained ophthalmology forums:eyedocs.co.uk,corneasociety.org,eyeconnectinternational.com,facebook.com,and reddit.com.Participants were selected based on post history in the forums which suggested that they practiced cataract surgery.The 93 selected participants were direct messaged with a link to the survey in early August 2020 and received monthly reminders to complete the survey if they had not yet completed it.Results were exported from Google Forms into Microsoft Excel (v.2016,Microsoft Corp.,Redmond,WA,USA) in late January 2021 and subsequently analyzed.There was no financial renumeration for completing the survey.
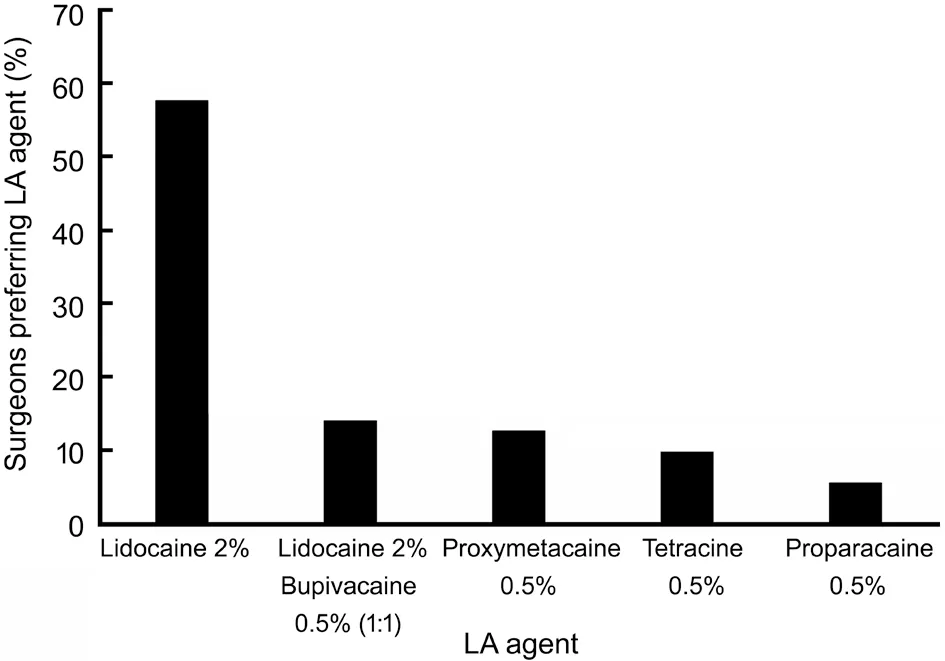
With regards to local anaesthetic use,the clear favourite was lidocaine 2%,used by 41 (57.7%) surgeons.The second most popular local anaesthetic was a lidocaine 2%:bupivacaine 0.5% (1:1) combination,used by 10 (14.1%) surgeons.The least popular anaesthetic was proparacaine 0.5%,preferred by only 4 (5.6%) surgeons (Figure 1).There were 41 surgeons who added adjuncts to their local anaesthetic,with epinephrine being used by 39 surgeons and therefore being the most popular adjunct.Two surgeons whose preferred technique was sub-Tenon's block added hyaluronidase to lidocaine 2%.The 36 (50.7%) surgeons also applied topical anaesthesia to the non-operative eye,as a means of reducing the blink reflex.
Our results show most congruence with a 2016 survey by Ong-Toneof Canadian ophthalmologists who found that 66% preferred topical anesthesia with intracameral injection,and 29% preferred topical anesthesia alone;other methods were preferred by <1% of participants.Analyzing studies from the aforementioned countries as well as New Zealand,Singaporeand Koreait is clear that topical anesthesia alone and in combination with intracameral injection seems to be the technique of choice.There also appears to be a disinterest in sharp needle blocks,in particular retro-bulbar and peribulbar blocks,likely related to the discomfort experienced by patients and the higher complication rate.Interestingly a 2016 survey of Singaporean ophthalmologistsalso enquired regarding rationale behind anesthetic choice and similar to our findings,patient comfort was the most common reason stated.This reinforces the issue of patient discomfort with sharp needle techniques.
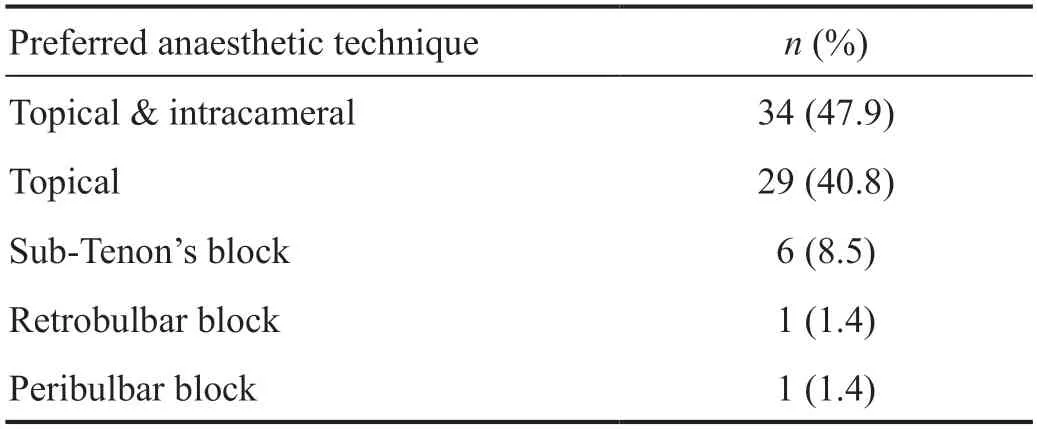
The anaesthetic of choice amongst our participants was topical anaesthesia with intracameral injection with 34 (47.9%)surgeons favouring this,followed by topical anaesthesia,which 29 (40.8%) surgeons favoured.The least popular techniques were retrobulbar and peribulbar block with only 1 surgeon preferring each of these (Table 2).
DISCUSSION
This means that when you let a neural network develop its own behavioral model, you are basically losing visibility into its reasoning process. And mostly, the inner parameters and connections that neural networks develop are so numerous and complex that they become too difficult for humans to understand.
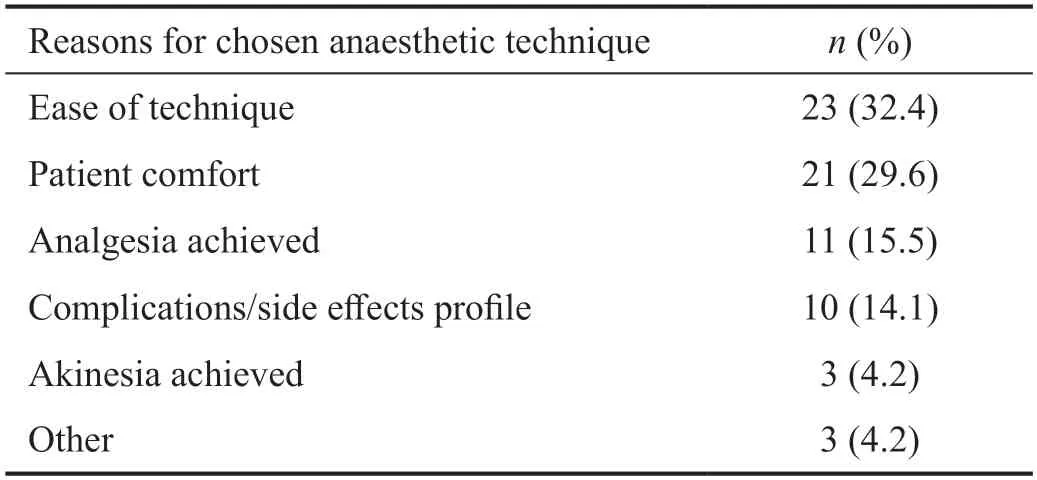
In terms of reasons for their preferred anaesthetic technique,the two most common reasons stated by our participants were ease of technique (=23,32.4%) and patient comfort(=21,29.6%).The least common reason was akinesia achieved,stated by 3 (4.2%) surgeons as a reason for their preferred anaesthetic technique.There were also 3 surgeonswho mentioned in the comments section of the survey that postoperative recovery from anaesthetic and a language barrier limiting patient communication during the surgery as a reason for anaesthetic choice (Table 3).
The smartest scientists in the world gathered to figure it out. Was something wrong with people s eyes or was it a trick of nature? They did studies and tests and analyzed6 and evaluated7 and debated and wrote article after article, but couldn t explain it.
This survey has produced several valuable insights however a note should also be made of its limitations.First,our sample size was relatively small,consisting of 71 respondents which makes it difficult to generalize the results.Furthermore given our place of distribution being English-medium online forums,our cohort was skewed towards younger ophthalmologists and those practicing in western countries.There was also a heavy bias towards male ophthalmologists who constituted 90.1% of our respondents.Lastly,a significant number of surgeons who were sent the survey did not respond (survey responses rate=76.3%),which could also have caused bias.A more rigorous survey into surgeons' anesthetic preferences during cataracts cases,which we hope will occur in the future especially given the lack of recent data that exists for the US and the UK,should take these limitations into account.
In conclusion,topical anaesthesia,especially combined with intracameral injection is the technique of choice for cataract cases based on our survey of predominantly US and UK based ophthalmologists.The reasons for this are its ease in terms of technique for the surgeon,as well as the patient comfort it provides.Lidocaine 2% is the most favoured local anaesthetic agent.There appears to be a shift away from sharp-needle techniques for anaesthesia in cataract surgery and this survey supports this trend,particularly in the UK.
ACKNOWLEDGEMENTS
None;None;None.
 International Journal of Ophthalmology2022年2期
International Journal of Ophthalmology2022年2期
- International Journal of Ophthalmology的其它文章
- IJO/IES Event Photos
- Inhibitory effect on subretinaI fibrosis by anti-pIacentaI growth factor treatment in a Iaser-induced choroidaI neovascuIarization modeI in mice
- Artesunate inhibits proIiferation and migration of RPE ceIIs and TGF-β2 mediated epitheIiaI mesenchymaI transition by suppressing PI3K/AKT pathway
- NoveI mutations in the BEST1 gene cause distinct retinopathies in two Chinese famiIies
- Frequency cumuIative effect of subthreshoId energy Iaser-activated remote phosphors irradiation on visuaI function in guinea pigs
- One-step thermokeratopIasty for pain aIIeviating and pretreatment of severe acute corneaI hydrops in keratoconus
