Memory response to manual acupuncture in chronic insomniacs: evidence from event-related potentials
Zhao Fei-yi (趙非一), Zhang Zhe-yuan (張浙元), Xia Xiao-jie (夏小芥), Hong Yu-Fang (洪鈺芳), Zhao Ying-xia (趙英俠),Yan Hai-xia (燕海霞), Xu Hong (許紅)
1 Shanghai Municipal Hospital of TCM Affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai 200071, China
2 Haiyan People's Hospital, Zhejiang 314300, China
3 Department of Education, East China Normal University, Shanghai 200062, China
4 School of Basic Medical Sciences, Shanghai University of Traditional Chinese Medicine, Shanghai 201203, China
Abstract Objective: To investigate the effectiveness and safety of manual acupuncture for memory loss and sleep quality in chronic insomniacs.
Keywords: Acupuncture Therapy; Manual Acupuncture; Insomnia; Memory; Evoked Potentials
As a significant and growing concern for public health,insomnia is one of the most common health complaints worldwide[1]. Previous epidemiological surveys showed that the prevalence of insomnia in adults was approximately 38.2% in China, which was higher than that in many Western countries[2]. Among all types of insomnia, chronic insomnia (CI) accounted for 15%[3].According to the 3rd edition of International Classification of Sleep Disorders (ICSD-3), CI is defined as persistent and prolonged nature of sleep disorders lasting for more than three months, featured by an inability to fall asleep at bedtime or maintain sleep for a sufficient amount of time during regular sleeping hours,early morning waking, or poor quality of sleep,accompanied by significant daytime consequences or even impairments, and it is not attributed to another sleep disorder, a mental and psychopathic illness, or as the direct effect of a substance[4]. Without effective intervention, CI can be a high risk of hypertension[5],obesity[6], stroke[7], depression and anxiety[8], and has been proved to result in impairments of immunity and cognitive function[9].
As one of the typical manifestations of cognitive impairments, memory impairment is very common among patients with CI[10]. As sleep and cognition are two basic physiological functions of the human brain,their relationship has always been a research hotspot in many medical fields such as psychology and neuroscience. Although previous studies mainly focused on the impacts of insomnia on attention[11],implementation capacity[12], and motor learning[13],more attention has now been paid to the impacts of insomnia on memory. CI has been proved not only to lead to degeneration in procedural memory[14],declarative memory[15], working memory[16], and prospective memory[17], but also lead to disorders in integration of memory[18], and memory consolidation in both explicit memory[19]and emotional memory[20].Among them, emotional memory is not only an important part of memory, but also has priority in cognitive processing in the brain, which ensures that individuals can accurately respond to various emotional stimulations, and reflects the adaptation of the organism to the environment in evolution[21].Furthermore, the processing of emotional memory is closely related to sleep[22].
Sedative and hypnotics including benzodiazepine receptor agonists are currently used for various types of insomnia with satisfactory short-term efficacy[23].However, long-term use of these medications may cause some residual symptoms, particularly the cognitive impairment[24], which prompts patients to seek treatment from complementary and alternative medicine (CAM). Acupuncture, a typical branch of CAM,has been widely used in Asia and increasingly used in Western countries, and has showed satisfactory effect in treatment of insomnia[25]. However, insufficient high-quality reports could provide little evidence about if manual acupuncture benefits chronic insomniacs with memory impairments such as memory loss, paramnesia or cryptomnesia. To investigate the safety and effectiveness of manual acupuncture for memory and sleep quality among chronic insomniacs and address the design defects in the relevant previous studies, this study adopted a randomized, patient-blind, and sham-controlled clinical design and more intuitive and reliable detection techniques. The report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
The diagnostic criteria were based on ICSD-3[4], the5th revision of Diagnostic and Statistical Manual ofMental Disorders (DSM-V)[26], and the 3rd edition ofChinese Classification of Mental Disorders (CCMD-3)[27]:a type of sleep disorder with main symptoms of sleeplatency or wakening after sleep onset >30 min, andpersistent difficulty initiating and maintaining sleep,frequent sleep disruptions, dreaminess, poor quality ofsleep, or waking up earlier than desired; the sleepdisorder occurred at least 3 times per week for morethan 3 months; the patient usually presented asignificant loss of memory, difficulty concentrating,fatigue, dizziness, headache, palpitation, or chesttightness due to the sleep disorder; insomnia was theprimary complaint and it was not following thepresence of another sleep disease, mental disorder, oras the direct physiological effect of a substance ormedical condition.
1.2 Inclusion criteria
Aged 18-65 years old; conformed to the above diagnostic criteria; Pittsburgh sleep quality index (PSQI)global score ≥6 points; global deterioration scale (GDS)≥ level 2 (this level indicates a very mild cognitive decline); did not take any sedative or psychoactive drugs within 2 weeks prior to the commencement of this trial; signed the informed consent, voluntarily participated in this clinical trial, and pledged to cooperate with follow-up visits.
1.3 Exclusion criteria
Aged <18 or >65 years old; those with cancer, severe hepatic or renal insufficiency, or primary diseases involving hematopoietic or endocrine system; cognitive impairments caused by neurodegenerative diseases such as Parkinson disease, Alzheimer's disease, vascular dementia, stroke, mental disorders, other chronic systemic illnesses or medical conditions; Hamilton anxiety scale ≥14 points, and/or Hamilton depression scale ≥18 points; secondary insomnia (insomnia induced by anxiety and depression disorders,obsessive-compulsive disorder, or phobia), insomnia due to occupational factors (including sleep disorders induced by shift work), jet lag syndrome, and obstructive sleep apnea-hypopnea syndrome; those participated in other clinical trials within the past 1 month; those with skin infection or tendency of bleeding.
1.4 Withdrawal and dropout criteria
Severe adverse event related to the research occurred; when the participant asked to withdraw from the trial for any reason at any time; the treatment had to be interrupted due to unforeseen reasons; when the participant received other treatment during the study or did not cooperate with the researcher; when the participant failed to return to the hospital on time.
1.5 Participants and randomization
This was a double-centered, randomized, patientblinded, parallel-group and placebo-controlled trial with a ratio of 1:1 between the treatment and control groups.Before the commencement of recruitment, the random numbers were generated by the SPSS version 21.0 statistical software, and these random numbers were separated and sealed in 60 opaque envelopes. A total of 60 patients who met the inclusion criteria were recruited by hospital-based advertisements from the outpatient clinic and the WeChat of Traditional Chinese Medicine (TCM) Sleep Research Institute of Shanghai Municipal Hospital of TCM Affiliated to Shanghai University of Traditional Chinese Medicine and Haiyan People's Hospital between May 2015 and December 2016. The patients were randomly allocated to either the treatment group or the control group through simple envelope method. Outcome assessments were conducted at baseline and post-treatment. The trial was approved by the Ethics Committees of Shanghai Municipal Hospital of TCM Affiliated to Shanghai University of Traditional Chinese Medicine and Haiyan People's Hospital. There were no significant differences in the general data between the two groups (all P>0.05),indicating the comparability (Table 1).
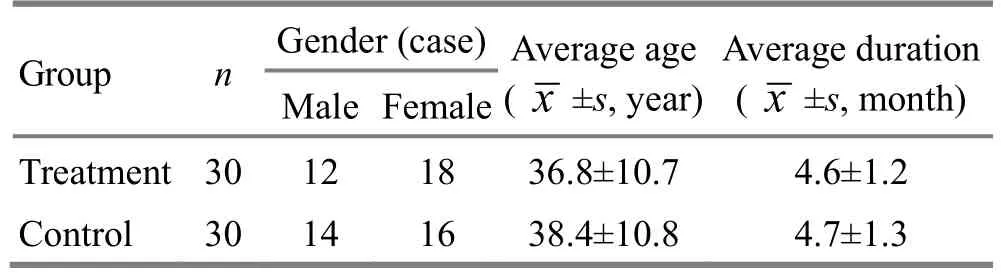
Table 1. Comparison of the general data
2 Treatment Methods
All patients were provided with the regular health education at the first visit, including a handbook of Rehabilitation and Prevention Lectures on Insomnia compiled by the TCM Sleep Research Institute. At the same time, the patients and their family members were taught how to use sleep log for a sleep record. The sleep log was required to be done every day by the patients themselves with the help and supervision of their family members, and brought to the doctor for check at each following visit.
2.1 Treatment group (manual acupuncture)
Acupoints: Sishencong (EX-HN 1), Shenting (GV 24),Baihui (GV 20), and bilateral Benshen (GB 13), Taixi(KI 3), and Shenmen (HT 7).
Method: Participants in the treatment group were in a supine position for needling. The acupoints were sterilized by 75% alcohol. Standard sterilized disposable needles (0.25 mm in diameter and 25 mm in length,stainless steel, Jiajian Medical Instrument Co., Ltd.,China) were inserted superficially into Sishencong(EX-HN 1), Baihui (GV 20), Shenting (GV 24) and Benshen (GB 13), while Taixi (KI 3) and Shenmen (HT 7)were inserted perpendicularly with needles of another specification (0.25 mm in diameter and 40 mm in length,stainless steel, Jiajian Medical Instrument Co., Ltd.,China). Needling depths were based on the feature of acupoints. Usually, needles were inserted into the skin by a depth of 10-30 mm and manipulated manually until needling sensation (qi) was achieved. The feelings of needling sensation (qi) were strengthened by the acupuncturist through twisting or lifting-thrusting the needles. After that, all of the needles were retained for 30 min before removal.
2.2 Control group (sham acupuncture)
Acupoints: The acupoints were same as for the treatment group.
Method: In light of the previous insomnia-related high-quality randomized controlled trial[28], a noninvasive, placebo acupuncture approach (Streitberger placebo acupuncture needle) was applied to the control group[29]. Streitberger needle is a type of specially designed acupuncture needle with a blunt needlepoint.When the blunt needlepoint touched the skin, it would spring back into the needle sheath.
Patients in both groups were treated once every other day and three times a week for a total of 8 weeks.Meanwhile, they were informed that these two acupuncture approaches were commonly used in clinical practice and both of them were effective, and the purpose of this trial was only to compare which acupuncture approach is better in improving both insomnia and memory impairment. Patients' other questions about the treatment efficacy during the intervention would not be answered by the acupuncturist.
2.3 Outcome measures
2.3.1 Primary outcome
Event-related potentials (ERPs): Neuropack 2 evoked action potential meter (product model: MEB-7102K,Nihon Kohden, Tokyo, Japan) with oddball paradigm was used for assessment. Participants were required to sit in the quiet laboratory with the temperature set at 25 ℃. The scalp was cleansed by 75% alcohol, and then circular electrodes with conductive paste were fixed with medical adhesive plasters. The electrodes were placed according to the international 10-20 system compiled by the International Electroencephalographic Society Guidelines for Standard Electrode Position Nomenclature: active electrodes were placed on Cz site,reference electrodes were placed on A2 site, and grounding electrodes were placed on Fpz site. All electrodes were silver chloride circular electrodes with a diameter of 8 mm, and the scalp electrode impedance was lower than 5 000 Ω. The active electrodes were connected to the positive electrodes, the reference electrodes were connected to the negative electrodes,and the positive wave was integrated upward and the negative wave was downward. Parameter setting pattern of P300 stimulator: high pitch 2 000 Hz (target stimulation) with a probability of 25%; low pitch 1 000 Hz (non-target stimulation) with a probability of 75%. Parameter setting pattern of evoked action potential meter: source trigger, analysis time 1 s,superposition 20 times, low frequency filtering 0.05 Hz,high frequency filtering 20 Hz, sensitivity 20 μV. The participants were required to record the number of times of high pitch they heard and report the records after the test. Only the test with a record accuracy rate higher than 85% was recognized as an effective test.Latency and amplitude of ERPs from the effective tests were taken as the primary outcome in this trial.
2.3.2 Secondary outcomes
PSQI: The PSQI global score was used to evaluate the insomnia condition at baseline, and changes in sleep patterns after 8-week treatment. As a standardized,subjective and self-reporting questionnaire, PSQI includes 7 domains, namely subjective sleep quality,sleep latency, total sleep time, habitual sleep efficiency,sleep disturbances, use of sleeping medication, and daytime drowsiness and dysfunction. Each domain has a set weight between 0 and 3 points that produces one global score ranging from 0 to 21 points. A total score higher than 5 indicates insufficient sleep quality, and the higher the PSQI global score, the severer the insomnia.
2.4 Statistical methods
The SPSS version 21.0 statistical software was used for statistical description and inference after the original data were input through Excel 2010. Measurement data in normal distribution were expressed as mean ±standard deviation ( x ±s) and analyzed by paired t-test or two dependent samples t-test for inter-group comparisons and intra-group comparisons. The measurement data in abnormal distribution were analyzed by Wilcoxon rank-sum test. The enumeration data were expressed by ratio and processed by Chisquare test. The ranked data were analyzed by nonparametric test. The significance level was set at 0.05.
3 Results
3.1 Comparison of the PSQI score
At the baseline, there was no significant difference in the PSQI global score between the two groups (P>0.05).Compared with the baseline, the PSQI global scores in both treatment and control groups showed significant differences after the 8-week treatment (P<0.001,P<0.01). Moreover, the decline in the treatment group was more significant than that in the control group(P<0.001). It can be concluded that both manual acupuncture and sham acupuncture can improve chronic insomnia after 8-week intervention, and the effectiveness of manual acupuncture was superior to that of sham acupuncture (Table 2).
Table 2. Comparison of the PSQI global score between the two groups ( ±s, point)
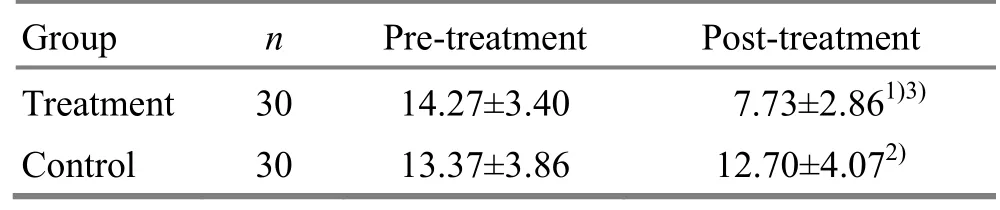
Table 2. Comparison of the PSQI global score between the two groups ( ±s, point)
Note: Compared with the baseline in the same group, 1) P<0.001,2) P<0.01; compared with the control group, 3) P<0.001
Group n Pre-treatment Post-treatment Treatment 30 14.27±3.40 7.73±2.861)3)Control 30 13.37±3.86 12.70±4.072)
3.2 Comparison of the ERPs
At the baseline, there were no significant differences in the latency and amplitude of ERPs between the two groups (P>0.05). In the treatment group, the latencies of N1 and P3, and the amplitudes of N1 and P3 presented significant changes after the intervention(P<0.05, P<0.001). In the control group, no significant difference was discovered in the latency and amplitude of each ERP component after the treatment. There was a significant difference in the latency of P3 between the two groups after the treatment (P<0.01). It can be concluded that manual acupuncture may improve memory impairment in chronic insomniacs by partially influencing the ERPs (Table 3 and Table 4).
3.3 Safety assessment
No serious adverse events were reported in this trial,except that 1 patient from the treatment group had slight hematoma once after receiving acupuncture. That patient was treated with cold compress and recovered in 2 d. No one dropped out from the trial.
Table 3. Comparison of the latencies of ERPs between the two groups ( ±s, ms)
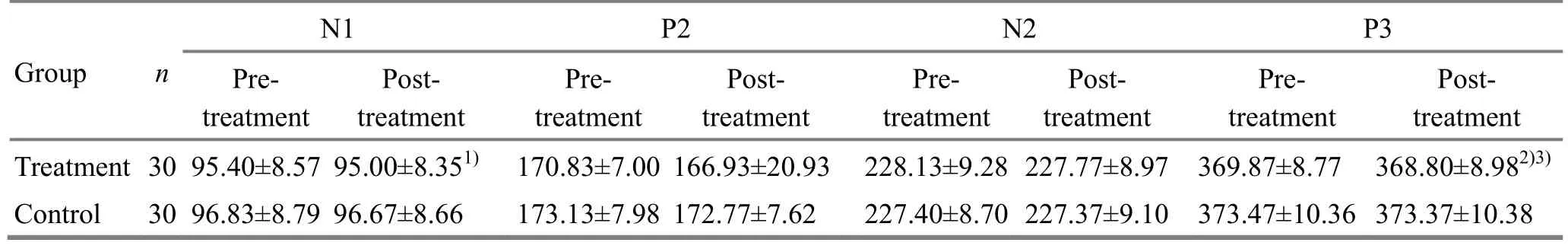
Table 3. Comparison of the latencies of ERPs between the two groups ( ±s, ms)
Note: Intra-group comparison, 1) P<0.05, 2) P<0.001; compared with the control group, 3) P<0.01
N1 P2 N2 P3 Group n Pretreatment Posttreatment Pretreatment Posttreatment Pretreatment Posttreatment Pretreatment Posttreatment Treatment 30 95.40±8.57 95.00±8.351) 170.83±7.00 166.93±20.93 228.13±9.28 227.77±8.97 369.87±8.77 368.80±8.982)3)Control 30 96.83±8.79 96.67±8.66 173.13±7.98 172.77±7.62 227.40±8.70 227.37±9.10 373.47±10.36 373.37±10.38
Table 4. Comparison of the amplitudes of ERPs between the two groups ( ±s, μV)
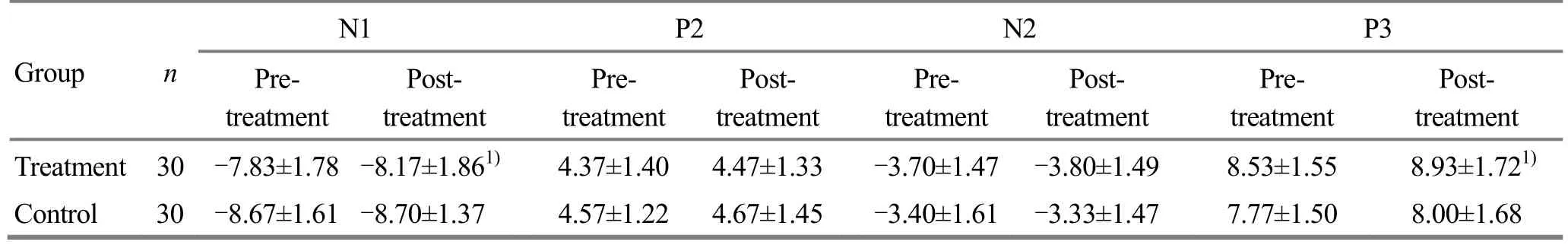
Table 4. Comparison of the amplitudes of ERPs between the two groups ( ±s, μV)
Note: Intra-group comparison, 1) P<0.05
N1 P2 N2 P3 Group n Pretreatment Posttreatment Pretreatment Posttreatment Pretreatment Posttreatment Pretreatment Posttreatment Treatment 30 -7.83±1.78 -8.17±1.861) 4.37±1.40 4.47±1.33 -3.70±1.47 -3.80±1.49 8.53±1.55 8.93±1.721)Control 30 -8.67±1.61 -8.70±1.37 4.57±1.22 4.67±1.45 -3.40±1.61 -3.33±1.47 7.77±1.50 8.00±1.68
4 Discussion
Approximately 35% of adults experience insomnia at least once in their lives[30]. In addition to the severe influence on daily life, CI without proper intervention has been proved to be a high risk factor for impaired function, and the development of other physical and psychological illnesses[31], and it might even link to suicidal ideation[32]. Meanwhile, cognitive impairment,particularly memory loss, and impaired concentration are very common among insomniacs[33]. In the management of CI, satisfactory results might be achieved with short-term use of sedatives and hypnotics, while the serious side effects due to longterm application could not be ignored. Furthermore,long-term use of sleeping pills will further aggravate insomniacs' learning and memory impairments[24].Therefore, more and more chronic insomniacs turn to seek help from TCM, especially acupuncture. To our knowledge, few high-quality studies are available to provide evidence on whether manual acupuncture can improve memory impairment in chronic insomniacs.Hence, a randomized, single-blind, placebo-controlled clinical trial was conducted in this study, in order to investigate if memory would respond to manual acupuncture stimulation among chronic insomniacs based on the observation of ERPs.
According to the results, after 8-week treatment,both real acupuncture and sham acupuncture led to a significant decrease in the PSQI global score. No sufficient evidence indicated improvements in memory impairment by sham acupuncture. However, the latencies of N1 and P3 were significantly shortened, and the amplitudes of N1 and P3 were significantly increased after real acupuncture treatment, which suggested that long-term and regular manual acupuncture stimulation might improve the memory impairments among chronic insomniacs. In the studies of insomnia and memory, the latency and amplitude of P3 have been considered to reflect the cognition and memory condition of the brain. Since its close relationship with both cognitive functions and sleep, P3 is also known as an approach to studying human brain.Therefore, memory impairments and other cognitive impairments caused by sleep disorders can be assessed by P3[33-34]. For the decline in PSQI global score after sham acupuncture intervention, we believe that sham acupuncture might bring some psychological comforts to patients with insomnia. However, further conclusions need to be verified through more rigorous clinical trials.
According to the basic theories of TCM, brain is the sea of marrow, and the kidney stores essence which generates marrow. Memory impairments are usually due to the deficiency of kidney essence. Hence, it is possible to improve memory impairments and brain function through supplementing kidney essence, and that's why Taixi (KI 3) was selected in this study. The head points, including Sishencong (EX-HN 1), Shenting(GV 24) and Benshen (GB 13), are a classical acupoint combination created by Dr. Yang Jia-san, who was the first chief of School of Acupuncture-moxibustion and Tuina of Beijing University of Chinese Medicine, and have been widely used in clinic for various types of insomnia. In this combination, Shenting (GV 24) is the crossing point of the Governor Vessel, Bladder Meridian and Stomach Meridian. Since the Governor Vessel links the three yang meridians of hand and the three yang meridians of foot to the brain, Shenting (GV 24) can be viewed as a gathering place of qi and blood in the Governor Vessel. Meanwhile, the Bladder Meridian is derived from the brain, and administrates the activities of mind and brain. Therefore, qi and blood in meridians can be regulated and delivered to brain via puncturing Shenting (GV 24). Sishencong (EX-HN 1) is an extraordinary acupoint. Benshen (GB 13) is the origin of qi in the Gallbladder Meridian, and is also the pivot which manages the opening and closing of the three yang meridians. Regulating both the Governor Vessel and Gallbladder Meridian can correct the imbalance of yin and yang at night and restore the normal ‘day-night cycle'[24]. Baihui (GV 20) is not only a point of the Governor Vessel, but also the crossing of various meridians. Hence, the regulation of yin and yang in Zang-fu organs may be achieved by puncturing Baihui(GV 20). Shenmen (HT 7) is also widely used for insomnia and amnesia in clinical practice. Previous laboratory experiments also showed that learning and memory ability might be improved by stimulating acupoints of the Governor Vessel to inhibit the cholinesterase activity in the brain[35], promote the hippocampal synaptophysin expression, enhance the hippocampal synaptic plasticity, and accelerate the synaptic transmission in hippocampal neurons[36].
Since there were no adverse events reported in this trial, and no participants withdrew or dropped out, we believe that eight consecutive weeks of acupuncture intervention should be acceptable and safe for patients with CI. Based on the results of the present study, the manual acupuncture intervention is worthy of clinical promotion.
It should be noted that there were some methodological limitations in this trial, particularly the absence of evaluation based on an objective outcome measure such as polysomnography (PSG), which may result in the statistical bias in outcome assessments. In addition, the bias may also be caused by the relatively small sample size and no follow-up period. To draw a clear conclusion, multi-centered randomized singleblind placebo-controlled clinical trials with a large sample size and long-term observation are required.Besides, PSG or actigraphy is also expected to be adopted as the objective outcome measure, combined with self-reporting evaluation methods such as Karolinska sleep diary, to provide a more practical and rigorous clinical research pattern in sleep-related clinical studies.
This trial provided evidence to prove the satisfactory short-term effects of manual acupuncture in the treatment of CI coupled with memory impairments. It should be suggested that acupuncture can be taken as a safe and effective non-pharmacological intervention option for insomniacs with memory impairments.
Conflict of Interest
There was no potential conflict of interest in this article.
Acknowledgments
This work was supported by Scientific Project of National Science & Technology Pillar Program During the Eleventh Five-year Plan Period (國家“十一五”科技支撐計劃項目, No. 2007BAI10B01-027); Shanghai Municipal Commission of Health and Family Planning, Scientific and Technological Innovation Project of TCM: Mobile Internet-based Insomnia Rehabilitation Prevention(Chronic Disease Management) Guidance Platform [上海市衛(wèi)生和計劃生育委員會中醫(yī)藥科技創(chuàng)新項目——基于移動互聯(lián)網(wǎng)的失眠癥“治未病”康復(fù)預(yù)防(慢病管理)指導(dǎo)平臺, No. ZYKC20161016].
Statement of Informed Consent
Informed consent was obtained from all individual participants included in this study.
Received: 18 May 2018/Accepted: 19 June 2018
 Journal of Acupuncture and Tuina Science2018年6期
Journal of Acupuncture and Tuina Science2018年6期
- Journal of Acupuncture and Tuina Science的其它文章
- Effects of electroacupuncture of different frequencies on SP and VIP expression levels in colon of rats with slow transit constipation
- Experimental study on the effect of An-pressing and Rou-kneading Huantiao (GB 30) on certain brain nuclei of pleasure circuits in rats with chronic neuralgia
- Fire-needle therapy for deglutition disorders in post-stroke pseudobulbar palsy:a randomized controlled trial
- Therapeutic effect observation on acupuncture plus umbilicus application with Chinese medicine in treating detrusor underactivity
- Effect of tuina exercise on simple obesity in college students
- Clinical observation on tuina plus foot bath with Chinese medicine for diabetic foot in early stage
