Effectiveness of inpatient alcohol detoxification and psychotherapeutic support program:a prospective self-controlled study at a tertiary hospital in Nepal
Suraj Shakya,Jug Maya Chaudhary,Pramesh Man Pradhan,Saroj Prasad Ojha,Mita Rana
Department of Psychiatry &Mental Health,Institute of Medicine,Tribhuvan University,Kathmandu,Nepal
Abstract
Key words:alcohol treatment;inpatient detoxification;motivation;psychotherapy;psychosocial;relapse;self-controlled study
INTRODUCTION
Alcohol use disorder,which includes alcohol dependence and harmful use,is one of widespread mental health and psychosocial problem.In Nepal,12-month prevalence estimates of alcohol use disorder are 3.4% in general (Dahal et al.,2019),3.1% among males and 0.6% among females;while alcohol attributable years of life lost is 2 years (WHO,2018).
A recent study on treatment gap in a district of Nepal reports that only 5.1% of people with alcohol use disorder sought treatment in past 12 months (Luitel et al.,2017).The barriers to treatment were mostly reported as affordability issues,being unsure where to go to get mental health care,stigma of being seen as “crazy,” perceived risk in applying for jobs and concern of being perceived as weak.Similarly,another study on use of alcohol treatment facilities in Kathmandu reports that traditionally alcohol non-using castes and people with higher socioeconomic status were over-represented in treatment centers (Neupane and Bramness,2014).
Two major treatment modalities are gaining popularity in helping a person with alcohol use disorder in Nepal.One modality is residential rehabilitation centers which run three or more months of non-pharmacological management program.Most of these centers incorporate 12-step programs,besides infrequent visits of physicians,psychiatrists,psychologists and counselors.The other modality is a pharmacological detoxification program,run by hospitals and clinics on inpatient or outpatient basis.
Inpatient settings offer constant medical care and supervision by professional staff,which is an advantage over outpatient or other modalities of care (Hayashida,1998) for easy availability of treatment for serious complications.In addition,such settings prevent patient access to alcohol and offer separation from the substance-using environment.Similarly,psychotherapeutic interventions are of great relevance for treatment outcome,and hence integration of psychotherapeutic “motivational” elements into detoxification program is suggested by various guidelines (Soyka and Horak,2004).
One aspect of how psychotherapeutic intervention (e.g.,motivational interview) works is that it helps in person's change talk,motivation and self-efficacy,enhancing overall treatment outcome.For instance,non judgemental atmosphere in session may provide unique opportunity for the clients to reflect on their reasons for change in behavior,and they can verbalize the discrepancy between their current alcohol use and longer-term life goals (Feldstein Ewing et al.,2011a).Evidences from translational researches provide hints on how psychotherapeutic intervention help in inhibiting activation in brain regions that respond to the salience of alcohol cues (Feldstein Ewing et al.,2011b).Within the therapy,a skillful therapist behavior and client change talk is mediated by the relational reasoning network,which is function of certain prefrontal cortical structure (e.g.,rostrolateral &dorsolateral prefrontal cortex),the emotional learning/memory network (e.g.,posterior cingulate cortex &precuneus areas) and the incentive reward network (Feldstein Ewing et al.,2011a).Feldstein Ewing et al.(2011b) further elaborate on how such in-session processes continue outside the therapy session and help in maintaining treatment gains.In addition,these sessions help in utilizing social bonds (social control theory),alternative rewards other than alcohol (behavior economics/choice theory) and social reinforcement/learning by observing others (social learning theory) (Moos,2007a).
In context of low and middle income countries like Nepal,one challenge is awareness on availability of treatment modalities for alcohol use disorder among general population.In addition,effectiveness of such treatment modalities for alcohol use disorder in Nepalese setting is not publicized.In this context,we report data of an inpatient alcohol detoxification and psychotherapeutic support program run in a tertiary level hospital.This paper is a part of a dissertation project by one of the author (JMC),when she was trained as a clinical psychologist at a teaching hospital.The project focused on studying motivational status of patients being treated for alcohol use disorder;details on these aspects are reported elsewhere.The aim of the current paper is to evaluate effectiveness of such treatment as usual (detoxification with concomitant psychotherapeutic approach) in terms of improvement in motivation to stay abstinent and status of drinking in 3-month follow-up.
SUBJECTS AND METHODS
Study design
This was a prospective self-controlled study design.It was conducted at inpatient unit at Department of Psychiatry and Mental Health at Tribhuvan University Teaching Hospital in Kathmandu,Nepal.This is a tertiary level teaching hospital,with integrated psychiatric and clinical psychological services.Ethical approval was taken from Institutional Review Board,Institute of Medicine,Tribhuvan University on December 29,2017 (Additional file 1).This trial was registered in Clinical-Trials.gov (NCT03988478).Informed consent of the study procedure was obtained from all participants (Additional file 2).
Non probability purposive sampling method was used.Data were collected for nine months targeting all the patients aged 18 years above,meeting criteria of alcohol dependence syndrome according to International Classification of Diseases 10threvision (WHO,1992).Data were collected once patient or one close relative attending patient at the inpatient unit consented for it.Patients with other psychiatric comorbidity (e.g.,schizophrenia,mood disorders),medical co-morbidity and multiple substance use in past 6 months were excluded.
Interventions
Department of psychiatry and mental health at Tribhuvan University Teaching Hospital has been running inpatient detoxification program since its establishment,but separate inpatient unit for substance related disorders started in 2000 (Sharma,2013).Since then detoxification as well as psychotherapeutic interventions has been integrated by team of consultant psychiatrists,clinical psychologists and residents (MD psychiatry and MPhil Clinical psychology).This has been summarized in a guideline “Alcohol Detoxification Protocol,” which was drafted at the department (Sharma et al.,2012).The objectives of inpatient detoxification and psychotherapeutic intervention are:
· To ensure that a person can cease alcohol use without experiencing a potentially hazardous withdrawal state;
· Help a person stay away from hazardous effect of excessive alcohol consumption;
· Diagnose and treat co-morbid medical and psychiatric conditions;
· Help through harm reduction procedures and initiate referral for ongoing treatment,relapse prevention and rehabilitation.
Medical and pharmacological managements
Immediate medical support of patients with complicated withdrawal is the first priority.Medical team also looks after management of fluid,electrolyte and supplementation of thiamine and other multivitamins.Once immediate management is done,short-term management for inpatient care is the main component of detoxification program.The management itself differs for uncomplicated or complicated cases.Pharmacological management ranges from use of chlordiazepoxide or lorazepam or diazepam.Injectable haloperidol is also used,if needed,for addressing aggression or sleep.The doses are titrated according to the severity of withdrawal features and they are tapered gradually in 10 to 14 days.Once short-term management is done,long-term therapy starts with the main aim of relapse prevention.Disulfiram is an option to be used as deterent.For anticraving therapy Naltrexone is also an option decided collaborately with the patients and their family members.The average hospital stay is two weeks,and usually less than a month.
Psychotherapeutic and psychosocial managementsThis is an integrated approach which involves consultants and residents in clinical psychology or psychiatriy together with nursing staff and all the staff of the detoxification team.Psychosocial intervention aims to enhance and maintain motivation or readiness to change and overall psychological growth and development.Ongoing assessment (using motivation level questionnaire,different rating scales and psychological testing as required) as well as assessment of individual strength,interpersonal and environmental issues are done.Interventions can be grouped into three levels as below:
A) Individual level:At individual level the following steps are considered:
· Psychosocial assessment
· Motivational interviewing for 1 to 3 sessions
· Optional-supportive psychotherapy,cognitive behavior therapy or other forms of psychotherapy (involve patients before deciding any therapy)
· Awareness program regarding self-help group,anti-abuse/anti-craving agents,drinking habits,coping skills and sleep hygiene
B) Group level:It includes:
· Group session once a week during the stay at hospital,with other clients with similar problem of alcohol and drug
· Introduction to self-help group
· Family therapy,if indicated
C) Primary support group:It includes sessions with primary support group like guardians,family members,close friends or legal guardians of client.They are chief sources of information;hence they have a key role in assessment.Minimum of two sessions with primary support group is targeted,focusing on psychoeducation and supportive psychotherapy as per the need.
Long-term management and relapse prevention
For long-term management and relapse prevention,patients are encouraged to join self-help group meetings (like AA).They can continue supportive psychotherapy or other sorts of psychotherapy.
Besides this medical and psychosocial management,ongoing assessment,diagnosis and treatment of co-morbid medical and psychiatric condition are also done accordingly.
Outcome measures
For the purpose of study,effectiveness of intervention was measured by two primary outcome measures;one through measure in readiness to change or motivation and the other with 3-month follow-up for status of abstinence and relapse.For readiness for change,19-itemed version of The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) (Miller and Tonigan,1996) was used.The authors of SOCRATES reported three relatively unrelated factors that were stable across rotations:Recognition,Ambivalence,and Taking Steps,with cronbach alphas of 0.91,0.90 and 0.60 respectively.Nepali translated version of SOCRATES (Adhikari,2017),which has been already used in previous study in the same department,has been used.
Regarding the maintenance of abstinence and relapse,several definitions exists on what is relapse (Potgieter et al.,1999).For current study,three criteria were chosen:if participants maintain complete abstinence,they were categorized as maintaining well;if they had one or two drinks in a setting,for not more than two or three days,they were categorized as occasionally drinking;if they drank more than occasionally,they were categorized in relapse status.
Other measures
The original research used objective rating scales for severity of alcohol dependence and withdrawal symptoms during time of admission.In-depth interviews were also done with patients during and after discharge.These data will be reported elsewhere.A sociodemographic proforma with sociodemographic details and information regarding alcohol use was also used.
Procedure
Author JMC initiated the project as a part of her dissertation research project.Initially,all the residents in Psychiatry (n= 11) and Clinical Psychology (n= 5) were re-oriented on treatment as usual for inpatient detoxification and psychotherapeutic support.They were under constant supervision of the faculties.Primary data collection was done by JMC.Eligible participants were approached for data collection after they were oriented to time,place or person,and when they were able to communicate.During baseline assessment,interview on sociodemographic detail was followed with rating on withdrawal and severity of alcohol dependence together with ratings on SOCRATES.Each patient underwent the procedure as per the Usual Treatment Protocol.Post test data were gathered from patients just prior to discharge (usually in 2 weeks) and 2 weeks after discharge using SOCRATES.Totally 63 patients were followed up through phone contact after 3 months of discharge.Patients and their family members were enquired on status of abstinence maintenance.
Data analysis
Data were initially entered in MS Excel.Final analysis was done in IBM SPSS Statistics for Windows,version 20 (IBM,Armonk,NY,USA).Descriptive statistics were calculated.Scores on SOCRATES were skewed and hence medians were reported.Friedman test,as a non-parametric test,was used to compare baseline and follow-up assessments.When these changes were statistically significant,apost hocanalysis was done using Wilcoxon signed-rank test,with Bonferroni adjustment.
RESULTS
Participant characteristics
Of 135 participants screened for alcohol use disorder between January and September 2018,only 109 (age 42.5 ± 9.3 years;male = 90.8%) were enrolled for the study.Totally 26 participants were excluded as they were having psychiatric and major medical co-morbidity or using multiple substance use.Patient characteristics are summarized in Table 1.Most of them were married (91.1%) with age range between 25 till 67.Most studied till tenth (28.3%) or twelfth standard (25.4%) and were from agriculture (31.7%) or service/sales profession (28.6%).Similarly,out of 109 enrolled for study,only 63 could be followed till 3 months.Most of them were residing outside Kathmandu Valley and they could not be contacted even through phone.Sociodemographic details of these 63 participants have also been summarized in Table 1.
Outcome
Primary outcome measure was pre and post measure reflected in SOCRATES.The baseline scores and follow-up scores in SOCRATES are summarized in Table 2.
Recognition
There was no significant change in scores for recognition of problem,as reflected in median scores of each successive follow-ups starting from the baseline.

Table 1:Baseline sociodemographic characteristics of patients

Table 2:SOCRATES measures at baseline and follow-up
Ambivalence
There was a decline in scores in ambivalence at successive follow-ups than the baseline and this was statistically significant,χ2= 9.7,P= 0.008.Post hocanalysis with Wilcoxon signed-rank tests was conducted with a Bonferroni correction,with significance level set at 0.017.Median scores were 16,13 and 12 respectively.There were significant differences between the baseline and other two post-tests,i.e.,prior to discharge and 2 weeks after discharge (Z= -5.0,P= 0.000 andZ= -3.0,P= 0.003).
Taking steps
There was statistically significant improvement in scores for taking steps,χ2= 13.1,P= 0.001.Post hocanalysis with Wilcoxon signed-rank tests was conducted with a Bonferroni correction applied,with significance level set at 0.017.Median scores were 37,39 and 40 respectively.There were significant differences between prior to discharge and 2 weeks after discharge (Z= -4.0,P= 0.000 andZ= -2.1,P= 0.036).
Three-month status of abstinence
After 3 months,63 participants were contacted through phone.Information was taken from participants and their family members regarding alcohol intake (Figure 1).Among them,73% of the participants were in complete abstinence,and 6.3% had one to three drinks on one or two occasions.Similarly,20.6% of the participants relapsed,meaning that they either took more than four drinks or started drinking regularly.
DISCUSSION
Alcohol use disorder is prevalent,and researches show that treatment gap exists (Rathod et al.,2016;Luitel et al.,2017).National Mental Health Policy (MoHP,1997) reflects commitment for access to treatment for all.However,it is necessary to prove that these available treatments are effective.The present study sought to evaluate an inpatient detox and psychotherapeutic support program at Tribhuvan University Teaching Hospital in Kathmandu.The findings hint the fact that the short-term inpatient detoxification and psychotherapeutic support program has significant impact on enhancing readiness for change,and maintaining alcohol free life style.
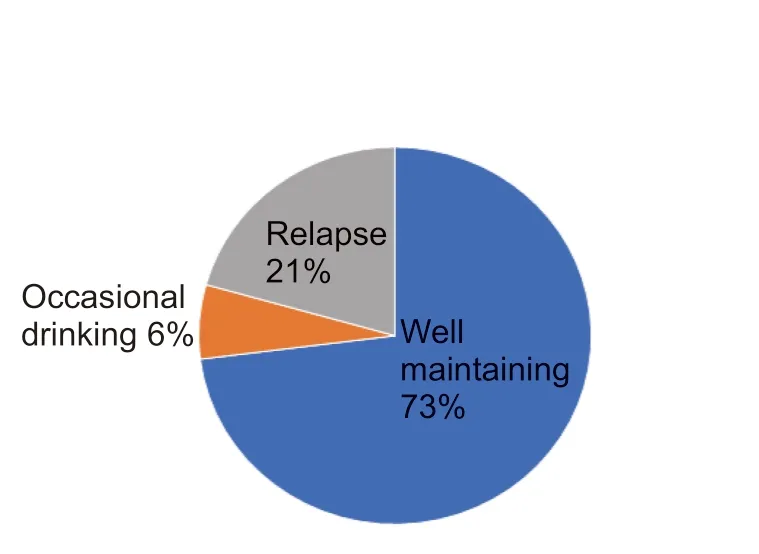
Figure 1:Status of abstinence in 3-month follow-up.
The baseline and follow-up results indicate that there is significant improvement in ambivalence towards drinking as problem and taking steps in either reducing alcohol or staying alcohol free at least for 3 months.These aspects of motivation are suggested by Miller and Tonigan (1996) and has highlighted on the role of motivational variable on treatment entry,compliance,and outcome of treatment (Miller,1985).This is also related to self-efficacy and scores on “taking steps” is associated with the expectancy to cope successfully with high-risk situations (Demmel et al.,2004).Regarding the “recognition” variable on SOCRATES,there has not been significant improvement,despite improvement in other two aspects of motivation.One hypothesis to explain this insignificant change in recognition factor is that most of the patients are brought to inpatient detoxification after withdrawal features and life threatening complications;and hence recognition or awareness of the problem caused by heavy drinking (Demmel et al.,2004),is already present during baseline assessment,which implies less change afterwards.Another possibility is about factor nature of SOCRATES in given population.Several researchers have proposed two-factor model,merging recognition factor and ambivalence factor (Maisto et al.,2003;Bertholet et al.,2009) according to their field studies.Hence,even in Nepalese population,the three-factor structure originally proposed by Miller and Tonigan (1996) needs to be evaluated.
Regarding relapse and abstinence maintenance,in current study 73% were maintaining well with complete abstinence after the intervention.This result is comparable or even better than other reports (Monahan and Finney,1996;Bradizza et al.,2006).As cited in Bradizza et al.(2006),“at 3 months post-treatment,40-60% of individuals in treatment for alcohol problems relapse to a first drink…” There are several predictors of relapse or remission in alcohol treatment.A previous study shows that in comparison to individuals who obtained help,those who did not were less likely to achieve remission and subsequently were more likely to relapse (Moos and Moos,2007b).
Limitation of this research includes lack of suitable control,and methodological concerns in single group pre- and post-test research designs (Marsden and Torgerson,2012).Similarly,several predictor variables for motivation and relapse,for instance,nature of alcohol habit,amount of alcohol intake,or types of complication after drinking and other psychosocial variables are not analyzed in this paper.Future work needs to incorporate these variables in the design itself.Generally,abstinence is generally achieved during the early days and weeks of treatment,but the majority of patients return to heavy drinking within 3 to 6 months after treatment begins (Lowman et al.,1996;Bradizza et al.,2006).Hence longitudinal designs even extending 6 months to few years are necessary.Similarly,the professionals and clinicians in addiction treatment would benefit from the analysis of specific components of treatment,that is more efficient and the overall underlying mechanism of change of the treatment modality,whether it be underlying biological mechanism,or psychological or social etiology underlying the modality.Besides these limitations and future research implications,this study in general,reiterates the message that people with alcohol use disorder need help and current treatment modalities facilitate healthy lifestyle.Scaling up such treatment modalities and making it more cost effective is necessary.
Additional files
Additional file 1:Institutional Review Board Approval.
Additional file 2:Informed Consent Form.
Acknowledgement
We would like to acknowledge all the faculties and residents at Department of Psychiatry and Mental Health,Maharajgunj Medical Campus,Tribhuvan University Teaching Hospital for supporting this project.
Author contributions
Concept and design of study protocol:SS,JMC,SPO and MR;data collection and analysis,drafting of the manuscript:SS and JMC;editing of the manuscript:SS,JMC,PMP,SPO and MR.All authors approved the final manuscript for publication.
Conflicts of interest
The authors have no conflicts of interest to declare.
Financial support
None.
Institutional review board statement
Ethical approval was taken from Institutional Review Board,Institute of Medicine,Tribhuvan University on December 29,2017.This study was performed according to theDeclaration of Helsinki,and informed consent of the study procedure was obtained from all participants.
Declaration of participant consent
The authors certify that they have obtained all appropriate participant consent forms.In the forms,the participants have given their consent for their images and other clinical information to be reported in the journal.The participants understand that their names and initials will not be published and due efforts will be made to conceal their identity.
Reporting statement
This study followed the Recommendations for the Conduct,Reporting,Editing and Publication of Scholarly Work in Medical Journals developed by the International Committee of Medical Journal Editors.
Biostatistics statement
The statistical analysis of this study was performed by the first author SS and approved by the other authors.
Copyright license agreement
The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement
Individual participant data that underlie the results reported in this article,after deidentification (text,and tables),will be available upon request.Data will be available immediately following publication,no end date for anyone who wishes to access the data.In order to gain access,data requestors will need to sign a data access agreement.Proposals should be directed to surajshakya@iom.edu.np.
Plagiarism check
Checked twice by iThenticate.
Peer review
Externally peer reviewed.
Open access statement
This is an open access journal,and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License,which allows others to remix,tweak,and build upon the work non-commercially,as long as appropriate credit is given and the new creations are licensed under the identical terms.
 Asia Pacific Journal of Clinical Trials:Nervous System Diseases2019年3期
Asia Pacific Journal of Clinical Trials:Nervous System Diseases2019年3期
- Asia Pacific Journal of Clinical Trials:Nervous System Diseases的其它文章
- Bacteriological profile of endotracheal tube aspirates in head injury patients admitted in Neurosurgical Intensive Care Unit:a cross-sectional study from a tertiary care hospital of Central Nepal
- Mindfulness-based cognitive therapy for university students with depression,anxiety,and stress symptoms:a randomized controlled trial
- Treatment with a halved dose of antipsychotics in patients with schizophrenia who relapse while receiving high-dose antipsychotic therapy
