Fire-needle therapy for deglutition disorders in post-stroke pseudobulbar palsy:a randomized controlled trial
Guo Yu-huai (郭玉懷), Sun Zhong-ren (孫忠人), Cai Shuo (蔡碩), Jin Ze (金澤), Wei Qing-shuang (魏慶雙), Jiang Fan (姜凡),Wang Ming-zhen (王明振), Yin Hong-na (尹洪娜)
1 Heilongjiang University of Chinese Medicine, Harbin 150040, China
2 Guangzhou University of Chinese Medicine, Guangdong 510006, China
3 The Second Hospital Affiliated to Heilongjiang University of Chinese Medicine, Harbin 150001, China
Abstract Objective: To observe the clinical efficacy of fire-needle therapy in treating deglutition disorders due to pseudobulbar palsy in the remission stage of stroke.
Keywords: Acupuncture Therapy; Fire-needle Therapy; Scalp Stimulation Areas; Stroke; Complications; Pseudobulbar Palsy; Deglutition Disorders; Randomized Controlled Trials
Stroke is a major cause of death and disability.Deglutition disorders usually happen in hours or days after stroke, often co-occurring with aspiration pneumonia, electrolyte disturbances and malnutrition during the in-bed period. It is found that almost 50% of all pneumonia cases are caused by deglutition disorders,which are also related to the high mortality and disability rates of stroke[1-2]. Although some of the post-stroke deglutition disorder patients don't spend too much time to restore their swallowing function,11%-50% of the patients still suffer from the swallowing difficulty even in half a year after the onset of stroke. It not only causes significant influence on the patients'quality of life, but also brings much trouble to their families[2]. Therefore, it is very important to seek a cost-effective treatment to tackle this problem. This study aimed to observe the therapeutic efficacy of fire-needle therapy in treating deglutition disorders due to pseudobulbar palsy in the remission stage of stroke.The report is given as follows.
1 Clinical Materials
1.1 Study design
Blind method was only applied to the evaluators, not to any physicians or patients involved in the trial. The subjects were from the Second Hospital Affiliated to Heilongjiang University of Chinese Medicine. Before the recruitment, they were initially screened at the Clinical Trial Screening Center. According to the randomization protocol designed ahead, the eligible subjects who had signed the informed consent form were divided into either a fire-needle group or a rehabilitation group at 1:1. They then received the corresponding 3-week intervention in the ward, and were evaluated before and after the intervention by two trained evaluators.
1.2 Diagnostic criteria
1.2.1 Diagnostic criteria of stroke
The diagnostic criteria of stroke of traditional Chinese medicine (TCM) referred to the Standard for Diagnosis and Therapeutic Effect Evaluation of Stroke (trial)[3].
The diagnostic criteria of stroke of the Western medicine were based on the criteria for cerebral infarction and cerebral hemorrhage from the Key Diagnostic Points for Cerebrovascular Diseases[4].
1.2.2 Diagnostic criteria of pseudobulbar palsy
The diagnostic criteria of pseudobulbar palsy referred to Practicing Neurology[5]and Six Consummate Skills of Acupuncture-moxibustion: Modern Acupuncturemoxibustion Therapies for Neuropathies[6]; the diagnostic criteria of post-stroke deglutition disorders were in accordance with the Diagnosis of Post-stroke Deglutition Disorders[7].
1.3 Inclusion criteria
Conforming to the above diagnostic criteria; ages 40-75 years old; disease duration of stroke 2-12 weeks;capable of completing the swallow test; the diagnosis of stroke was confirmed; without a previous history of difficulty swallowing; willing to participate in the trial and having signed the informed consent form, or the consent form was signed by the guardian upon the agreement of the patient; not involved in other clinical trials at the same time; capable of completing the required questionnaire; item 1a of the National Institutes of Health stroke scale (NIHSS) was scored 0 or 1.
1.4 Exclusion criteria
Pregnant or breast-feeding women; suspicious diagnosis of dementia according to the evaluators;unstable cardiac or pulmonary function; abnormal cervical anatomical structure; deglutition disorders due to other diseases rather than stroke; those diagnosed as progressive neuropathies, such as Parkinson's disease;those with chronic cardiac or respiratory disease.
1.5 Rejection and dropout criteria
Did not follow the treatment protocol or used other treatment methods concurrently, which might affect the outcome according to the evaluators; the condition aggravated or there occurred other severe diseases during the study.
1.6 Statistical methods
All the data were processed by IBM SPSS Statistics version 23.0. Kolmogorov-Smirnov Test was adopted to examine the normal distribution. When the measurement data were in normal distribution and under homogeneity of variance, they would be expressed as mean ± standard deviation (±s); the intra-group comparisons were analyzed by paired t-test,and the between-group comparisons were examined by independent samples t-test. When the data were in abnormal distribution and under homogeneity of variance, Mann-Whitney U test was used for the measurement data, Chi-square test was used for the enumeration data, and Ridit test was adopted for the ranked data. P<0.05 was considered to be statistically significant.
1.7 Baseline data
Between February 2017 and February 2018, a total of 62 subjects were recruited. They were randomized into either a fire-needle group or a rehabilitation group based on their visiting sequence by IBM SPSS Statistics version 23, with 31 cases in each group.
During the intervention, 2 cases in the fire-needle group dropped out: one was due to the fear of fire needle and was taken as invalid; the other case was also regarded as invalid since the patient failed to follow the treatment and the result was unsatisfactory according to the physician. Three cases in the rehabilitation group dropped out: two cases quitted halfway and the other one was rejected for receiving other treatment.
At the baseline, there were no significant differences in the data of age, gender, disease duration, body mass index (BMI), and the scores of NIHSS, dysphagia severity rating scale (DSRS), the modified Mann assessment of swallow ability (MMASA) and Kubota Toshio swallow test (KTST) between the two groups (all P>0.05),indicating that the baseline data were equivalent between the two groups and they were comparable(Table 1).
The process of the trial is shown in Figure 1.
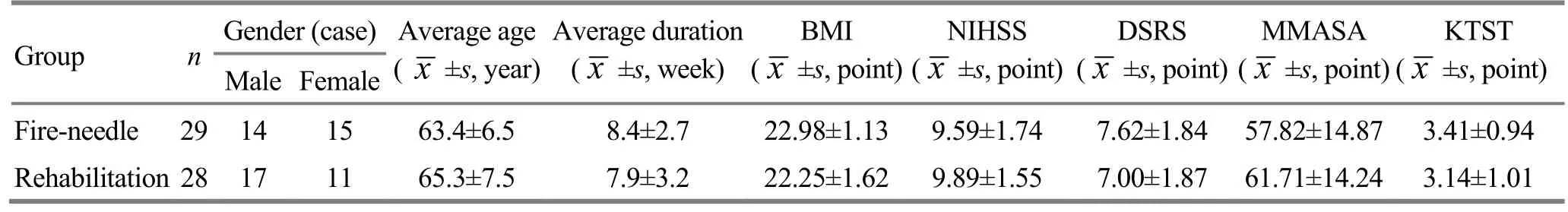
Table 1. The baseline data of the two groups
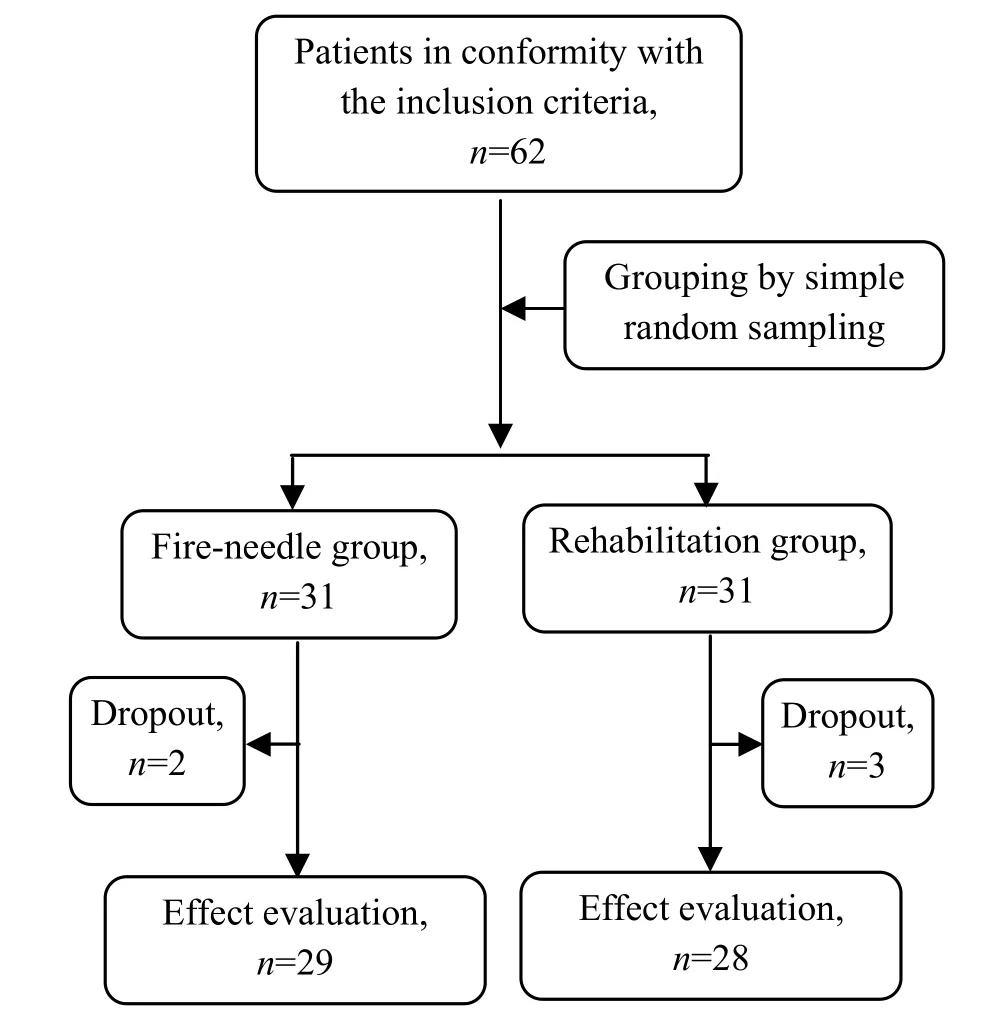
Figure 1. Flow chart of the clinical trial
2 Treatment Methods
2.1 Basic intervention
The patients were given basic symptomatic interventions for stroke and other diseases, as well as acupuncture.
Acupoints: Motor Zone, Sensory Zone and Speech Zone of Jiao's scalp acupoints on the healthy side;Baihui (GV 20); bilateral Fengchi (GB 20), Wangu (GB 12),Yuzhen (BL 9) and Tianzhu (BL 10); Shousanli (LI 10),Waiguan (TE 5), Hegu (LI 4), Jianyu (LI 15), Quchi (LI 11),Biguan (ST 31), Futu (ST 32), Zusanli (ST 36),Yanglingquan (GB 34), Yinlingquan (SP 9), Sanyinjiao(SP 6), Qiuxu (GB 40) and Taichong (LR 3) on the affected side.
Method: Filiform needles of 0.30 mm in diameter and 40 mm in length or elongate needles of 0.30 mm in diameter and 125 mm in length were used. Pointtoward-point needling method was applied to Yuzhen(BL 9) towards Tianzhu (BL 10), Jianyu (LI 15) towards Quchi (LI 11), Biguan (ST 31) towards Futu (ST 32),Zusanli (ST 36) towards Yanglingquan (GB 34), and Yinlingquan (SP 9) towards Sanyinjiao (SP 6). The scalp acupoints were treated with superficial needling and the rest points were perpendicularly punctured. The treatment was performed twice a day, 30 min for each session.
2.2 Rehabilitation group
In addition to the basic interventions, the speech therapist provided rehabilitation training which included the following seven aspects.
One, repeatedly gently stimulated the cheeks,zygomatic arches, soft palate, posterior pharyngeal wall and tongue with ice cube every day, and asked the patient to pronounce ‘a(chǎn)', ‘ka' and ‘pa', etc. based on his condition and to swallow saliva.
Two, selected a proper diet pattern and dieting position according to the patient's condition, cleansed the oral cavity immediately after intake of food, and asked to patient to practice swallow during the intermittences.
Three, relaxed the patient's neck and shoulders.
Four, lifted and swung the upper limbs, while keeping the airway open and the movements in coordinated.
Five, once the groan was down, asked the patient to be seated and keep as close as possible to the back of the chair and pronounce ‘a(chǎn)' simultaneously.
Six, the training for lips, tongue and jaw.
Seven, focus on the practice of stress, tone,intermittence and pause and the patient should follow the changes of tone and volume of the device.
2.3 Fire-needle group
In addition to the basic interventions, the fire-needle group received fire-needle therapy.
Acupoints: Fengchi (GB 20), Gongxue (Extra),Lianquan (CV 23), Waijinjin (Extra), Waiyuye (Extra),Zhiqiang (Extra), Tunyan 1 (Extra), Tunyan 2 (Extra) and Renying (ST 9).
Method: Fine tungsten steel fire needles of 0.50 mm in diameter and 40 mm in length were chosen. Prior to the treatment, the to-be-treated acupoints were properly exposed and the assistant sterilized the acupoints with iodine. Then, the practitioner held a spirit lamp with one hand and swiftly punctured the above acupoints with the fire needle when the needle tip was burnt red, by depth of 3-5 mm for Fengchi(GB 20), Gongxue (Extra), Zhiqiang (Extra), Tunyan 1(Extra), Tunyan 2 (Extra) and Renying (ST 9), and by 10-15 mm for Lianquan (CV 23), Waijinjin (Extra) and Waiyuye (Extra). At the end of puncture, the assistant pressed the punctured areas with cotton balls to prevent bleeding. The above points were divided into five groups, i.e. Fengchi (GB 20) and Zhiqiang (Extra),Gongxue (Extra) and Tunyan 1 (Extra), Tunyan 2 (Extra)and Lianquan (CV 23), Waijinjin (Extra) and Waiyuye(Extra), and bilateral Renying (ST 9). The five groups of points were selected alternately, one group each day.The treatment was performed once a day, 5 times a week, for a total of 3 weeks.
Tunyan 1 (Extra), Tunyan 2 (Extra), Gongxue (Extra)and Zhiqiang (Extra) were empirical points used by Prof.Gao Wei-bin to treat bulbar paralysis[4,8]and once won the second prize of the National Scientific and Technological Progress Award. Tunyan 1 (Extra) is located between the hyoid bone and Adam's apple, in the depression 0.5 cun away from the anterior midline;Tunyan 2 (Extra) is located on the posterior edge of sternocleidomastoid muscle, on the same level of mentolabial furrow. Gongxue (Extra) is located 1.5 cun below Fengchi (GB 20), on the same level of lower lip.Zhiqiang (Extra) is between the hyoid bone and the superior thyroid notch. The details are shown in Figure 2 and Figure 3.

Figure 2. Locations of Tunyan 1 (Extra) and Zhiqiang (Extra)
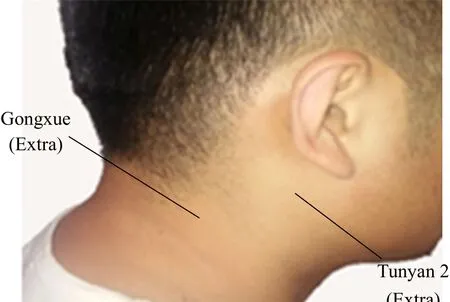
Figure 3. Locations of Tunyan 2 (Extra) and Gongxue (Extra)
3 Observation of Therapeutic Efficacy
3.1 Observation items
The participants were evaluated before and after the treatment by the following scales. The adverse events and unaccomplished items were also recorded.
3.1.1 DSRS[9]
The DSRS evaluates the difficulty swallowing from three dimensions: water intake, food intake and diet supervision. Each dimension can be scored 0-4 points, 0 standing for normal swallowing function and 4 standing for loss of swallowing function. The patients were scored based on their ability to differentiate water and food and their dependence on the therapist.
3.1.2 MMASA[1]
The MMASA consists of 12 items to evaluate swallow,including consciousness, cooperation, respiration,swallow, comprehension ability, aphasia, swallowing saliva, movement of tongue, tension of tongue, vomit,cough reflex and taste. The full score is 100 points and the minimum score is 19 points. The higher the score,the better the swallow ability. A score >95 points indicates the ability to diet independently, while a score≤94 points suggests the therapist to perform swallow training or guidance for the patients.
3.1.3 KTST[10]
In KTST, the participant is offered 30 mL warm water and asked to try to drink it in a normal way, during which the swallow and choke conditions are observed.Level Ⅰ, finish drinking by one time without choking;level Ⅱ, finish drinking by two times without choking;level Ⅲ finish drinking by once time but with choking;level Ⅳ, finish drinking by multiple times with choking;level Ⅴ, unable to finish drinking. Among which,patients at level Ⅱ and Ⅲ require guidance in dieting,while patients at level Ⅳ and Ⅴ need intensive treatment.
3.2 Criteria of therapeutic efficacy
The therapeutic efficacy was measured by referring to the method of Shi Xue-min[11]for evaluating difficulty in swallowing based on the level of KTST.
Cured: KTST level Ⅰ.
Markedly effective: Improved by 2 levels or more in KTST.
Effective: Improved by one level in KTST.
Invalid: No improvement in the performance of KTST.
3.3 Results
3.3.1 Comparison of the scores of DSRS, MMASA and KTST
Before the treatment, there were no significant differences in the scores of DSRS, MMASA and KTST between the two groups (P>0.05). After 3-week treatment, the scores of DSRS, MMASA and KTST showed significant changes in both groups (all P<0.05);the scores of DSRS, MMASA and KTST in the fire-needle group were significantly different from those in the rehabilitation group (all P<0.05), indicating that the patients in the fire-needle group obtained more significant improvement than the patients in the rehabilitation group (Table 2).
3.3.2 Comparison of the therapeutic efficacy
After the treatment, the total effective rate was 100.0% in the fire-needle group, versus 96.4% in the rehabilitation group, and the between-group difference was statistically insignificant (P>0.05); the cured and markedly effective rate was 100.0% in the fire-needle group versus 57.1% in the rehabilitation group, and the between-group difference was statistically significant(P<0.05), suggesting that the fire-needle group produced a more significant therapeutic efficacy than the rehabilitation group (Table 3).
3.3.3 Adverse events and incomplete treatment
The occurrence rate of adverse events and incomplete treatment was 13.8% in the fire-needle group versus 10.7% in the rehabilitation group, and the between-group difference was statistically insignificant(P>0.05), (Table 4).
Table 2. Comparison of the scores of DSRS, MMASA and KTST (±s, point)
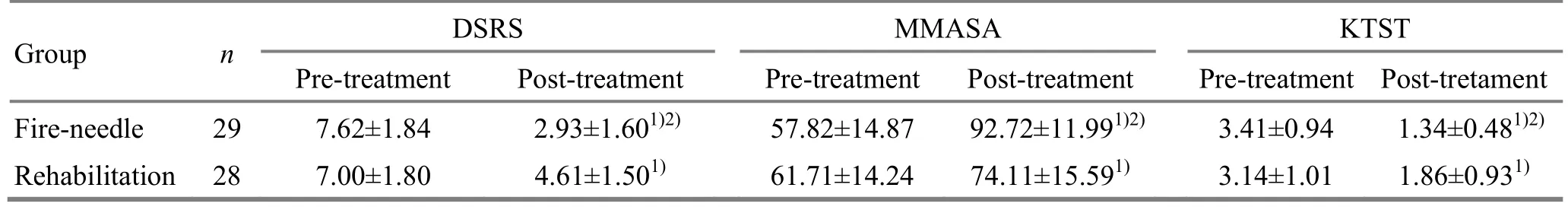
Table 2. Comparison of the scores of DSRS, MMASA and KTST (±s, point)
Note: Compared with the baseline in the same group, 1) P<0.05; compared with the rehabilitation group after the treatment, 2) P<0.05
Group n DSRS MMASA KTST Pre-treatment Post-treatment Pre-treatment Post-treatment Pre-treatment Post-tretament Fire-needle 29 7.62±1.84 2.93±1.601)2) 57.82±14.87 92.72±11.991)2) 3.41±0.94 1.34±0.481)2)Rehabilitation 28 7.00±1.80 4.61±1.501) 61.71±14.24 74.11±15.591) 3.14±1.01 1.86±0.931)
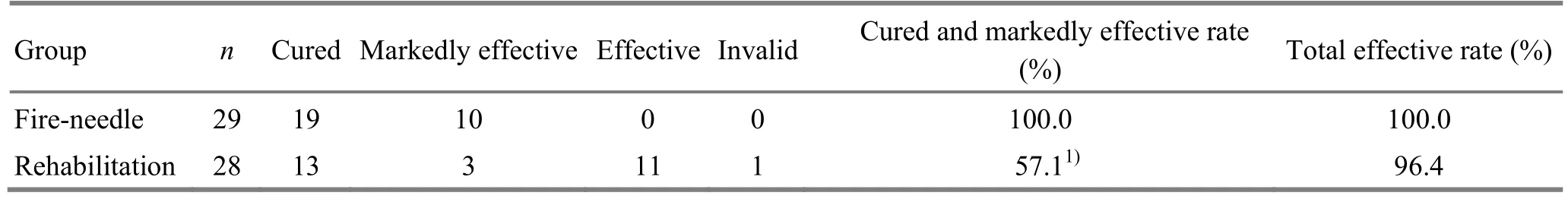
Table 3. Comparison of the clinical efficacy (case)
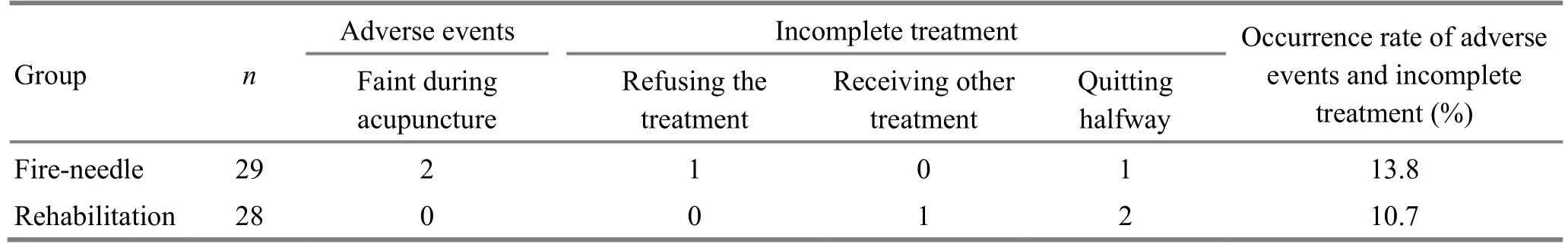
Table 4. Comparison of the adverse events and incomplete treatment (case)
4 Discussion
Deglutition disorder due to pseudobulbar palsy in post-stroke remission state belongs to throat Bi-impediment syndrome in TCM. Using fire-needle therapy to treat throat Bi-impediment syndrome has already been recorded in Ling Shu (Spiritual Pivot),which provides the theoretical evidence. Fire-needle therapy is under the scope of warm unblocking acupuncture method, one of the three unblocking therapies invented by the national TCM master He Pu-ren, who believed that fire-needle therapy can reinforce yang qi, activate meridian qi and expel pathogens with its warm-hot nature. Since it can use fire to warm the yang aspect, warm and unblock meridians and collaterals, produce heat with heat, and promote the circulation of qi-blood, this therapy is usually applied to treat lumps or nodules formed by qi,blood, phlegm or dampness[12]. Throughout constant clinical practice and theoretical research, doctors from different generations hold that stroke should be associated with wind, fire, phlegm, stagnation, blood and deficiency. There is no such term as pseudobulbar palsy in classics, but there is a similar term named Yin Fei (aphasia and paralysis). Hence, deglutition disorder due to pseudobulbar palsy after stroke should also be related to phlegm, blood and stagnation, etc. Therefore,fire-needle therapy is often used to treat throat Bi-impediment associated with qi, blood, phlegm and stagnation. Besides, acupuncture has been recommended to treat deglutition disorders (grade B),which should be sufficient to prove the effectiveness of acupuncture in the treatment of deglutition disorders[13-15].
A normal swallowing process can be divided into 5 phases. The oral phase is mainly to sense and propel the food, complete mastication, and form the food bolus. In the pharyngeal phase, the upper esophageal sphincter opens due to the swallowing reflex and the bolus enters the esophagus. The food bolus is finally pushed into the stomach via the cricopharyngeal sphincter in the esophageal phase. In oral phase deglutition disorder, it is probably because the tongue has lost its sensation or movement, and the teeth are either unclosed or over-closed due to mimetic paralysis,so there accumulates too much secretion in oral cavity and the food can't be maintained inside the mouth or transported to the pharynx but stuck at the hard palate.It usually manifests as inability to swallow, coupled with sialorrhea and choking. Pharyngeal phase deglutition disorder often happens when the involved muscles fail to coordinate. In this condition, the food bolus may be inhaled into the respiratory tract during respiration, or the food may enter the nasal cavity. When esophageal phase deglutition disorder occurs, it is usually because of the dysfunction of esophageal peristalsis or esophageal spasm which can affect the downward transportation of the food. But, since the esophagus is not governed by the swallowing center of the cerebral cortex, so the pseudobulbar palsy-induced deglutition disorder usually doesn't occur in the esophageal phase,but more in the oral and pharyngeal phases[6,16].Therefore, to directly or indirectly stimulate the tongue and pharynx should be the key step in the treatment of this type of deglutition disorder.
Through years' clinical experience, Prof. Gao Wei-bin has brought up nape acupuncture therapy to treat bulbar palsy and pseudobulbar palsy. Lianquan (CV 23)is located in the depression on the upper edge of hyoid bone, and it has mylohyoideus muscles and genioglossus in the deeper layer. Waijinjin (Extra) and Waiyuye (Extra) are below the jaw, 1.5 cun above the depression of thyroid cartilage, 0.3 cun away on the two sides [Waijinjin (Extra) on the left and Waiyuye (Extra)on the right]. According to Prof. Gao, stimulating Lianquan (CV 23), Waijinjin (Extra) and Waiyuye (Extra)can directly work on the hypoglossal nerve and activate the tongue to restore the function of tongue for propelling food during swallowing. Zhiqiang (Extra),Tunyan 1 (Extra) and Tunyan 2 (Extra) are novel points discovered by Prof. Gao to treat deglutition disorders in bulbar palsy or pseudobulbar palsy, and are usually treated with slow lifting-thrusting and twisting manipulations to help recover the motor function of glossopharyngeal nerves and muscles. Zhiqiang (Extra)is between the epiglottic cartilage and thyroid notch,with thyrohyoid ligament and hyoepiglottic ligament inside. Tunyan 1 (Extra) is located between the hyoid bone and Adam's apple, where resides the middle constrictor of pharynx. Tunyan 2 (Extra) is on the same level of mentolabial furrow, in the depression anterior to the vertebral body of C3, with the upper constrictor of pharynx located in the deep[7,17]. Prof. Gao believes that improving the oral phase should be the crucial step in the treatment of pseudobulbar palsy[18]. But there are other researchers who hold that the oral phase and pharyngeal phase should both be stressed[17]. Based on the above opinions, we chose to intervene both tongue and pharynx. Moreover, there are already numerous evidences that have proven the effect of stimulating glossopharyngeal region in improving the swallowing function in pseudobulbar palsy after stroke[18-20].
Therefore, in this study, we punctured Lianquan(CV 23), Waijinjin (Extra) and Waiyuye (Extra) to intensify the stimulation to the hyoid muscles; Fengchi(GB 20) and Gongxue (Extra) were treated to promote the cerebral blood circulation; Zhiqiang (Extra), Tunyan 1 (Extra) and Tunyan 2 (Extra) were punctured to stimulate the pharyngeal muscles. This glossopharyngeal treatment paradigm was to improve the swallowing function in a synergetic manner and to form a repairing cycle of stimulation, repair,re-stimulation, and re-repair. Meanwhile, fire-needle therapy can intensively stimulate the muscle region of the meridian in the glossopharyngeal area, which can help regulate and unblock the meridians and collaterals passing by.
This study showed that after a 3-week treatment, the scores of DSRS, MMASA and KTST were significantly improved in the two groups (all P<0.05), indicating that the two methods both can ameliorate the symptoms;the fire-needle group achieved more significant improvements in the three scales compared with the rehabilitation group (all P<0.05), suggesting that fire-needle therapy can produce a more significant effect in improving the symptoms than rehabilitation.The fire-needle group had a significantly higher cured and markedly effective rate than the rehabilitation group (P<0.05), indicating that fire-needle therapy can produce a better efficacy in treating deglutition disorders due to pseudobulbar palsy in the remission stage of stroke compared with rehabilitation. There was no significant difference in the occurrence rate of adverse events and uncompleted treatment between the two groups (P>0.05).
In summary, fire-needle therapy can effectively promote the recovery of swallowing function in pseudobulbar palsy in the remission stage of stroke, and is worth promoting in clinical practice.
Conflict of Interest
The authors declared that there was no potential conflict of interest in this article.
Acknowledgments
This work was supported by National Natural Science Foundation of China (國家自然科學(xué)基金, No. 81473761,No. 81704181); Key Research Project of Economic and Social Development in Heilongjiang Province (黑龍江省經(jīng)濟(jì)社會發(fā)展重點(diǎn)研究課題, No. JD2017019).
Statement of Informed Consent
Informed consent was obtained from all individual participants or their relatives in this study.
Received: 28 May 2018/Accepted: 19 June 2018
 Journal of Acupuncture and Tuina Science2018年6期
Journal of Acupuncture and Tuina Science2018年6期
- Journal of Acupuncture and Tuina Science的其它文章
- Effects of electroacupuncture of different frequencies on SP and VIP expression levels in colon of rats with slow transit constipation
- Experimental study on the effect of An-pressing and Rou-kneading Huantiao (GB 30) on certain brain nuclei of pleasure circuits in rats with chronic neuralgia
- Memory response to manual acupuncture in chronic insomniacs: evidence from event-related potentials
- Therapeutic effect observation on acupuncture plus umbilicus application with Chinese medicine in treating detrusor underactivity
- Effect of tuina exercise on simple obesity in college students
- Clinical observation on tuina plus foot bath with Chinese medicine for diabetic foot in early stage
