Chronic pancreatitis: Pain and computed tomography/magnetic resonance imaging findings
Yue Feng,Ling-Ji Song,Bo Xiao
Abstract Chronic pancreatitis (CP) is a fibroinflammatory disease characterized by irreversible destruction of pancreatic tissue.With the development of the disease,it may lead to exocrine and/or endocrine insufficiency.CP is one of the common diseases that cause abdominal pain,which will not get permanent spontaneous relief as the disease evolves.The American College of Gastroenterology clinical guidelines recommend computed tomography or magnetic resonance imaging as the first-line examination for the diagnosis of CP.CP common imaging findings include pancreatic atrophy,irregular dilatation of the pancreatic duct,calcification of pancreatic parenchyma,pancreatic duct stones,etc.In clinical practice,whether any correlations between CP-induced abdominal pain patterns (no pain/constant/intermittent pain) and corresponding imaging findings present are not well known.Therefore,this review aims to comprehensively sort out and analyze the relevant information by collecting lots of literature on this field,so as to construct a cross-bridge between the clinical manifestations and imaging manifestations of CP patients.Also,it provides an imaging basis and foundation for the classification and diagnosis of abdominal pain types in clinical CP patients.
Key Words: Chronic pancreatitis;Pancreatitis;Abdominal pain;Computed tomography;Magnetic resonance imaging
lNTRODUCTlON
Chronic pancreatitis (CP) is a fibroinflammatory syndrome caused by various causes.Long-term recurrent pancreatitis causes normal pancreatic parenchyma to be replaced by fibrotic tissues.With the development of the disease,pancreatic tissue and function undergo irreversible changes and destruction,which eventually lead to chronic abdominal pain,exocrine and endocrine pancreatic insufficiency[1,2].
The global incidence of CP is approximately 10 cases per 100,000 general population per year,and the incidence is increasing over time.Notably,the incidence of CP is twice as high in men as in women[3,4].The general clinical manifestations of patients with CP are abdominal pain,nausea,vomiting,etc.,among which abdominal pain is the most common (about 76% of CP patients)[5].However,although it is not common,10% of patients with CP are pain-free[6].The pain manifestations of CP are highly variable and diverse,which can even be converted to each other.Unfortunately,the mechanism of pain is incompletely understood.
For the diagnosis of CP,the American College of Gastroenterology (ACG) clinical guidelines recommend computed tomography (CT) or magnetic resonance imaging (MRI) as the first-line examination[7].
The objective of the present review is to deeply investigate the pain,CT or MRI manifestations of CP patients,and to find out whether there are some change trends or relationships between pain and imaging findings,so as to build a crossbridge between clinical manifestations and imaging manifestations of CP patients.Also,it can provide an imaging basis and foundation for the classification and diagnosis of abdominal pain types in clinical CP patients,which may improve the diagnostic accuracy and the prognosis of CP patients.
PRELlMlNARY UNDERSTANDlNG OF CP
The first definition of CP was proposed in 1946[8],and a new mechanistically derived definition of CP was published by Whitcombet al[9] in 2016,that is,CP is characterized by pathologic fibro-inflammatory syndrome of the pancreas in individuals with genetic,environmental and other risk factors such as hypercalcemia,hypertriglyceridemia,autoimmune disorders and so forth.Advanced CP is featured with pancreatic atrophy,fibrosis,chronic pain,ductal distortion and strictures,calcifications,dysplasia,pancreatic exocrine dysfunction,and endocrine dysfunction[9,10].
CP is a fibroinflammatory disease of the pancreas.Its pathophysiology is very complex and the pathogenesis is not completely understood.Although the mechanism of CP is complex,a large number of studies have shown a similar development trend,that is,various causes lead to progressive irreversible damage to the pancreatic parenchyma,and the pancreatic enzymes release following the injury of the exocrine tissue leading to inflammation.Long-term recurrent pancreatitis and injury can activate pancreatic stellate cells,leading to the formation of fibers and scars.Finally,the pancreas shrinks and hardens,resulting in exocrine and endocrine insufficiency of the pancreas[11-14].
THE PAlN OF CP
The clinical manifestations of CP are mainly upper abdominal pain,which is complex and multimodal.The pain pattern varies according to the temporal nature and severity of CP.According to the temporal nature of pain,it can be divided into constant or intermittent pain[15].According to the severity of pain,it can be divided into mild,moderate,or severe.Previous studies[10,16,17] used five types of pain patterns (A-E) (Table 1),and patients were required to choose from five pain patterns according to the type and severity of their pain.The most common pain pattern is the 'D' type,which is characterized by constant mild to moderate pain plus episodes of severe pain.In addition,in a retrospective study of 54 CP patients,Bahuvaet al[18] found that the presence or absence of pain was not significantly related to the severity of CPstructural changes,regardless of the structural changes.Therefore,this study showed that pancreatic morphological abnormalities had a poor predictive ability for CP pain.
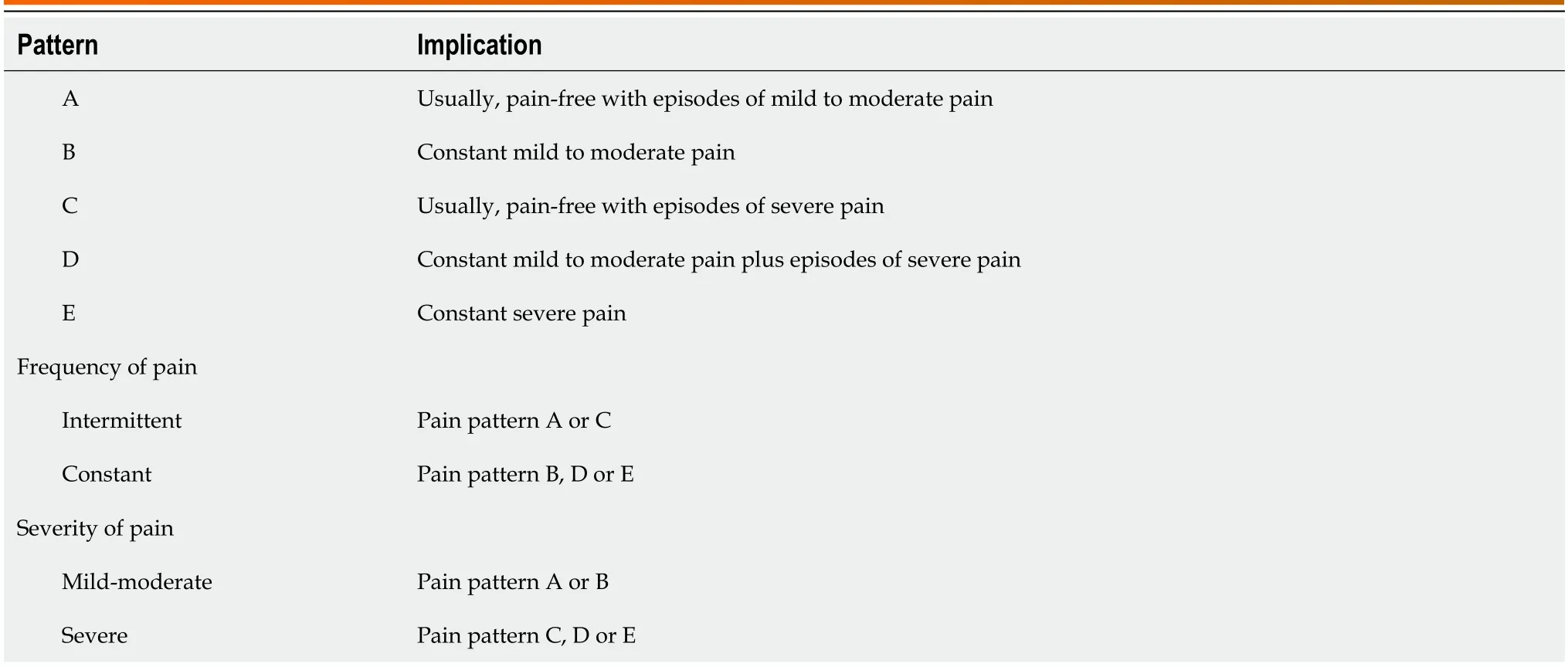
Table 1 Patterns and classification of pain[10,16,17]
CP not only have a variety of pain patterns but also have a complex mechanism of pain.Including multiple factors,such as pancreatitis;the pancreatic duct is compressed and narrowed due to stones or strictures,which may lead to duct hypertension or pancreatic ischemia and further cause pain;and complications such as pseudocysts,local inflammatory masses,duodenal and bile duct obstruction[19,20].At present,the common CP pain assessment tools recommended by the international consensus guidelines include the Visual Analogue scale,Izbiki pain score,McGill Pain Questionnaire,and so on[21].
In the early years,some scholars[22,23] believed that the spontaneous relief of pain depended on the progressive development of CP,and believed that the pain of CP would improve with progressive pancreatic insufficiency (such as severe exocrine/endocrine insufficiency,severe duct abnormalities,more pancreatic calcification,etc.),especially for alcoholic CP,which is the so-called "burn-out" hypothesis.
However,most studies[16,24,25] have shown that the pain of CP did not seem to be significantly improved over time,and it was not uncommon for patients to experience pain recurrence during follow-up.
Combined with the study of Dimcevskiet al[26],it has been shown that there are neurological components in CPinduced pain,and cortical reorganization is a pathogenesis of CP patients,indicating that the pain of CP may be largely independent of pancreatic fibrosis and progressive pancreatic insufficiency.The possible phenomenon is that as the disease progresses,the pain of CP patients may be alleviated,but it cannot be significantly relieved permanently.Therefore,waiting for spontaneous pain relief seems to be inaccurate and not worthy of praise.
CT/MRl FlNDlNGS OF CP
The diagnosis of CP is to combine its clinical features with characteristics of CT or MRI,endoscopic ultrasonography (EUS),and pancreatic function examination[7,19].Clinically,CT or MRI recommended by the ACG clinical guidelines are often used as the first-line examination for the diagnosis of CP[7].The diagnostic criteria for CP can be traced back to the Cambridge classification of pancreatic morphology in 1984 (Table 2)[27],and the M-Annheim classification of CP proposed by Schneideret al[14] in 2007 (Table 3),as detailed in the tables.
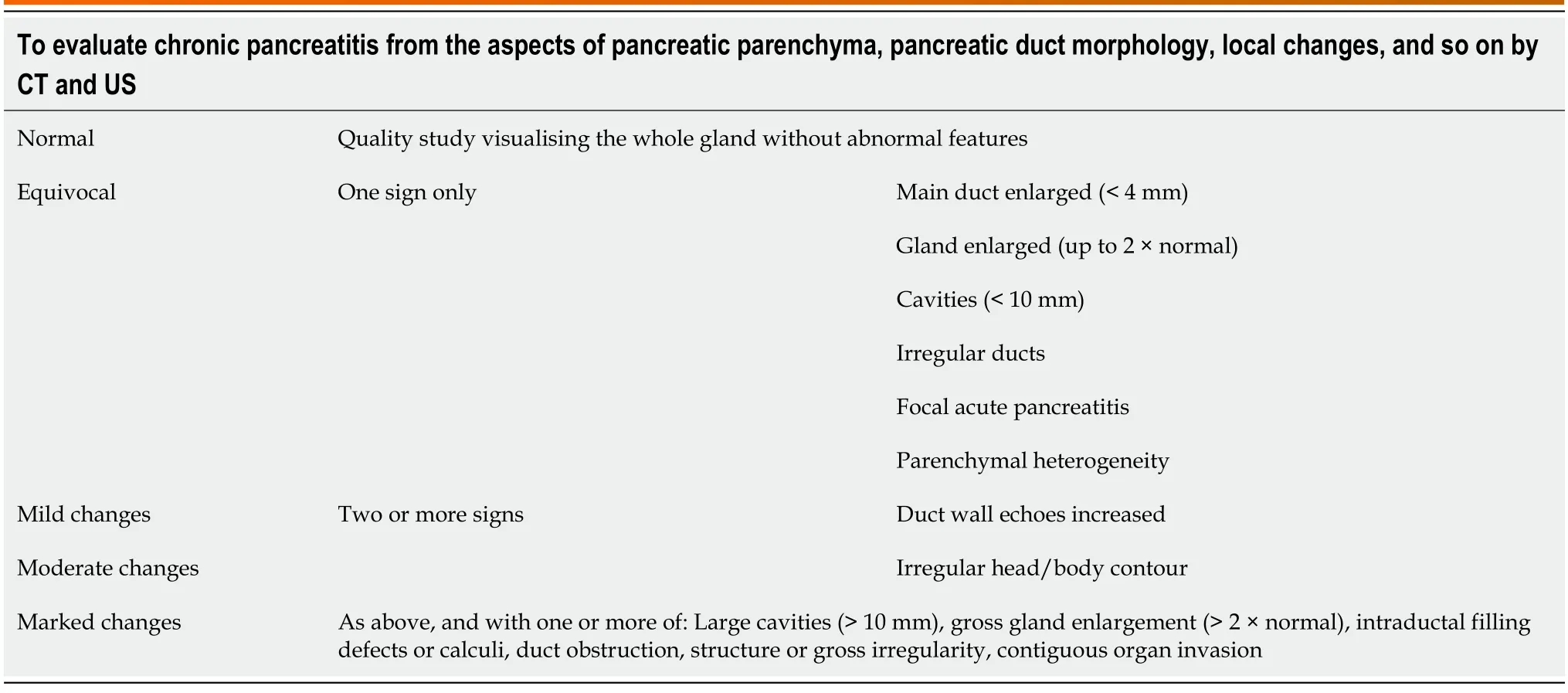
Table 2 Cambridge classification diagnostic criteria in chronic pancreatitis[27]
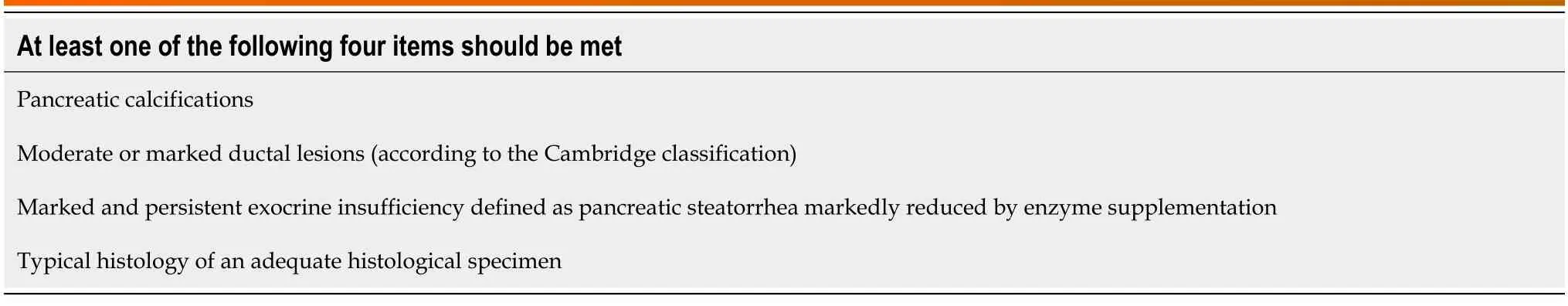
Table 3 M-Annheim diagnostic criteria of definite chronic pancreatitis[14]
The progression of CP can be divided into early and advanced stages.The early stage especially refers to the period before the development of morphological changes in the pancreas.Because the morphology of the pancreas is mostly normal at this time,it is difficult to diagnose by conventional imaging methods.In the advanced stage,the morphology of the pancreas changes,which often manifests as pancreatic atrophy,pancreatic parenchyma calcification,irregular dilatation and distortion of the pancreatic duct,intraductal calculi,etc.,and it can also be accompanied by complications,such as pseudocyst,common bile duct stricture,duodenal obstruction,etc.These manifestations can be detected by conventional radiological imaging (CT or MRI)[28].CT scan is easily available,noninvasive,and relatively cheaper compared to other modalities.MRI is superior to CT for the evaluation of pancreatic parenchymal and ductal changes,with better resolution than CT,but it is more expensive and requires more time.
Three common CT findings of CP are pancreatic ductal dilatation (68%;Figure 1A),parenchymal atrophy (54%;Figure 1B),and pancreatic calcification (50%;Figure 1B)[19].MRI shows pancreatic duct stones better than CT,while CT shows calcification better than MRI.
Figure 1 Chronic pancreatitis. A: Chronic pancreatitis with main pancreatic duct stone and main pancreatic duct dilatation.A 58-year-old man with chronic pancreatitis presented with no pain.The abdominal computed tomography (CT) scan represents the main pancreatic duct stone (orange arrow),the dilated main pancreatic duct (yellow arrows) with a diameter of 0.5 cm,as well as the combined gallbladder multiple stones (white arrow);B: Chronic pancreatitis with pancreatic parenchymal atrophy and multiple pancreatic calcifications.A 69-year-old man with chronic pancreatitis.The abdominal CT scan shows a decrease in pancreatic volume,parenchymal atrophy,and multiple calcifications in the pancreatic parenchyma (orange arrows).
In recent years,most of the literature and guidelines[29,30] emphasize the importance of early diagnosis of CP,and achieve the purpose of early detection and early diagnosis before irreversible changes in the pancreas,so as to avoid late complications and improve the prognosis and clinical outcomes of CP patients.
Early diagnosis of pancreatic fibrosis can provide a valuable opportunity to prevent disease progression[11].Khatkovet al[11] believed that multidetector CT (MDCT) can be used as a non-invasive diagnostic tool for detecting pancreatic fibrosis,and its post-processing indicators are related to the degree of pancreatic fibrosis,so it is expected to be used for early diagnosis of CP.The results of a study involving 74 patients showed that compared with mild pancreatic fibrosis,the normalized contrast enhancement ratio during the venous phases and the pancreatic late/early attenuation ratio increased in patients with severe pancreatic fibrosis,while the unenhanced pancreatic density decreased.Therefore,the application value of MDCT in the early diagnosis of CP is further verified.
A prospective study by Liuet al[31] showed that pancreatic stiffness and T1 relaxation time in multimodal functional MRI can be used as independent predictors of pancreatic fibrosis grading and showed significant associations with fibrosis extent.And substantial changes in mild CP can be detected by T1-mapping,which is manifested by a significant increase in the T1 relaxation time of pancreatic parenchyma in patients with mild CP[32].Therefore,T1-mapping can also be used as a new MRI technique to evaluate early CP.In addition,magnetic resonance elastography (MRE)-derived stiffness,which can be used to measure tissue mechanical properties and provide information on soft tissue stiffness in vivo,is the highest diagnostic indicator for detecting CP without secretory insufficiency (reflecting early CP),and there is no difference in the diagnostic effect between T1 relaxation time and MRE-derived stiffness[28].Furthermore,the research of Wanget al[33] showed that multitasking dynamic contrast enhanced MRI technology can not only achieve early detection and early diagnosis of CP because changes in microcirculation characteristics are usually preceded by morphological changes,but also it can identify and diagnose CP and pancreatic ductal adenocarcinoma by estimating microcirculation parameters (such as tissue plasma flow,fractional plasma volume,transfer constant,etc.).
THE RELATlONSHlP BETWEEN PAlN AND lMAGlNG FlNDlNGS OF CP
Before this,there were many studies on the correlation between the pain of CP and its imaging morphological manifestations,but they were scattered and not concentrated.On one hand,pain is the most common clinical manifestation of CP.On the other hand,CT/MRI is the most commonly used imaging examination for CP.There is no review to summarize the correlation and connection between the two.Here,it is summarized in the form of tables (Table 4) and text,in order to find something valuable.
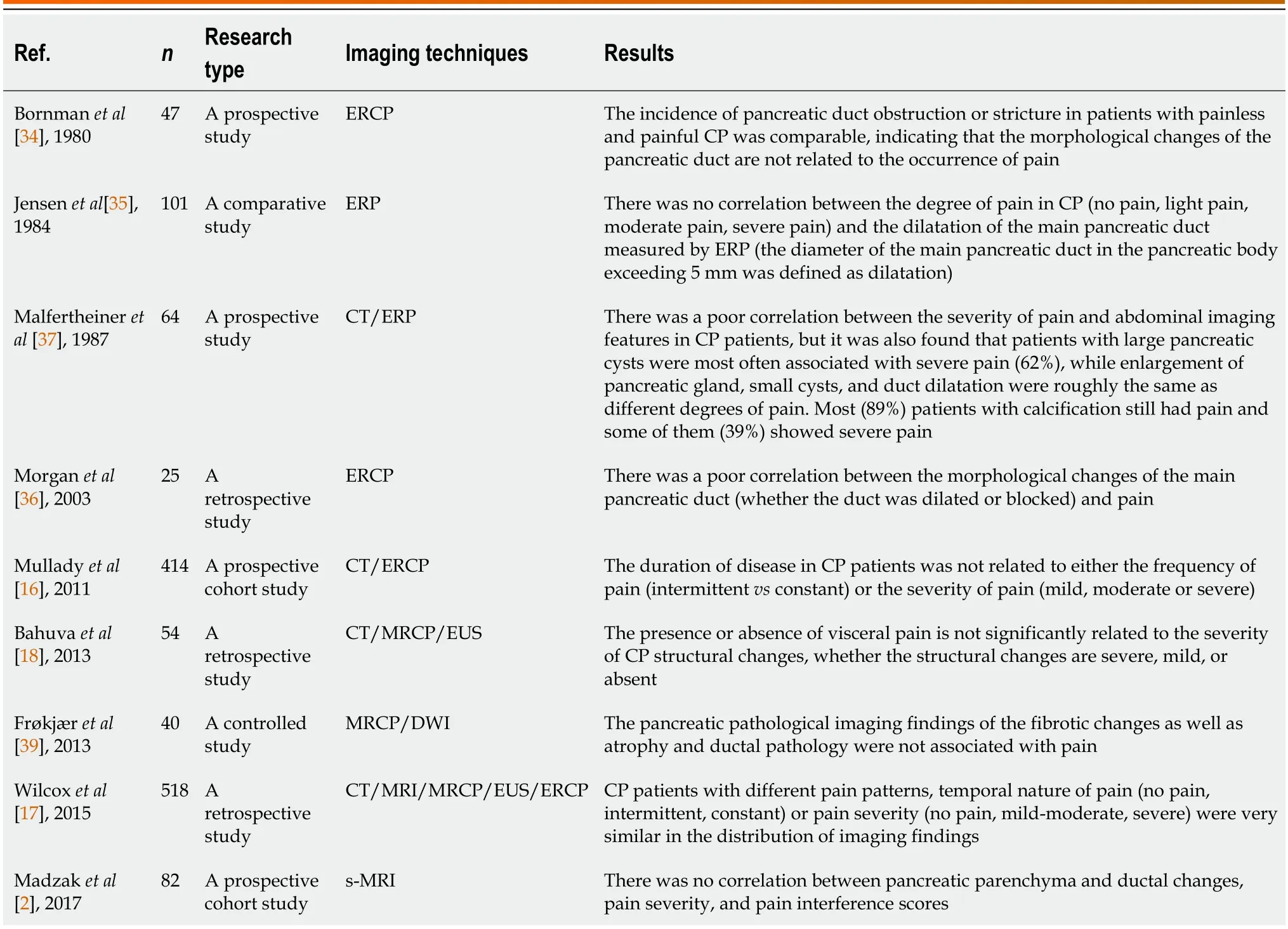
Table 4 The relationship between pain and imaging findings of chronic pancreatitis
It can be traced back to a study of 47 patients with CP by Bornmanet al[34] in 1980.The ERCP examination technique used in the study showed that the incidence of pancreatic duct obstruction or stricture was comparable between painless and painful CP patients,indicating that the morphological changes of the pancreatic duct were not related to the occurrence of pain.Along this line,it can be found in subsequent studies that Jensenet al[35] found there was no correlation between the expansion of the main pancreatic duct and the severity of pain in patients with CP in a comparative study of 101 patients.Similarly,Morganet al[36] also confirmed that in patients with CP,whether the main pancreatic duct was dilated or blocked,the pain performance was similar.Therefore,it is not hard to see that there is no significant correlation between the presence or severity of pain in CP patients and the morphological changes (dilatation or stricture) of the pancreatic duct.
In addition,further studies[18] also found that there was no significant correlation between the presence or absence of abdominal pain and the severity of CP morphological structural changes.A retrospective study of 518 CP patients was conducted by Wilcoxet al[17] using CT/MRI/MRCP and other imaging methods.It was found that CP patients with different pain patterns,temporal nature of pain (no pain,intermittent,constant),or severity of pain (no pain,mildmoderate,severe) were very similar in the distribution of imaging findings.
In summary,the severity and duration of abdominal pain symptoms caused by CP are not significantly correlated with the degree of damage to pancreatic anatomical structures (such as pancreatic parenchymal atrophy,pancreatic duct dilatation or stricture,and pancreatic parenchymal fibrosis).However,although the correlation between pain and imaging morphological changes is poor,some other meaningful things have been found.For example,CP patients with large pancreatic cysts are most often associated with severe pain (Figure 2) The correlation between pancreatic enlargement,small cysts duct dilatation,and different degrees of pain is roughly the same.Furthermore,the vast majority of patients with calcification still have pain,and some of them can be manifested as severe pain[37].
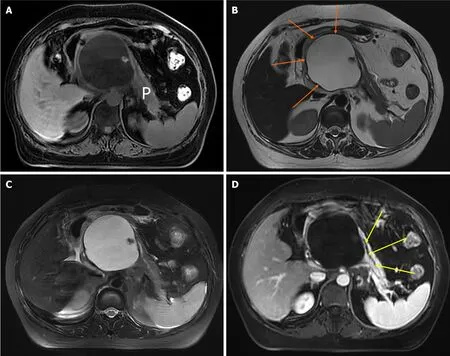
Figure 2 Chronic pancreatitis with large pancreatic cysts. A 52-year-old woman with chronic pancreatitis presented with upper abdominal pain.The upper abdominal magnetic resonance images.A: Magnetic resonance imaging (MRI) fat-suppressed T1-weighted imaging shows a large pseudocyst of the head of the pancreas,which has a low signal;B: MRI T2-weighted imaging can show a clear boundary of pseudocyst (orange arrows) with a diameter of 7 cm × 11 cm,which has a high signal;C: MRI fat-suppressed T2-weighted imaging;D: MRI enhanced scanning venous phase shows the large pseudocyst has no enhancement as well as the displaced main pancreatic duct (yellow arrows).P: Pancreas.
Moreover,it was found that the duration of disease in CP patients was not related to either the frequency of pain (intermittentvsconstant) or the severity of pain (mild,moderate,or severe)[16].Combined with CP-induced pancreatic neural alterations,such as intrapancreatic nerves increase in size (neural hypertrophy) and number (increased neural density),related studies have shown that these neural alterations are related to the severity of neuropathic pain.Therefore,the neural alterations of CP are active shapers of disease evolution and progression[38].This means that a series of pancreatic morphological imaging findings (such as parenchymal atrophy and pancreatic duct dilatation) with the progression of CP may not be related to the severity of pain in patients,and the presence or absence of visceral pain has nothing to do with the severity of CP because most of the pain drivers of advanced CP are neurological rather than pancreatic.Therefore,it is not difficult to explain why the correlation between pain symptoms and imaging findings is poor[18,39].
CONCLUSlON
In summary,CP is a fibroinflammatory syndrome caused by a variety of causes.The most common clinical manifestation is abdominal pain and the mechanism of abdominal pain is not fully understood.CT/MRI is usually used as the first-line imaging diagnosis of CP.The duration and severity of abdominal pain caused by CP are poorly correlated with pancreatic imaging morphological changes.There is a correlation between pain caused by CP and neural alterations and related complications.Therefore,the next research should further explore the relationship between neural alterations or related complications caused by CP and pain,in order to have a deeper understanding of CP.
FOOTNOTES
Author contributions:Feng Y,Song LJ and Xiao B designed the research study;Feng Y,Song LJ and Xiao B analyzed the data and wrote the manuscript;All authors have read and approved the final manuscript.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Ling-Ji Song 0000-0003-4508-9654;Bo Xiao 0000-0001-5862-974X.
S-Editor:Li L
L-Editor:A
P-Editor:Zhao S
 World Journal of Radiology2024年3期
World Journal of Radiology2024年3期
- World Journal of Radiology的其它文章
- Artificial intelligence for disease diagnostics still has a long way to go
- Ductal carcinoma in situ within a fibroadenoma: A case report and review of literature
- Evaluating pediatric ureteropelvic junction obstruction: Dynamic magnetic resonance urography vs renal scintigraphy 99mtechnetium mercaptoacetyltriglycine
