Efficacy and effect on related brain-gut peptides of acupoint sticking therapy for functional dyspepsia
Kong Wei-guang (孔偉光), He Tian-feng (何天峰)
1 Department of Spleen and Stomach Diseases, Inner Mongolia Hospital of Traditional Chinese Medicine, Huhhot 010020, China
2 Department of Acupuncture, Jiading Hospital of Traditional Chinese Medicine, Shanghai, Shanghai 201899, China
Abstract
Keywords: Acupoint Sticking Therapy; Emplastrum Therapy; Dyspepsia; Liver-qi Stagnation and Spleen Deficiency;Brain-gut Peptide; 5-hydroxytryptamine; Ghrelin
Functional dyspepsia (FD) is a functional gastrointestinal disease, which refers to a group of upper abdominal discomfort symptoms such as loss of appetite, epigastric distention, epigastric pain, early satiety, belching, nausea, and desire to vomit, but without organic lesions. The overall global prevalence of FD is 11.5%-14.5%, and the prevalence of FD in Asia is 8.0%-23.0%, with China having a higher prevalence of FD than developed Asian countries, but a lower prevalence than other developing Asian countries[1-2].Previous findings from our research group showed that acupoint sticking with Jianpi Tongjing Zhitong ointment could improve various gastrointestinal discomforts,reduce their anxiety symptoms, and smooth out gastrointestinal motility in FD patients, but its mechanism remains unclear[3].
It has been found that gastrointestinal hormones such as 5-hydroxytryptamine (5-HT) and ghrelin play an important role in the pathogenesis and treatment of FD[4-5]. In this study, we observed the efficacy of acupoint sticking with Jianpi Tongjing Zhitong ointment in the treatment of FD due to liver-qi stagnation and spleen deficiency as well as its effects on serum 5-HT and ghrelin contents, and explored the possible mechanism. The results of the study are reported as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria in Western medicine
Roman Ⅲ Functional Gastrointestinal Disease Diagnostic Criteria were referred[6]: at least one of postprandial fullness, early satiety, epigastric pain or burning, and no evidence of organic disease (including upper gastrointestinal endoscopy) could explain the symptoms; with symptoms for at least 6 months prior to diagnosis, and the symptoms in the last 3 months met the above criteria.
1.1.2 Diagnostic criteria in traditional Chinese medicine (TCM)
Referring the criteria for identifying ‘fullness’ due to liver-qi stagnation and spleen-deficiency in theGuiding Principles for Clinical Study of New Chinese Medicines[7].Primary symptoms: gastric distention and fullness, loss of appetite, fatigue and weakness, often aggravated by emotional discomfort. Secondary symptoms: pain in bilateral hypochondrium, loose stools. Tongue and pulse: a pale tongue with white coating, deep wiry or weak pulse.
1.2 Inclusion criteria
Those who met the above diagnostic criteria; had not taken any gastrointestinal prokinetic drugs for at least 4 weeks prior to treatment; were not participating in other clinical trials; signed informed consent.
1.3 Exclusion criteria
Those who were aged <18 years or >65 years;diagnosed with organic diseases such as esophagitis,atrophic gastritis, gastric or duodenal ulcer, or gastroenteric tumor or irritable bowel syndrome;combined with serious primary or wasting diseases of the cardiac, cerebral, pulmonary, or renal systems; were susceptible to infection or bleeding; women were pregnant or with intent to get pregnant or lactating;with allergic constitution or were allergic to the drugs or medical tape used in this study.
1.4 Statistical analysis
The data were analyzed by SPSS 21.0 software. The measurement data conforming to normal distribution were expressed as mean ± standard deviation (±s).Intra-group comparison was assessed by pairedt-test and between-group comparison was tested using independent samplet-test. For measurement data that did not conform to normal distribution, the results were expressed as median (minimum, maximum) [M (min,max)], and tested by non-parametric test. Chi-square test and non-parametric test were used for counting data and categorical data. Pearson was adopted for correlation analysis.P<0.05 was taken as statistically significant.
1.5 General data
A total of 100 patients were enrolled from outpatients in the Department of Spleen and Stomach,Inner Mongolia Hospital of Traditional Chinese Medicine between July 2018 and December 2019. The patients were divided into a control group and a treatment group by the random number table method,with 50 cases in each group. One dropout occurred in the control group and 3 dropouts occurred in the treatment group during the study period. There were no statistically significant differences between the two groups in baseline gender, age or disease duration (allP>0.05), confirming that the two groups were appropriately comparable (Table 1).
This trial was approved by the Medical Ethics Committee of Inner Mongolia Hospital of Traditional Chinese Medicine (Approval No. nmgzy-2017-08).

Table 1. Baseline characteristics between the two groups
2 Treatment Methods
2.1 Treatment group
The treatment group received acupoint sticking with Jianpi Tongjing Zhitong ointment.
Ointment formulation:Zhi Chuan Wu(Radix Aconiti Praeparata) 6 g,Ding Xiang(Flos Caryophylli) 10 g,Cao Dou Kou(Semen Alpiniae Katsumadai) 10 g,Bai Jie Zi(Semen Sinapis Albae) 6 g,Bai Zhu(Rhizoma AtractylodisMacrocephalae) 10 g,Wu Zhu Yu(Fructus Evodiae) 10 g,Gao Liang Jiang(Rhizoma Alpiniae Officinarum) 6 g,Gan Cao(Radix Glycyrrhizae Preparata) 5 g andCi Shi(Magnetitum) 30 g.
The above herbs were powdered and made into an ointment at the ratio of 1:1 with oil as the base, evenly placed on a 3 cm × 3 cm adhesive patch (each patch contained 3 g of raw herbs) and applied to Shenque(CV 8), Shangwan (CV 13), Zhongwan (CV 12), Xiawan(CV 10), Guanyuan (CV 4), bilateral Tianshu (ST 25) and Zusanli (ST 36). Each application was applied for 4-6 h and removed afterward, once a day. The patient was instructed to observe the skin during this period and discontinued immediately in case of blistering or allergy.
2.2 Control group
The control group was treated with mosapride citrate(State Food and Drug Administration Approval No.H20031110, 5 mg/tablet, Chengdu Kanghong Pharmaceutical Co., Ltd., China), 5 mg/time, 3 times per day orally taken 15-30 min before meals.
2.3 Duration of treatment and precautions
The efficacy was assessed after 4 weeks of treatment.All other drugs related to the treatment of the disease were withdrawn during the treatment period in both groups. Patients were instructed to avoid spicy, cold and other stimulating foods; avoid excessive mental stress and maintain a relaxed mood; pay attention to rest and avoid overexertion.
3 Results
3.1 Observation items
3.1.1 TCM symptom score
According to the quantitative criteria of TCM symptom scoring, the symptoms of liver-qi stagnation and spleen-deficiency were scored[7]. The main symptoms were graded into 4 levels, scored 0, 2, 4 and 6 points respectively; the secondary symptoms were also graded into 4 levels, scored 0, 1, 2 and 3 points respectively, and the total score was obtained by adding up the component symptom scores, with higher scores indicating greater symptoms. The reduction rate of TCM symptom score was calculated according to the TCM symptom score. Reduction rate of TCM symptom score= (Pre-treatment TCM symptom score - Post-treatment TCM symptom score) ÷ Pre-treatment TCM symptom score × 100%.
3.1.2 Gastric emptying rate
The barium strip method was used to measure solid gastric emptying function before and after treatment,and then the gastric emptying rate was calculated[8].
3.1.3 Serum brain-gut peptides contents
Enzyme immunoassay was used to measure the contents of serum 5-HT and ghrelin.
3.2 Criteria for therapeutic efficacy
Clinically cured: The clinical symptoms and signs of patients disappeared or basically disappeared, and the reduction rate of TCM symptom score was ≥95.0%.
Markedly effective: The patient's clinical symptoms and signs improved significantly, and the reduction rate of TCM symptom score was ≥70.0% but <95.0%.
Effective: The clinical symptoms and signs of the patients were improved, and the reduction rate of TCM symptom score was ≥30.0% but <70.0%.
Invalid: The patient's symptoms and signs did not improve significantly, or even worsened, and the reduction rate of TCM symptom score was <30.0%.
3.3 Results
3.3.1 Comparison of therapeutic efficacy
The total effective rate was significantly higher in the treatment group than in the control group (89.4%versus 79.6%,P<0.05), (Table 2).
3.3.2 Comparison of the gastric emptying rate
The gastric emptying rate of the two groups increased significantly after treatment (bothP<0.01),and it was significantly greater in the treatment group than in the control group (P<0.01), (Table 3).
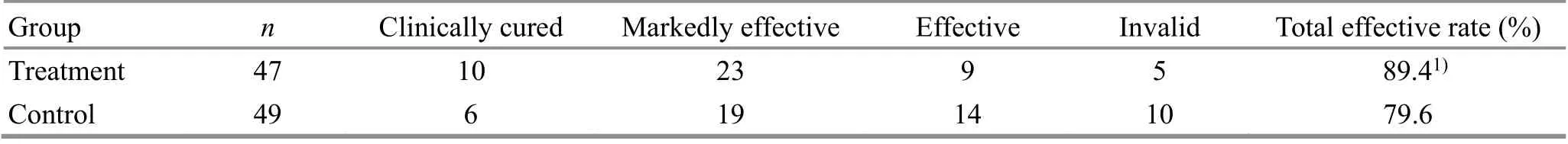
Table 2. Comparison of the therapeutic efficacy between the two groups (case)
Table 3. Comparison of the gastric emptying rate between the two groups ( ±s, %)

Table 3. Comparison of the gastric emptying rate between the two groups ( ±s, %)
Note: Compared with the same group before treatment, 1) P<0.01;compared with the control group after treatment, 2) P<0.01
Group n Before treatment After treatment Treatment 47 46.26±5.49 75.62±6.411)2)Control 49 47.47±5.30 71.45±6.761)
3.3.3 Comparison of the serum 5-HT and ghrelin contents
The serum 5-HT content of the two groups decreased significantly after treatment (bothP<0.01), and it was significantly lower in the treatment group than in the control group (P<0.05). The serum ghrelin content of the two groups increased significantly after treatment(bothP<0.01), and it was significantly greater in the treatment group than in the control group (P<0.05),(Table 4).
3.3.4 Correlation analysis between brain-gut peptides and gastric emptying rate
According to Pearson correlation analysis, a negative correlation (r=-0.59,P<0.01) was observed between serum 5-HT content and gastric emptying rate, and a positive correlation (r=0.64,P<0.01) was observed between serum ghrelin content and gastric emptying rate after acupoint sticking therapy.
Table 4. Comparison of the serum 5-HT and ghrelin contents between the two groups (±s, ng/mL)
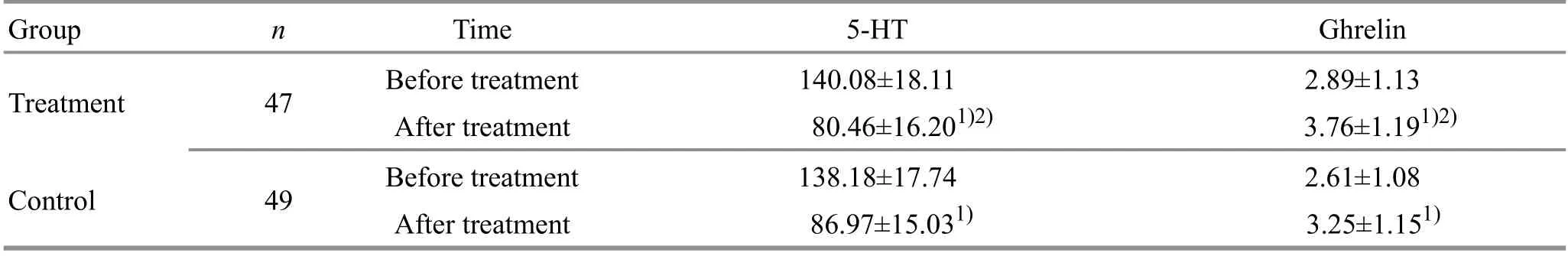
Table 4. Comparison of the serum 5-HT and ghrelin contents between the two groups (±s, ng/mL)
Note: Compared with the same group before treatment, 1) P<0.01; compared with the control group after treatment, 2) P<0.01
Group n Time 5-HT Ghrelin Treatment 47 Before treatment 140.08±18.11 2.89±1.13 After treatment 80.46±16.201)2) 3.76±1.191)2)Control 49 Before treatment 138.18±17.74 2.61±1.08 After treatment 86.97±15.031) 3.25±1.151)
4 Discussion
FD is the most common functional gastrointestinal disease in clinical treatment. It is characterized by high incidence, recurrent attacks and chronic prolongation,seriously affecting patients’ physical and mental health and quality of life. FD belongs to the category of‘fullness’ in TCM, and is located in the stomach. It is related to the liver and spleen, with liver-qi stagnation and spleen deficiency as the main pathogenesis[9]. The ointment used for acupoint sticking in this study is based on the empirical prescription Jianpi Tongjing Zhitong formula created by our department director Duan Ying-xi.Wu Zhu Yu(Fructus Evodiae),Bai Jie Zi(Semen Sinapis Albae),Ding Xiang(Flos Caryophylli) and other drugs were used to act on the Stomach and Conception Vessel for warming yang and regulating qi,strengthening the spleen and soothing the liver[10-11].The results of the study also showed that this therapy was effective and significantly superior to the control group (P<0.05), which can markedly improve the patients' digestive tract discomforts and gastric emptying rate.
The pathogenesis of FD has not yet been fully elucidated, and numerous studies in recent years have confirmed that the pathogenesis of FD is closely related to the dysfunction of the brain-gut axis[12-14]. Brain-gut peptide, as a peptide with dual distribution in the brain and gastrointestinal tract, is an important factor in the brain-gut axis and plays an important mediating role in the treatment of FD. 5-HT is an important neurotransmitter in the brain-gut axis that mediates gastrointestinal motility, secretion, and sensation, and is closely associated with symptoms such as gastroparesis,abdominal pain, diarrhea, and abnormal visceral sensation[15]. Ghrelin, a newly discovered brain-gut peptide, is also closely related to gastric motility, gastric emptying, and gastric acid secretion functions[16].
The results of this study suggested that acupoint sticking with Jianpi Tongjing Zhitong ointment could reduce the serum 5-HT content, increase the serum ghrelin content in FD patients due to liver-qi stagnation and spleen deficiency and showed better effect compared with the control group (P<0.05), indicating that acupoint sticking with Jianpi Tongjing Zhitong ointment can regulate peripheral brain-gut peptides.Consistent with our findings, existing studies have shown that traditional therapies, such as acupuncture and herbal medicine, may alleviate the clinical symptoms of FD patients by regulating peripheral 5-HT and ghrelin levels, thereby inhibiting visceral hypersensitivity and regulating various movements and functions of the gastrointestinal tract[5,17-18].
Our study further conducted a correlation analysis between clinical efficacy and brain-gut peptides by objective indicators. The results showed that serum 5-HT level was negatively correlated with gastric emptying rate (r=-0.59,P<0.01) and serum ghrelin level was positively correlated with gastric emptying rate (r=0.64,P<0.01) in FD patients after treatment, which proved the role of peripheral 5-HT and ghrelin in the treatment of FD by acupoint sticking with Jianpi Tongjing Zhitong ointment , and provided a more objective basis for their relationships. It can be seen that the pathogenesis of FD due to liver-qi stagnation and spleen deficiency and the mechanism of acupoint sticking therapy may be related to brain-gut peptides. The organism forms an interconnection between the gastrointestinal tract and the central nervous system under the action of braingut axis, and when there is an exogenous stimulus acting on the central nervous system, the sensory,motor and endocrine functions of the gastrointestinal tract are affected through its efferent nerves[19-20]. Some studies have confirmed that acupoint stimulation can promote gastric motility and gastric emptying and correct disturbances in gastric electrical rhythms, thus achieving the effect of regulating imbalances in the autonomic nervous system[21].
In summary, the emergence of brain-gut axis has raised the understanding of FD from a localized gastrointestinal level to a whole-body perspective. In this study, by observing the brain-gut peptide levelsin vivo, we searched for the targets of acupoint sticking with Jianpi Tongjing Zhitong ointment in treating FD,which provided a basis for further development of this therapy and also a new therapeutic idea for those who are intolerant to gastroprokinetic drugs.
Conflict of Interest
There was no potential conflict of interest in this article.
Acknowledgments
This work was supported by Research Project of Health and Family Planning Commission of Inner Mongolia Autonomous Region (內(nèi)蒙古自治區(qū)衛(wèi)生和計(jì)劃生育委員會(huì)科研項(xiàng)目, No. 201703065).
Statement of Informed Consent
This trial had been approved by the Ethics Committee of Inner Mongolia Hospital of Traditional Chinese Medicine(Approval No. nmgzy-2017-08). Informed consent was obtained from the patients in this study.
Received: 29 October 2020/Accepted: 19 December 2020
 Journal of Acupuncture and Tuina Science2021年5期
Journal of Acupuncture and Tuina Science2021年5期
- Journal of Acupuncture and Tuina Science的其它文章
- Exploring the effect of acupuncture plus mild hypothermia on miRNA-204 and its target gene expressions in CIRI rat brain tissues based on MAPK signal pathway
- Experimental observation of effects of acupoints,cone numbers and durations of moxibustion with different moxibustion methods on skin surface and inside temperature
- Therapeutic massage for knee osteoarthritis:a systematic review and meta-analysis of randomized controlled trials
- Clinical efficacy observation of ‘Tong Du Yun Pi’manipulation for infantile diarrhea in autumn
- Clinical observation on moxibustion therapy plus tuina in treating children with recurrent respiratory tract infections due to qi deficiency of spleen and lung
- Effects of acupuncture plus language training on language function and cerebral blood flow in patients with motor aphasia after ischemic stroke
