Clinical application of ultrasound-guided selective proximal and distal brachial plexus block in rapid rehabilitation surgery for hand trauma
Jin Zhang, Man Li, Hai-Bin Jia, Lan Zhang
Jin Zhang, Man Li, Hai-Bin Jia, Lan Zhang, Department of Anesthesiology, Sichuan Orthopedic Hospital, Chengdu 610041, Sichuan Province, China
Abstract
Key words: Selective brachial plexus block; Ultrasound; Hand trauma; Rapid rehabilitation surgery
INTRODUCTION
The hand is one of the most complex and refined pieces of natural engineering in the human body. In the daily life, the hand is used much more frequently than other parts in the human body. Thus, hands are the most frequent body parts injured in the daily life. For patients with hand trauma, immediate and appropriate treatment could result in a favorable prognosis. This type of population mostly requires surgery. Surgery for hand trauma consists of procedures such as surgical anastomosis and debridement and stitching, which has a high anesthetic requirement[1,2]. General anesthesia is not recommended because it has many side effects which may affect patient outcomes.Instead, brachial plexus block, a regional anesthesia technique, is often used in the upper limb and hand surgery. However, incomplete block and failure of anesthesia always happen due to the fact that it involves blind injection of local anesthetic.Ultrasound-guided selective proximal and distal brachial plexus block may help to solve the problem[3]. In the present study, the efficacy of ultrasound-guided selective proximal and distal brachial plexus block in patients with hand trauma undergoing rapid rehabilitation surgery at our hospital was researched between January 2018 and June 2019.
MATERIALS AND METHODS
Participants
A total of 68 patients with traumatic hand injuries treated at our hospital from January 2018 to June 2019 were selected. Patients eligible for the study were identified by the following criteria[4]: Clinically confirmed with hand trauma; graded as American Society of Anesthesiologists physical status I to II; participating in the research voluntarily and signing the relevant statements; approved by the hospital ethics committee. Patients who have contraindications to anesthesia, patients who cannot undergo surgery, and those who lack complete clinical data were excluded from the research.
They were divided into an observation group and a control group with 34 patients in each group by using the random number table method. There were 23 male patients and 11 female patients in the observation group (age: 23 to 75 years; average age: 45.15 ± 10.45 years; weight: 37 to 80 kg; average weight: 59.25 ± 10.20 kg),including 1 patient with blast injuries to the hand, 8 with broken hand, 14 with hand fracture, and 11 with avulsion of the soft tissue. In the control group, 24 patients were male and 10 patients were female (age: 21 to 78 years; average age: 45.26 ± 10.38 years;weight: 36 to 81 kg; average weight: 59.21 ± 10.25 kg), including 2 patients with blast injuries to the hand, 9 with broken hand, 13 with fracture, and 10 with avulsion of the soft tissue. There was no significant difference in the demographic characteristics between the two groups.
Patients in the observation group underwent ultrasound-guided selective proximal and distal brachial plexus block. Depending on the requirements during the operation, the median, ulnar, or radial nerve block was performed on the basis of brachial plexus block performed against the clavicle. The amount of anesthetic required for the distal brachial plexus block was 20 mL of 1.3% lidocaine plus 10 mL of 1% ropivacaine. The amount of anesthetic required for the median, ulnar, and radial nerve block was 5 to 10 mL of 1% lidocaine.
The median nerve was blocked usually in the operation at the site between the tendons of palmaris longus and flexor carpi radialis with the forearm supinated.Along the imaginary line between the humerus and lateral condyle, the pulse of the brachial artery was identified. Around 0.7 cm inside the artery was the site of the median nerve block. In the distal side, about 2.5 cm away from the point, the needle was tilted up to an angle of 20 degrees and inserted. The injection was begun when the abnormal sensation was felt.
The ulnar nerve was blocked usually in the operation at the site of hypothenar region or little finger. The patient lied on his back and externally rotated the arm, with the elbow flexed. The ulnar nerve sulcus was fixed by doctor’s thumb and the needle was inserted after it was found. When the patients felt an electric sensation in the little finger and ring finger, the injection was performed.
The radial nerve block was usually achieved in the surgery at the site of hypothenar region or the back of the hand. Subcutaneous infiltration for anesthesia was performed at about four-finger breadth away from the outside of the humerus. This site toward the humerus was also chosen for needle insertion. The electric sensation through the thrum and the hand back can be felt for it is the place where the radial nerve penetrates the lateral intermuscular septum. When abnormal sensation was got,sector shaped nerve block of the brachial plexus was performed on the patient.
In the control group, nerve block of the brachial plexus was performed using 20 mL of 1.3% lidocaine plus 10 mL of ropivacaine. Brachial plexus nerve was blocked at the site of the clavicle. The needle was inserted inward, backward, and downward at the height of 1 to 2 cm vertically above the midpoint of the clavicle. The injection was performed when the abnormal sensation was felt. If the anesthesia efficacy was not perfect enough, additional local anesthetic of 0.5% lidocaine was used.
Measurements
The measurements for the research included efficacy of pain relief[5], intraoperative complications, healing time for wounds, and length of hospital stay. Pain relief was rated as “excellent” (pain free and do not need additional analgesia), “very good”(tolerable mild pain and discomfort and do not need additional analgesia), “good”(intolerable pain and need additional analgesia), and “poor” (intolerable pain and additional analgesia did not have much efficacy in reducing pain and the operation was disturbed by the pain). The percentage of cases with analgesia graded as“excellent or very good” was estimated and compared between the two groups.Intraoperative complications included respiratory depression, hypertension,hypotension, and tachycardia.
Statistical analysis
Metering data and counting data are expressed as the mean ± SD and percentages (%),respectively. The data and differences between the two groups were analyzed bytandχ2tests using SPSS software 18.0. APvalue < 0.05 was considered statistically significant.
RESULTS
Analgesic efficacy
A comparison of the analgesic efficacy between the two groups is shown in Table 1.The percentage of cases with analgesia graded as “excellent or very good” was higher in the observation group than in the control group (P< 0.05).
Complications
In terms of incidence of complications, the observation group was obviously lower than in the control group (P< 0.05, Table 2).
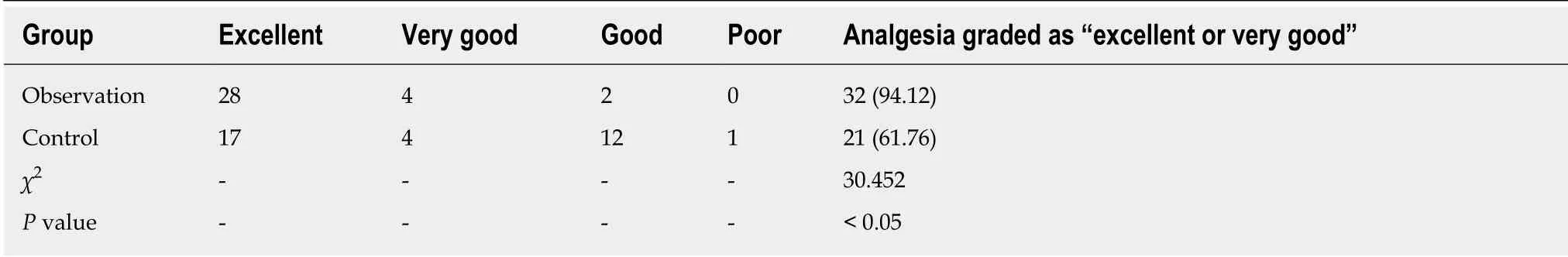
Table 1 Analgesic efficacy in the two groups, n (%)
Healing time for wounds and length of hospital stay
The healing time for wounds and length of hospital stay were lower in the observation group than in the control group (P< 0.05, Table 3).
DISCUSSION
Hand trauma is very common in the clinical practice. Surgery is the predominant therapy for it. During the surgery, anesthesia is essential to ensure its success. Brachial plexus block is one of the mostly used types of anesthesia. However, the anesthesia efficacy of this method always depends on the skill of the clinicians because it is performed under blind investigation. Any slight error may cause incorrect puncture,complications, and repeated needle insertion[6,7]. Thus, single brachial plexus block cannot meet the needs of the clinical surgery. It is necessary to find more rational and scientific anesthesia methods.
Ultrasound-guided puncture include two ultrasound imaging planes, namely, outof-plane ultrasound guidance and in-plane imaging. Ultrasound-guided plexus block has various advantages including accurately identifying the position and structure of plexus, less irritation, less pain, and more response. Anatomical variation associated difficulty of puncture can be solved. It is also applicable for some children,unconscious patients, and some patients using nerve blocks or general anesthesia[8].
The success rate of anesthesia is high, anesthesia efficacy is good, and the onset of action is short for ultrasound-guided plexus block. To some extent, it can reduce the dose of anesthetic[9]. In addition, the incidence of complications is low for the operation. Nerves, vessels, pleura, and other issues can be easily shown in the imaging, which can effectively avoid conditions such as nerve and vessel injury[10].However, the following matters should be paid attention to in the practice: The needle insertion site should be observed and identified at the beginning of the operation;choosing the best ultrasonic frequency for the operation to obtain the clearest image;and slight movements of the ultrasound probe may affect the efficacy of imaging.Thus, clinicians are required to have a thorough grasp of the techniques such as color flow imaging, image enlargement, image focus, and image saving[11].
Supraclavicular nerve block is a common brachial plexus block. The operation is easy. The patient is asked to lie on their back. Then, the clinician puts a thin pillow under the shoulder of the patient to make his/her head turn to one side. Conventional disinfection is performed. The clinician should find the midpoint of the clavicular first. Local anesthetic is administered to form skin mound at a depth of approximately 1 cm from the skin at the midpoint. The needle 3.5 cm is pushed inward, backward,and downward to find the first rib. After the first rib is found, the needle is inserted.The rib is touched to detect and observe the patient’s abnormal feeling. If the patient has no obvious discomfort, the anesthetic is injected along the rib[12].
Perrettaet al[13]showed that selective brachial plexus block can be performed by selecting the specific nerve branches according to the position of the wound or injecting anesthetic with different anesthesia time for different nerves in order to promote early active movement recovery and wound pain relief. Carbocaine or lidocaine is often used for brachial plexus block abroad. For the short-term surgery,chloroprocaine is always applied and for the long-term surgery, docaine, bucaine, or bupivacaine is always applied. The effects of these anesthetic drugs can last 5 to 10 h and even 18 to 20 h. Ropivacaine or lidocaine is usually used in the clinical practice in China, which shows good efficacy.
In the present study, all the patients were given anesthetics at the lowest effective concentration. Using local anesthetic of low concentration and high volume of distribution helps to ensure adequate volume in the sheath. Two studies[14,15]reported that brachial plexus block alone may be associated with incomplete anesthesia or anesthesia failure, which needs additional local anesthesia or intravenous adjuvant drugs. However, in the present study, we observed that using additional regionalanesthesia may have an effect on the surgical field of vision, which may further disturb the operation. Moreover, intravenous adjuvant drugs may cause respiratory depression, which is harmful to perioperative management.
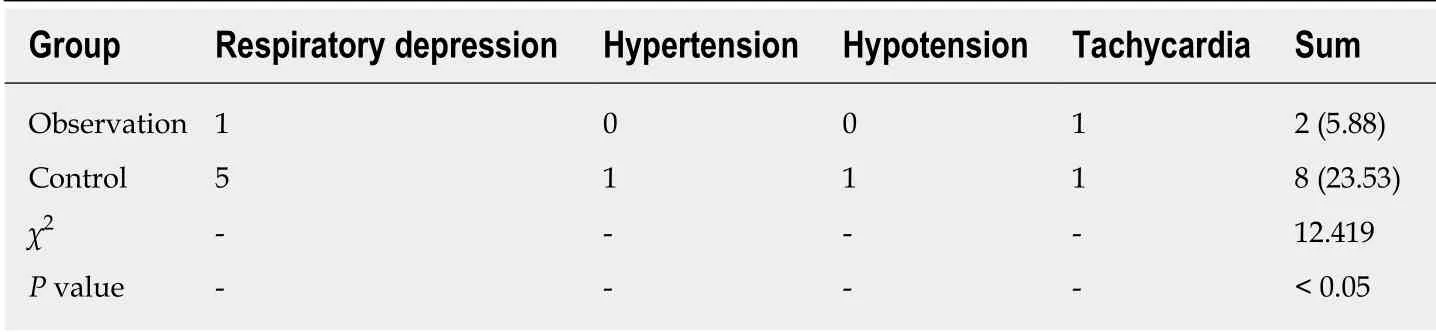
Table 2 The incidence of complications in the two groups, n (%)
In the current study, the percentage of cases with analgesia graded as “excellent or very good” was higher in the observation group than in the control group and the incidence of intraoperative complications was lower in the observation group than in the control group, suggesting that ultrasound-guided selective proximal and distal brachial plexus block can improve pain relief and reduce the incidence of intraoperative complications. It can make up for the defects of brachial plexus block alone and avoid affecting the surgery. What’s more, the healing time for wounds and length of hospital stay were lower in the observation group than in the control group,which can be explained by the benefits of ultrasound-guided selective proximal and distal brachial plexus block including good pain relief efficacy, muscle relaxation,inhibition of vasoconstriction, improved fracture associated vascular dysfunction, and speedy recovery[16].
Ultrasound-guided selective proximal and distal brachial plexus block used in this study confirmed the quality and safety of anesthesia and reduced the risk of incomplete anesthesia. Brachial plexus block have many advantages. It is noninvasive,repeatable, objective, and accurate, and the anesthetic-induced changes are able to be tracked with a high success rate and low incidence of complications. In spite of this,the anesthesiologist should acquire or increase their knowledge of vascular ultrasonography as well as practical skills. Further study may be warranted to investigate the scientific monitoring technology for the pain relief.
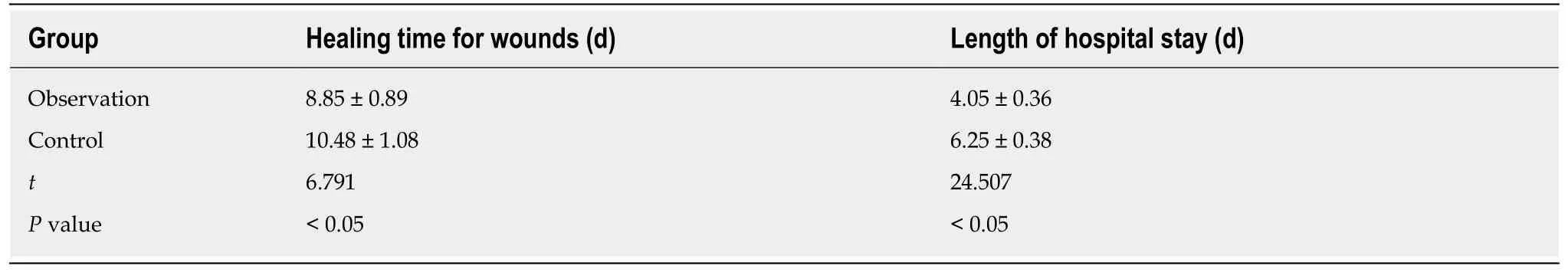
Table 3 Comparison of wound healing time and length of hospital stay between the two groups
ARTICLE HIGHLIGHTS
Research background
Hand surgery procedures are complex and challenging for they may involve many nerves. To modify the anesthesia efficacy, ultrasound-guided regional anesthesia is always applied in the surgery in this population. The published outcome data on usage of ultrasound-guided selective proximal and distal brachial plexus block in patients undergoing surgery for hand trauma is limited.
Research motivation
What benefits does ultrasound-guided selective proximal and distal brachial plexus block have in rapid recovery surgery for hand trauma? Does it really improve the anesthesia efficacy as well as reduce the potential side effects and complications? With these questions, a case-controlled study was conducted.
Research objectives
In this study, the authors aimed to explore the efficacy of ultrasound-guided selective proximal and distal brachial plexus block in rapid recovery surgery for hand trauma.
Research methods
Patients with traumatic hand injuries who required surgery were included. They were assigned to an ultrasound-guided selective proximal and distal brachial plexus block group and a conventional brachial plexus block group. The anesthesia efficacy, pain, and outcomes were compared.
Research results
Patients with ultrasound-guided selective proximal and distal brachial plexus block showed better analgesic efficacy than the control group. Moreover, the incidence of complications,wound healing time, and length of hospital stay were lower in the observation group than in the control group.
Research conclusions
Ultrasound-guided selective proximal and distal brachial plexus block used in this study confirmed the quality and safety of anesthesia and reduced the risk of incomplete anesthesia and pain in patients undergoing surgery for hand trauma.
Research perspectives
To achieve safe anesthesia, patients should be closely monitored and observed when ultrasoundguided selective proximal and distal brachial plexus block was performed. Associated guidelines and expert consensus should be developed based on the clinical experience to avoid the negative side effects of this form of local anesthesia.
 World Journal of Clinical Cases2020年11期
World Journal of Clinical Cases2020年11期
- World Journal of Clinical Cases的其它文章
- Tumor circulome in the liquid biopsies for digestive tract cancer diagnosis and prognosis
- Isoflavones and inflammatory bowel disease
- Cytapheresis for pyoderma gangrenosum associated with inflammatory bowel disease: A review of current status
- Altered physiology of mesenchymal stem cells in the pathogenesis of adolescent idiopathic scoliosis
- Association between liver targeted antiviral therapy in colorectal cancer and survival benefits: An appraisal
- Peroral endoscopic myotomy for management of gastrointestinal motility disorder
