Distraction arthroplasty in osteoarthritis of the foot and ankle
Sherif Dabash, Joshua R Buksbaum, Austin Fragomen, S Robert Rozbruch
Sherif Dabash, Austin Fragomen, S Robert Rozbruch, Limb Lengthening and Complex Reconstruction Service, Weill Cornell Medical College Department of Orthopaedic Surgery,Hospital for Special Surgery New York, NY 10021, United States
Joshua R Buksbaum, SUNY Downstate Health Sciences University, College of Medicine,Brooklyn, New York, NY 11226, United States
Abstract
Key words: Distraction arthroplasty; First metatarso-phalangeal joint arthritis; Second tarsometarsal joint arthritis; Ankle arthritis; Subtalar arthritis; Post-traumatic osteoarthritis
INTRODUCTION
Osteoarthritis is a degenerative condition affecting articular joints causing loss of mobility and independence due to pain and swelling in the affected joint. There are a multitude of causes for the onset of osteoarthritis and treatments for its progression and symptoms. Post-traumatic osteoarthritis (PTOA) comprises a large portion of osteoarthritis cases affecting the ankle and foot[1]. The treatment of osteoarthritis in the ankle, subtalar, 1stmetatarsophalangeal (MTP) joint, or 2ndtarsometatarsal joints(TMT) joint with fusion or arthroplasty have been well documented[1-6]. Distraction Arthroplasty was first described as a conservative treatment for arthritis of the hip in young patients[7]. Since then, there has been a growth in interest related to this newer surgical technique, and numerous studies have described its application as a treatment for PTOA in the ankle and foot. Distraction arthroplasty can be used to treat PTOA of these joints as a viable joint preservation alternative, especially in younger patients who are not candidates for either fusion or arthroplasty[6,8-12].
Unlike the knee, most cases of ankle arthritis are classified as post-traumatic. Ankle sprains are one of the most common athletic injuries and can lead to PTOA of the ankle, and there are few treatments to delay or reverse the progression of posttraumatic ankle arthritis[13]. In the ankle, or the Tibio-talar joint, fusion and arthroplasty are well documented treatments for PTOA[1,6,14]. In addition to the ankle,PTOA is prevalent in the subtalar joint. Hindfoot fractures of the talus and calcaneus can lead to persistent pain and the progression of PTOA. In the subtalar, or Talocalcaneal joint, fusion and arthroplasty are well documented treatments for PTOA[1,12,15]. Osteoarthritis of the 1stMTP joint can often be debilitating, as it bears approximately 50% of the body’s weight during ambulation. Osteoarthritis of the 1stMTP joint can be caused by Hallux Rigidus or Hallux Valgus deformities, in addition to trauma. Fusion and arthroplasty are well documented treatments for PTOA in the first MTP joint[2,3,16-19]. The effectiveness of distraction arthroplasty in treating PTOA of the 1stMTP has been documented[8]. Osteoarthritis can affect the TMT joints due to several causes, including trauma, deformity, and prior foot surgery[4,5,20,21]. PTOA of the second TMT joint is often painful and difficult to treat. In the second TMT joint,fusion and arthroplasty are well documented treatments for PTOA[4,5]. Currently, there are no studies investigating the use of distraction arthroplasty to treat PTOA in the second TMT. Distraction Arthroplasty is a viable joint preserving surgery alternative to fusion and arthroplasty to treat post-traumatic osteoarthritis and is especially suitable for younger and active patients[6,8-10,22-26].
CLINICAL PRESENTATION
Patient A: Ankle distraction for posttraumatic arthritis
Patient A is a 52-year-old female who presented with left ankle PTOA. She complained of gradual pain developing in her ankle after multiple sprains and wear and tear from an active lifestyle. This pain was treated with a Watson Jones procedure 29 years prior, and an ankle distraction with external fixation performed one year prior, in addition to tarsal tunnel release and arthroscopic cheilectomy. The patient developed an equinus contracture due to her time spent with her ankle immobilized during distraction. She was diagnosed with advanced PTOA of the left ankle, in addition to an equinus contracture. Our decision was to take on a joint-preservation course of action, to help the patient continue to enjoy her active lifestyle. Our plan included arthrotomy and cheilectomy, microfracture, ankle distraction, and bone marrow aspirate concentrate (BMAC) injection to treat the ankle PTOA, in addition to release of the gastrocnemius and soleus to correct the equinus contracture.
On physical exam, pre-operative range of motion (ROM) in the left ankle was -10 degrees of dorsiflexion (DF) to 40 degrees of plantarflexion (PF). Pre-operative ROM in the left subtalar joint was from 5 degrees of inversion to 5 degrees of eversion. Postoperative ROM n in the left ankle was 5 degrees of DF to 40 degrees of PF, and ROM in the subtalar joint was 10 degrees of inversion to 5 degrees of eversion. After surgery, patient continued extremely active lifestyle and did report taking some pain medication to treat pain after activity, however she stated that her pain levels had been significantly reduced through her surgical treatment. Patient is now nine years from date of distraction arthroplasty frame removal and is doing well with no pain(Figures 1-4).
Patient B: Ankle distraction + correction of flat foot deformity
56-year-old female who presented with right ankle PTOA. She complained of pain in her ankle at 5/10 after an inversion injury to her ankle sustained 16 years prior while running. She was diagnosed with an Osteochondritis Dissecans lesion on the medial aspect her talar dome. She also had a flat foot deformity. She was recommended ankle fusion by another surgeon, however our decision was to undertake distraction arthroplasty to offload the ankle joint and the Osteochondritis Dissecans lesion, while simultaneously placing an arthroeresis screw to treat her flat foot deformity.
On physical exam, pre-operative ROM in the ankle was 0 degrees of DF to 50 degrees of (PF). Pre-operative ROM in the subtalar joint was 40 degrees of inversion to 10 degrees of eversion. Pre-operative self-reported pain level was 5/10, and the patient was taking Tylenol 1000 mg BID and 5 mg of Oxycodone daily for pain.
On physical exam post-operatively, ROM was recorded as 20 degrees of DF to 40 degrees of PF in the ankle and subtalar ROM was 20 degrees of inversion to 20 degrees of eversion. The patient reported no pain after surgery and did not take any pain medications. Patient is now two years from frame removal and is doing well(Figures 5 and 6).
Patient C: Sub-talar distraction
Patient C is a 45-year-old female who presented with PTOA of the right sub-talar joint after sustaining a fracture and dislocation of the talus. Upon examination, she presented with pain worsening with increasing activity on the lateral side of the foot and a limp due to pain. On physical examination, ROM in the right ankle was 0 DF to 70 degrees PF, and ROM in the right sub-talar joint was 20 degrees of inversion and 0 degrees eversion. Patient did not see improvement in pain after conservative treatment with PRP injections. Patient was offered sub-talar fusion or distraction.Because of her age, she elected to proceed with distraction. After surgery, ROM in the sub-talar joint improved to 15 degrees of inversion and 10 degrees of eversion.Additionally, patient reported no pain after surgery and has returned to her normal level of activity. Patient is now three years post removal of frame and is doing well with no pain (Figures 7-11).
Patient D: 1st MTP distraction
Patient D is a 48-year-old male who presented to the office with hallux rigidus deformity of the right first MTP joint. The patient reported pain and difficulty wearing normal shoes. Patient did not see improvement with conservative treatments of orthotics and injections of the first MTP joint. The patient was presented with multiple treatment options; fusion, cheilectomy, cartiva, and distraction of the first MTP joint to treat pain and hallux rigidus. After discussion with the patient, the patient elected to proceed with cheilectomy and distraction arthroplasty of the first MTP joint with external fixation. After surgery, the patient reported improvement of pain and ROM. Patient is now six months post removal of the distraction arthroplasty frame and is doing well with no pain (Figures 12-14).
Patient E: 2nd TMT distraction
Patient E is a 66-year-old male who presented with flat foot and dorsal pain in his left foot caused by PTOA and synovial cysts in his second (TMT) joint. Patient reported his pain levels as ranging from four to six out of ten and taking ibuprofen for pain.Patient was recommended midfoot fusion at the second TMT, but after his satisfaction with ankle and sub-talar distraction performed by our physicians on the contralateral limb, he elected to proceed with distraction arthroplasty of the second TMT. Planned treatment included distraction of the second TMT, debridement, and BMAC injection in the second TMT, in addition to insertion of arthroeresis screw and gastrocnemius lengthening to treat flat foot deformity. After surgery, patient reported no pain and did not take any medication for pain. Patient is now two years post removal of the frame and is doing well with no pain (Figures 15-18).
SURGICAL TECHNIQUE
Ankle distraction
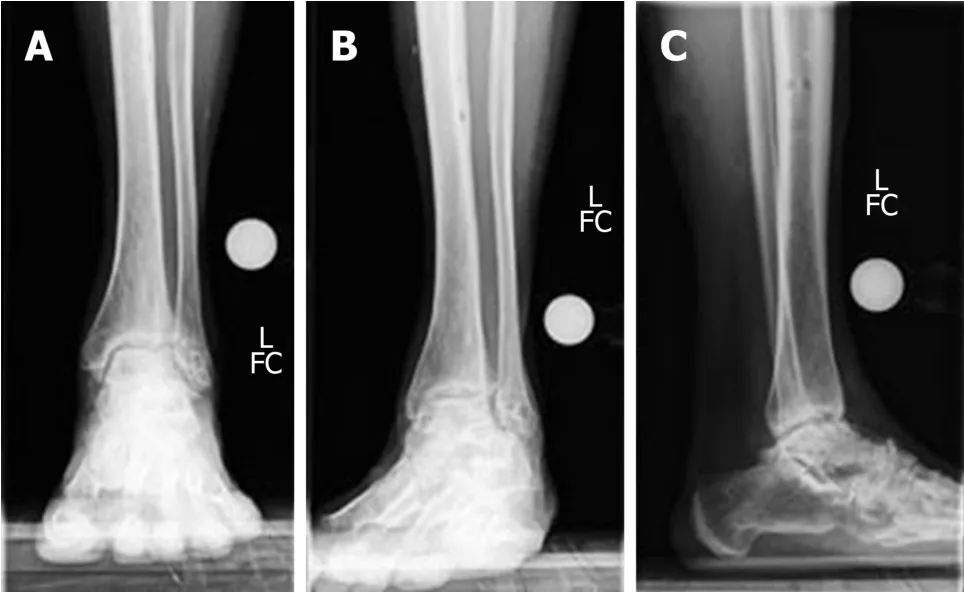
Figure 1 Pre-operative standing X-rays demonstrating post-traumatic osteoarthritis of the ankle joint.
The ankle distraction frame is simply composed of two rings connected together with two threaded rods and a locking rod that connects the footplate to the proximal adjustable ring which allows gradual DF. A tibial ring is chosen that gives two fingerbreadths of space circumferentially between the skin and the ring. The proximal ring is secured with two 6-mm hydroxyapatite-coated pins. A 4.8-mm drill bit is used to fix the first pin approximately 6 cm proximal to the medial malleolus directly anterior in the tibial crest and perpendicular to the shaft of the tibia. Surgeon has to avoid unicortical pins that miss the medullary canal and put the bone at risk of fracture. It is then secured to the ring with a three-hole cube. Intraoperative fluoroscopy is used to confirm that the ring is perpendicular to the axis of the tibial shaft. Universal hinges are then applied in line with a K-wire which approximates the Inman axis from the tip of the lateral malleolus to the tip of the medial malleolus, in a posterolateral-to-anteromedial direction.
A footplate is secured by olive wires one inch proximal and parallel to the plantar aspect of the foot. A locking rod connects the footplate to the proximal adjustable ring,which allows for gradual DF to correct equinus contractures. Threaded rods connect the two rings where the square nuts are placed on the proximal part of the rod.Measurement of the length of the threaded rod above the square nut is important to ensure that the foot/ankle is back into neutral position after ROM exercises. Acute distraction of 3 mm is done intraoperatively by turning the square nuts on the proximal ring. Acute distraction beyond that is not recommended to avoid neurologic traction injury; acute correction of equinus contracture is avoided for the same reason.
Another 2 mm of distraction is done on postoperative day one when normal postoperative plantar sensation is confirmed. Another one mm on postoperative day two will be done. During the 2 wk visit, another 1 to 2 mm of distraction is done if needed. The total distraction in the frame is about 6-8 mm. The ROM exercises (15 repetitions/session) should be done by unlocking the ring four times daily.
In addition to distraction, the senior authors injects BMAC into the ankle joint and routinely do microfracture of the joint. Clinical data regarding the mechanism of action of hyaline cartilage regeneration are lacking, however, senior authors feel that these adjunctive procedures optimize healing and gives better results[9]. Future research should be directed towards comparing the benefit of adding biologics in the form of BMAC or not.
Sub-talar distraction
Sub-talar distraction begins with a 4 cm anterior skin incision is made over the lateral hindfoot. Dissection is carried down anterior to the peroneal tendons. The posterior facet and sinus tarsi of the joint are visualized. Osteophyte along the lateral talus and calcaneus are excised. The joint is inspected, and a 1.8 mm wire is used to make multiple drill holes for microfracture while cooled with saline in the talus and in the tibia. The holes are spaced by 5 mm. Furthermore, a 4 mm micro burr is used to remove a thin layer of hard subchondral bone. The subtalar joint is mobilized from 20 degrees of inversion to 15 degrees of eversion. A 3 cm × 3 cm collagen sponge is soaked in BMAC and is inserted into the distracted sub-talar joint.
The ankle distraction frame is then applied. A 155 mm frame and ring are applied to the distal third of the tibia, orthogonal to the tibial axis, and stabilized with two anteromedial half pins. The half pins are 6 mm hydroxy appetite coated pins placed after drilling with a 4.8 mm drill. The two feet rings are attached for fixation to the talus and calcaneus. Opposing olive wires are placed in the talus and in the calcaneus-4 in total- and are attached to the frame and tensioned. Acute distraction of the subtalar joint is then carried out, with 4 mm applied acutely by distracting between the two feet rings. The ankle and foot are both assessed for neutral position, and distraction of the sub-talar joint is confirmed with intra-operative fluoroscopy.
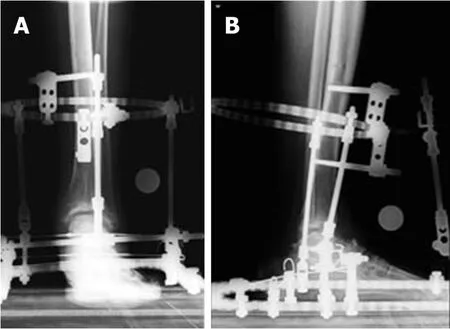
Figure 2 Post-operative standing X-rays demonstrating distracted ankle joint and distraction frame.
1st MTP distraction
First MTP joint distraction begins with a 3 cm dorsal skin incision made over the talus neck. Dissection is then carried down to a palpable prominence, and the extensor retinaculum is incised. The superficial peroneal nerve is protected, the tendons are retracted, and the distal surface of the talus is assessed for osteophytes, which are then excised. Intra-operative fluoroscopy allows for confirmation of complete removal of the osteophyte.
Next, a 4 cm medial skin incision is made across the metatarsophalangeal joint, and dissection is carried down to the medial capsule, which was longitudinally incised.The capsule is peeled off the medial side of the metatarsal head and reflected dorsally.The dorsal surface of the metatarsal head and the proximal phalanx are assessed for osteophytes, which are then excised. Medial eminence is also excised using a microsagittal saw. The MTP joint is then, subluxated, allowing for inspection of the articular cartilage. Inspection of the joint showed a 1 cm × 5 mm area of grade 4 full thickness loss of cartilage on the metatarsal head and an area of 5 mm × 5 mm of full thickness cartilage loss on the proximal phalanx. A 1.6 mm wire is used to perform microfracture while cooled with saline.
Fixator is then used to span the first MTP joint from a dorsal approach. A 3 mm self-drilling pin is placed dorsal to plantar in the proximal phalanx. Next, with the help of the frame for guidance, a second pin is placed parallel in the axial plane, but perpendicular to the metatarsal. This is also a 3 mm self-drilling pin. These are the most proximal and distal pin and are defined by the orientation of the fixator. The pin clamps are then used to add additional pins in the metatarsal and also in the proximal phalanx. Placement and stability of the pins are confirmed. The fixator is then applied and fastened. The fixator is placed in line with the axis of the joint in the coronal and sagittal planes. Three point five mm of distraction is then applied across the joint. The angle between the metatarsal and phalanx is assessed, and was reported to be within normal range at 15 degrees of DF. Lastly, intra-operative fluoroscopy is used to guide a spinal needle into the joint and to inject 3 mL of BMAC into the joint.
2nd TMT distraction
Second TMT distraction begins with a two and half cm skin incision over the dorsum of the joint and dissection is carried down to the joint. The joint is exposed,capsulotomy is performed, and the joint is visualized and assessed. Advanced arthrosis was noted of the joint. Using a 1.6 mm wire, microfracture is performed of the middle cuneiform and of the second metatarsal part of the joint while cooled with saline.
A mini rail fixator is then applied with pins coming in at a different plane from the original incision. Using 2.0 mm threaded pins, one pin is inserted into the middle cuneiform; this is the reference pin. This pin is placed orthogonal to the joint in a sagittal plane and is well positioned within the middle cuneiform. The mini rail external fixator is then applied and guides the insertion of a second metatarsal pin,also 2.0 mm. The placement and alignment of the two pins with the foot and fixator are assessed, and both were determined to be satisfactory. Additional pins are placed in the proximal and distal pin clamps, allowing for excellent purchase. Lastly, the external fixator is then applied to allow for intra-operative distraction. Three mm of distraction is placed across the joint and assessed by direct vision.
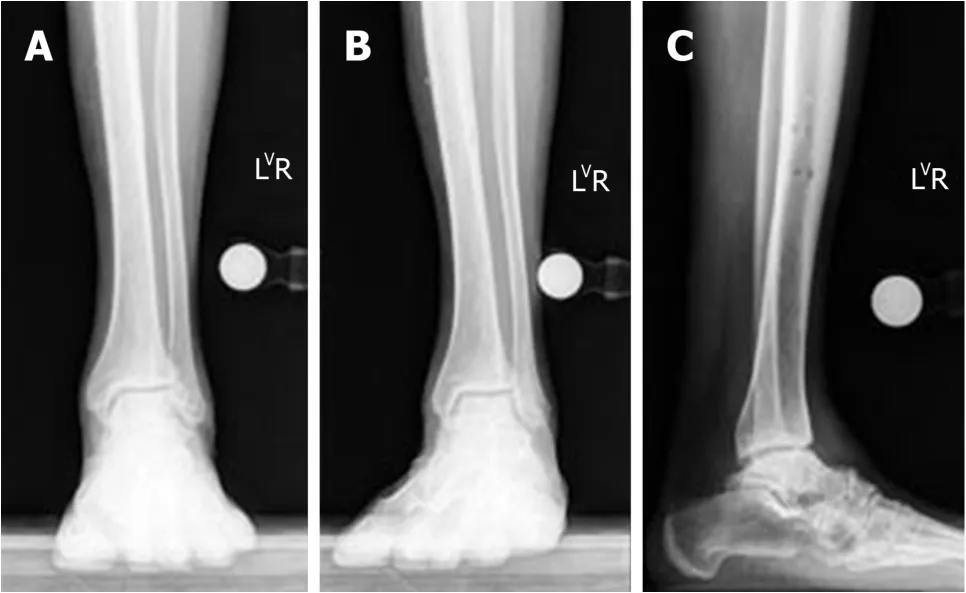
Figure 3 One-year post-operative standing X-rays demonstrating improved ankle joint space and articular surface after distraction.
POST OPERATIVE PERIOD AFTER ANKLE DISTRACTION
The patient is allowed full weight bear as tolerated with crutches in the postoperative period. The neutral position is marked on the hinge, and the patient is taught how to unlock the hinge and do active assisted ROM exercises with the aid of foot strap. Later on, the patients are encouraged to ambulate with the frame’s hinge unlocked. Acute distraction more than 3 mm is not recommended. We usually distract 3 mm in the operating room, and any residual distraction (2-4 mm) is done by the physician while the patient is still in the hospital, or at the first clinic visit 2 wk postoperative. Frame is kept in distraction for 12 wk as there is no added benefit to keep it for longer time.
LIMITATIONS
Distraction arthroplasty results in good functional outcomes at medium to long term follow up. The addition of microfracture seems to create functional outcome deterioration, whereas the addition of a biologic agent either BMAC or PRP appears to benefit earlier return to function. Randomized clinical trials with long term follow up are needed to compare if microfracture accompanied with the distraction is beneficial or not.
This case series represents our center experience with this technique. Larger multicenter studies are needed to show the effectiveness of our technique with comparison to others, and also comparing each surgeon’s preference of adding biologics in form of BMAC or not and reporting the statistical differences between different techniques.
CONCLUSION
Our case series aimed to describe the surgical technique of distraction arthroplasty of different joints in the foot and ankle, and their ability to improve patient outcomes. It is an alternative procedure to preserve the native joints instead of fusing or replacing the arthritic joint. Based on our experiences, distraction arthroplasty is a viable and effective treatment for PTOA in the ankle, subtalar, 1stMTP, and 2ndTMT joint.Distraction arthroplasty can prolong the integrity of the joints of the foot and ankle,and in our experiences, if combined with injection of BMAC can improve the outcomes of distraction arthroplasty procedure and prolong the time until the patient needs further surgical intervention, in the form of fusion or arthroplasty.
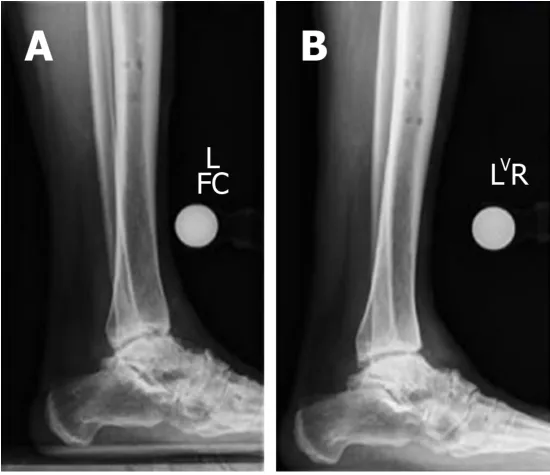
Figure 4 Comparison of pre and one-year post-operative standing X-rays demonstrating improved ankle joint space and articular surface after distraction.

Figure 5 pre-operative standing X-rays and magnetic reconnaissance imaging, in addition to intra-operative fluoroscopy of the right ankle after anterior cheilectomy and distraction.
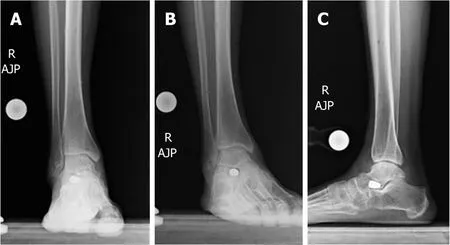
Figure 6 One-year post-operative standing X-rays of the right ankle, demonstrating improved ankle joint space, articular cartilage, and joint alignment one year after removal of frame.

Figure 7 Pre-operative standing X-rays of the right subtalar joint demonstrating sub-talar joint space narrowing and post-traumatic osteoarthritis.

Figure 8 Pre-operative computed tomography scans of the right subtalar joint demonstrating sub-talar arthritis and sclerosis of the articular surface.
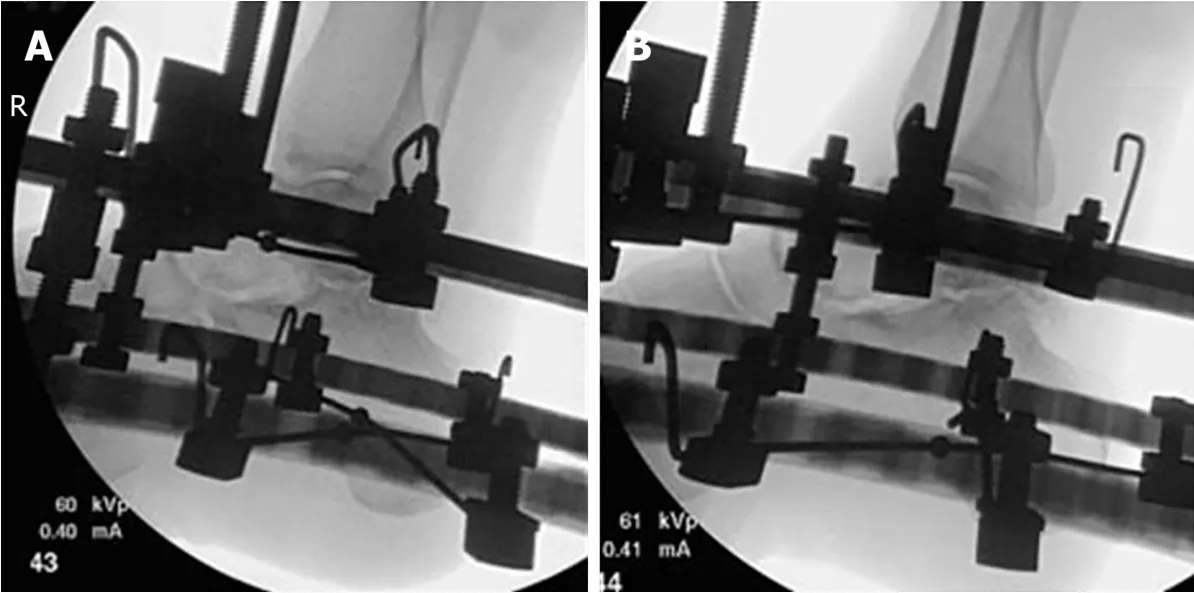
Figure 9 Intra-operative fluoroscopy of the right sub-talar joint before and after application of intraoperative distraction.
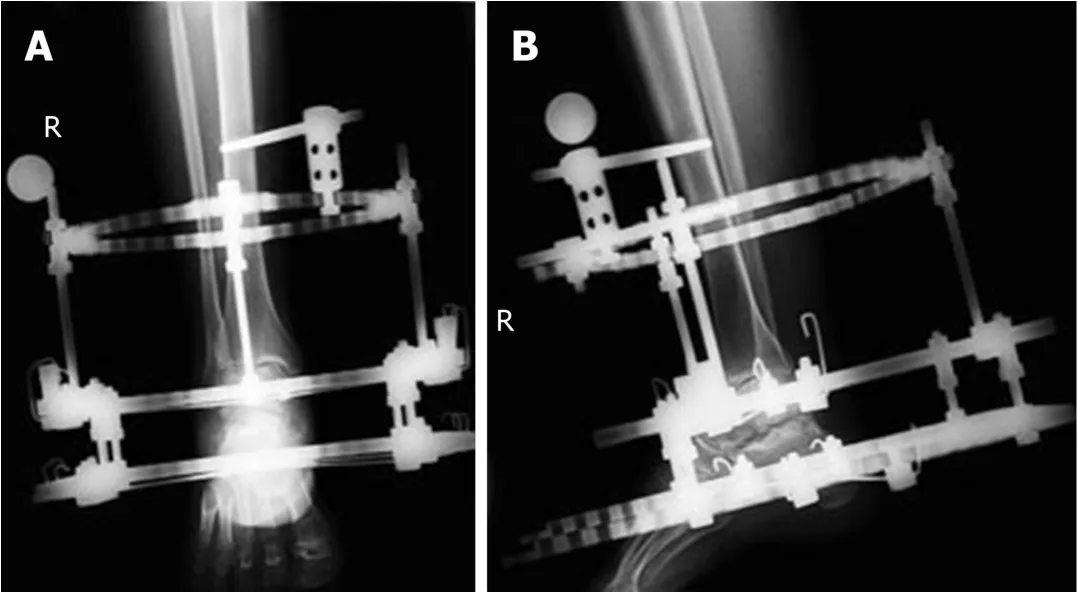
Figure 10 One-month post-operative standing X-rays of the right sub-talar joint distraction, demonstrating widening of sub-talar joint space.
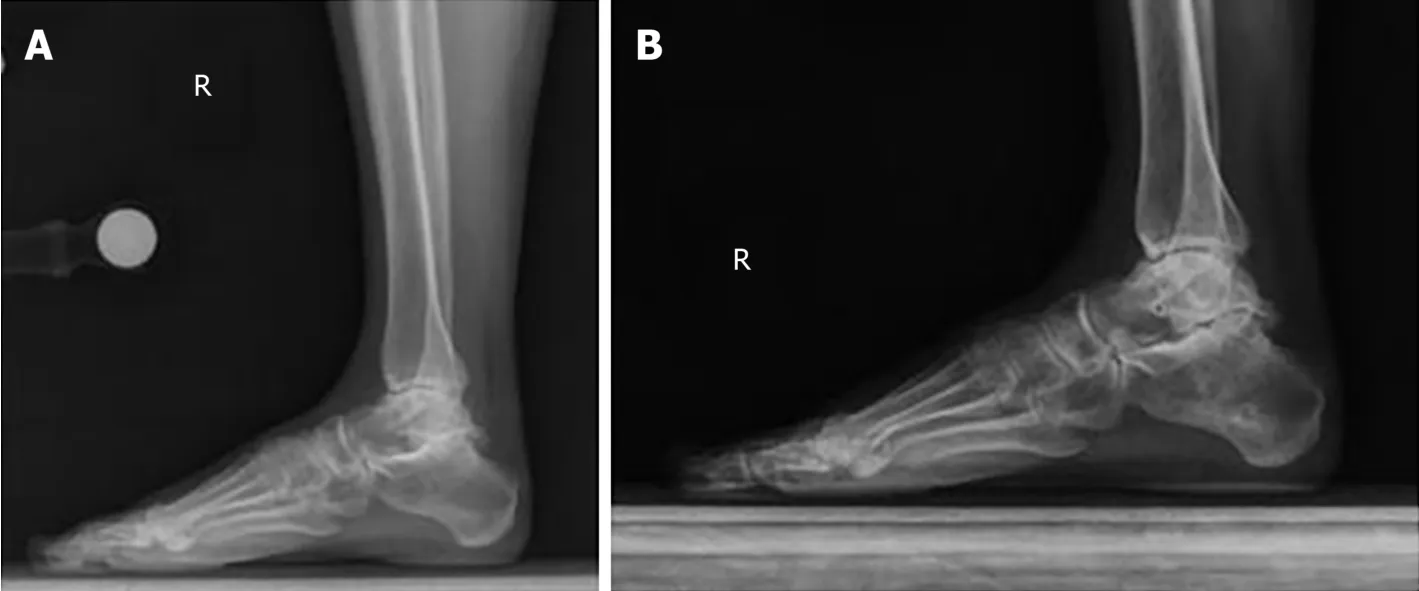
Figure 11 Comparison of pre and one-year post-operative standing X-rays of the right sub-talar joint.

Figure 12 Pre-operative X-rays of the first metatarsophalangeal joint demonstrating hallux rigidus of the first metatarsophalangeal.
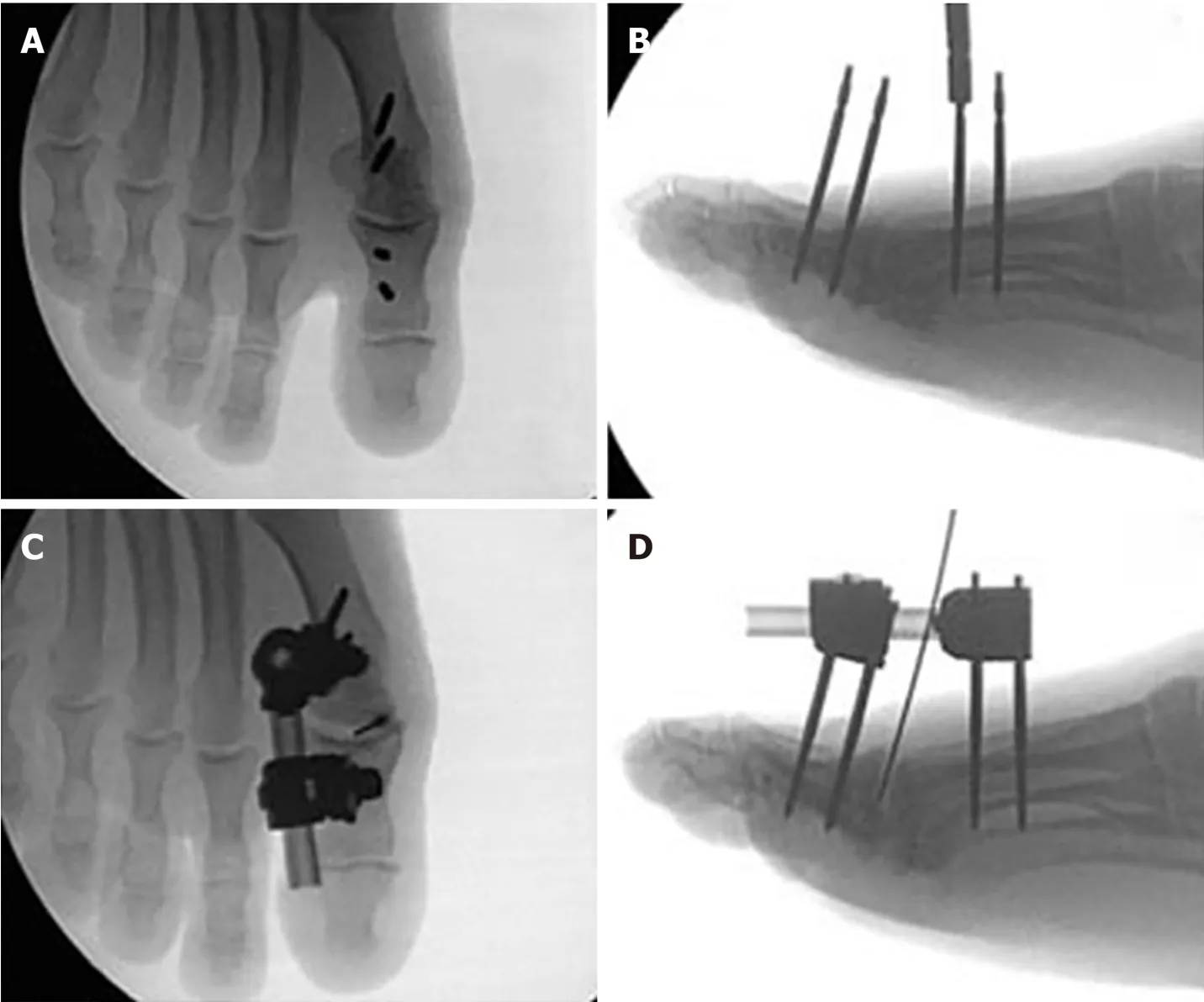
Figure 13 Intra-operative fluoroscopy of the right first metatarsophalangeal joint before and after application of external fixator.
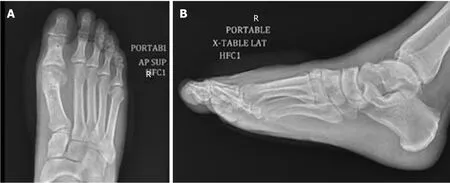
Figure 14 Three-month post-operative X-rays of the first metatarsophalangeal joint demonstrating improved metatarsophalangeal joint space.
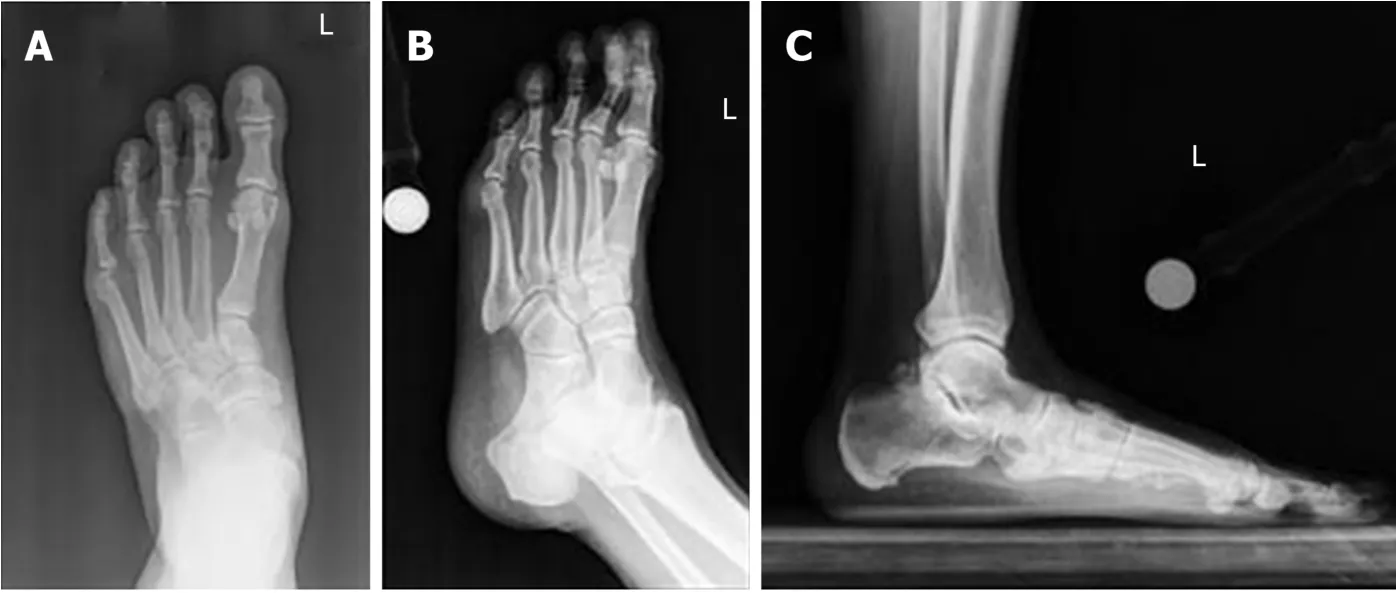
Figure 15 Pre-operative standing X-rays of the left second tarsometatarsal joint, demonstrating joint space narrowing and post-traumatic osteoarthritis in addition to flat foot deformity.
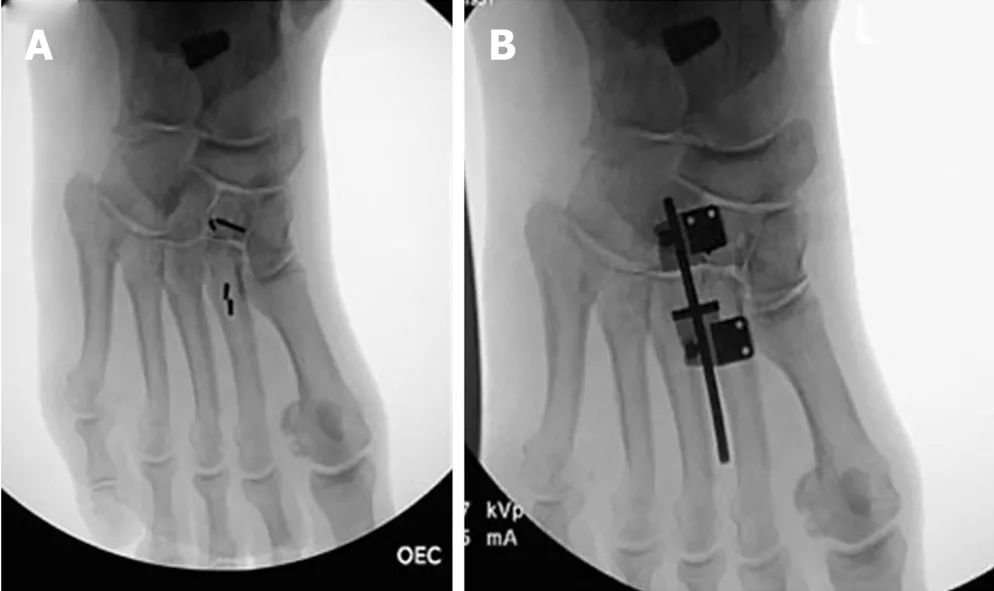
Figure 16 Intra-operative fluoroscopy of the left second tarsometatarsal joints demonstrating insertion of arthroeresis screw into the sub-talar joint to treat flat-foot deformity, in addition to application of external fixator.
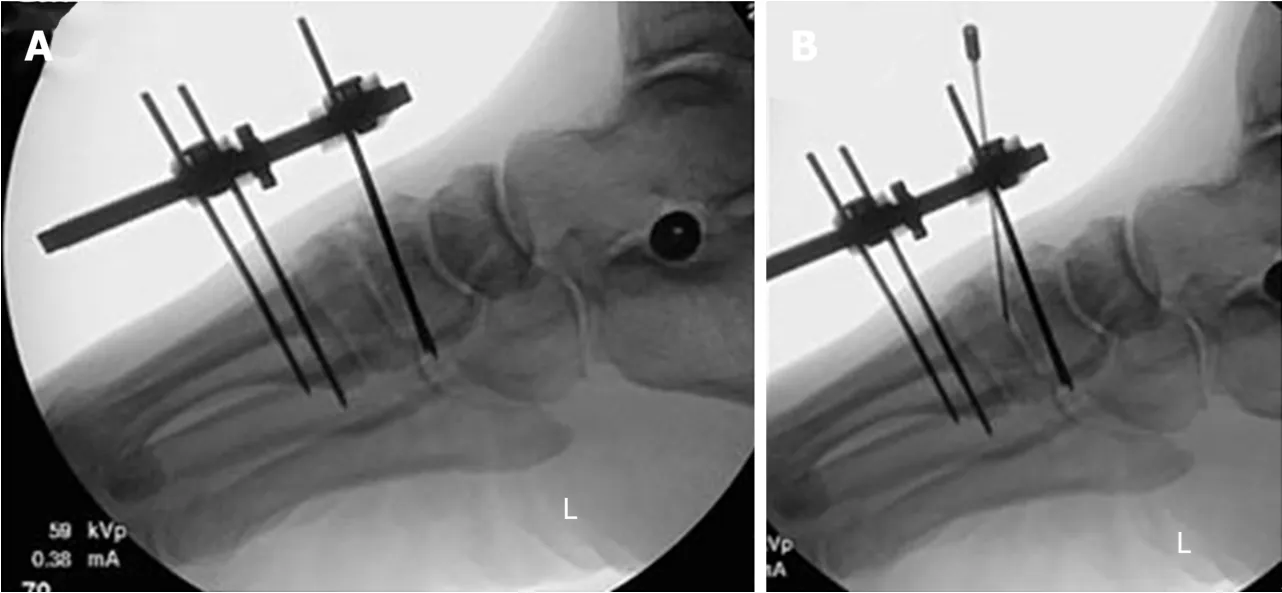
Figure 17 Intra-operative fluoroscopy of the left second tarsometatarsal joints joint demonstrating injection of bone marrow aspirate concentrate and application of external fixator.

Figure 18 Three-months post-operative X-rays of the left second tarsometatarsal joint, demonstrating improved tarsometatarsal joint space and articular cartilage.
 World Journal of Orthopedics2020年3期
World Journal of Orthopedics2020年3期
- World Journal of Orthopedics的其它文章
- Atraumatic groin pain secondary to an aneurysmal bone cyst: A case report and literature review
- Systematic review of the etiology behind patellar clunk syndrome
- Analysis of electrocautery smoke released from the tissues frequently cut in orthopedic surgeries
- Observational study of a new modular femoral revision system
- Lumbar interspinous pressure pain threshold values for healthy young men and women and the effect of prolonged fully flexed lumbar sitting posture: An observational study
