Cutaneous Metastasis of Uterine Cervical Carcinoma with a Cellulitis-Like Presentation
Qing Cai,Qiong Wu,Xiu-Lian Xu?,Wei-Da Liu
?
1Department of Mycology,Shanghai Dermatology Hospital,Shanghai 200050,China,2Department of Dermatology,Renji Hospital,School of Medicine,Shanghai JiaoTong University,Shanghai 200127,China,3Department of Pathology,4Department of Mycology,Hospital for Skin Diseases(Institute of Dermatology),Chinese Academy of Medical Sciences and Peking Union Medical College,Nanjing,Jiangsu 210042,China.
Introduction
The reported incidence of cutaneous metastasis from internal carcinoma ranges from 0.7%to 10%,with wide variability across different studies.Although cervical carcinoma is a very common malignant tumor in women,the frequency of cutaneous metastasis from cervical carcinoma is less than 2%.1Usually,metastasis occurs at a site adjacent to the primary carcinoma,and the most common clinical presentation of the metastasis is a nodule.Cervical carcinomas almost always metastasize to the abdomen wall,vulva,or anterior chest wall.To the best of our knowledge,reports of a facial cellulitis-like metastasis of cervical carcinoma are relatively rare in the published literature.Herein,we report the case of a Chinese woman,who had a two years history of cervical carcinoma and a developed facial metastasis presenting as a cellulitis-like lesion.
Case report
A 45-year-old woman was referred to Hospital for Skin Diseases(Institute of Dermatology),Chinese Academy of Medical Sciences and Peking Union Medical College with the complaint of facial infiltrative erythema and swelling for three months.Two years ago,the patient had been diagnosed with cervical squamous carcinoma and received a radical hysterectomy after undergoing cervical laser conization.She had been followed up in a cancer hospital for the ensuing two years without recurrence.One year before her visit to the Hospital for Skin Diseases,she had a denture fixed on her upper anterior teeth.Three months ago,the patient felt uncomfortable and swollen around the upper anterior teeth and the upper lip;upon inspection,no abnormal signs were found in the oral cavity.She received an incision and drainage from a local stomatology department.However,her symptoms were not relieved,and she noticed progressive erythema and swelling on the nose and the upper lip. She had been treated with azithromycin(0.25g once per day)and ornidazole(0.5g twice per day) for nearly one month without any improvement.One month ago,she experienced cough,expectoration,and a fever of less than 38°C.The patient had no history of facial trauma and hypertension,diabetes,or liver diseases.

Figure 1.The facial lesion of the patient.Diffuse erythema,swelling,and telangiectasia on the central face and swelling of the upper lip.
A physical examination showed diffuse erythema,with swelling and telangiectasia on her central face,and marked swelling of the upper lip,with tenderness(Fig.1).No lesions were found in the oral cavity,and no superficial lymph nodes were found.A computerized tomography scan revealed a nodule(9.0cm×8.0cm in size)as well as inflammation of the lingual segment in the left lung and a bilateral pulmonary pleural effusion.Laboratory investigations revealed a C-reactive protein(CRP)of 104mm/h(normal range: 0-20mm/h),carcinoembryonic antigen(CEA)of 4.71μg/L(normal range:0-10μg/L),cytokeratin 19 fragments(CYFRA21-1)of 13.05μg/L(normal range: 0-3.3μg/L), neuron-specific enolase (NSE) of 3.98μg/L(normal range:0-16.3μg/L),and carbohydrate Antigen 125 (CA-125) of 164.6U/ml (normal range:0-30.2U/ml).
The histopathology of the right cheek revealed lobules of atypical epithelial tumor cells aggregated in the dermis without connection to the overlying epidermis(Fig.2A).The lesion of the upper lip mucosa displayed dark blue tumor cell aggregating with atypical nuclei located in the subcutaneous tissue as well as in the vascular lumens and adipose tissues (Fig. 2B). Immunohistochemically, the atypical cells were positive for anti-cytokeratin antibody(CK)and negative for CEA(Fig.2C and 2D).
The lack of connection to the epidermis ruled out the primary invasive squamous cell carcinoma, and the growth pattern ruled out adnexal carcinoma.
On the basis of the intravascular infiltrate and the patient’s confirmed history of cervical carcinoma, a cutaneous metastasis from the cervical carcinoma was diagnosed.The histological features of the pulmonary nodule were consistent with the diagnosis of metastatic squamous cell carcinoma.The patient’s condition was categorized as stage IVB based on the presence of a distant metastasis,in accordance with the FIGO staging system.Thereafter,the patient underwent palliative chemotherapy with docetaxel.Six months later,the cutaneous lesions had disappeared,and the lung nodule had regressed.The patient has since been lost to follow-up.
Discussion
The incidence of cutaneous metastasis for internal carcinomas is under 10%,and skin metastasis from cervical carcinoma is relatively rare.1-2Among studies published in English,just over 50 cases of cervical carcinoma with a cutaneous metastasis have been reported by now.3-6
Usually,regions of cutaneous metastasis are near the primary tumor.Facial metastasis typically follows from oral squamous cell carcinoma,a hypernephroid tumor,lung cancer,or breast cancer,and it was very rarely in cervical carcinoma,only three cases have been reported on PubMed till now.3,5,7The mechanism of a facial metastasis may be associated with lymphatic and hematogenous pathways.
The most frequent clinical type of all cutaneous metastases is the nodule,1,4,7followed by plaque,inflammatory metastasis,carcinoma en cuirasse,and alopecia neoplastica.An inflammatory metastasis can also be called carcinoma erysipeloides, which is mostly observed in breast cancer metastasis,although it is occasionally also found for other malignant tumors.7Including the present case,there have been two reported cases of inflammatory telangiectatic pattern of cutaneous metastasis from cervical carcinoma.3The case reported by Yang et al.3from Taiwan and our case were both characterized by inflammatory telangiectatic erythema,swelling,and tenderness on the central face.Their case was treated as cellulitis without improvement.Our case was also treated with antibiotics for nearly one month in consideration of her oral surgery history.
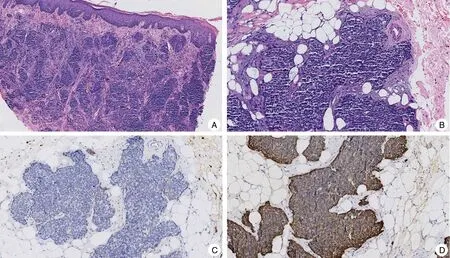
Figure 2.Histopathological results of the facial lesion.(A)Lobules of atypical epithelial tumor cells aggregated within the dermis without connection with the epidermis(H&E,×40).(B)Sheets of atypical cells located in the vascular lumens and adipose tissue(H&E,×100).(C)Atypical epithelial tumor cells were negative for CEA(Immunohistochemical staining,×100).(D)Atypical epithelial tumor cells were positive for anti-cytokeratin antibody(Immunohistochemical staining,×100).
The histopathology patterns of cervical carcinoma include adenocarcinoma, squamous carcinoma, and undifferentiated carcinoma.The most frequent type of cutaneous metastasis reported is still controversial.2,4Agrawal et al.4reviewed 47 cases of cutaneous metastasis from cervical carcinoma that occurred between 1993 and 2008.Among these cases,squamous cell carcinoma was the most common histopathology pattern(30/47),compared with only five cases of adenocarcinoma.Histological and immunohistochemical analyses of the facial lesion in our case confirmed the presence of metastatic squamous cell carcinoma,which was more likely because of the hematogenous spread. Meanwhile, a nodule on the patient’s lung was also confirmed to be metastatic carcinoma. Based on these findings, our case was definitively diagnosed and prescribed antitumor therapy,which was effective.The average time between an initial diagnosis and a cutaneous metastasis of cervical carcinoma is 20.7 months.4Metastasis to the skin always indicates a poor prognosis,8and the average survival period is only 8.5 months.4Thus, making an early diagnosis and promptly commencing appropriate treatment is helpful for prolonging the lives of patients with skin metastasis.
Here, we present an unusual case of cutaneous metastasis from cervical carcinoma. First, the clinical manifestation of this case inflammatory facial metastasis is unusual in the English literature. Second, such an inflammatory telangiectatic erythema is easily misdiagnosed because it must be differentiated from benign dermatitis and infectious diseases such as cellulitis and zygomycosis. Last, cutaneous metastasis is always a predictor of poor prognosis,so a prompt diagnosis and treatment are important for prolonging the life of a patient with this condition.
- 國(guó)際皮膚性病學(xué)雜志的其它文章
- Instructions for Authors
- Deep Penetrating Nevus
- Apocrine Sweat Gland Adenocarcinoma in the Left Retroauricular Area:A Rare Case Report
- Actinic Granuloma:A Case Report
- Squamous Cell Carcinoma Secondary to Mutilating Palmoplantar Keratoderma
- Toxic Shock Syndrome Due to Streptococcus pyogenes Presenting with Purpura Fulminans in an Older Adult