Distribution of pathogenic bacteria and antimicrobial sensitivity of eye infections in Suzhou
Li Zhang, Hai-Zhang You, Guo-Hui Wang, Wei Xu, Jian-Shan Li, Qing-Liang Zhao,Shu Du
1Department of Hospital-Acquired Infection Control, Lixiang Eye Hospital of Soochow University, Suzhou 215021, Jiangsu Province, China
2Department of Administrative Office, Lixiang Eye Hospital of Soochow University, Suzhou 215021, Jiangsu Province, China
3Department of Clinical Laboratory, Lixiang Eye Hospital of Soochow University, Suzhou 215021, Jiangsu Province, China
4Department of Pharmacy, Lixiang Eye Hospital of Soochow University, Suzhou 215021, Jiangsu Province, China
5Department of Corneal and Lacrimal Passage, Lixiang Eye Hospital of Soochow University, Suzhou 215021, Jiangsu Province, China
6Department of Fundus Diseases and Ocular Trauma, Lixiang Eye Hospital of Soochow University, Suzhou 215021, Jiangsu Province, China
Abstract
· KEYWORDS: eye infection; pathogenic bacteria; drug resistance; antimicrobial sensitivity test
INTRODUCTION
Eye infections refer to common and frequently-occurring ophthalmic diseases caused by various bacterial infections, which are generally caused by pathogenic factors such as bacteria, fungi and viruses, of which bacterial infections are the most common[1-2].Eye infections have a close bearing on various risk factors, such as trauma, surgery,contact lens wearing, age, dry eye, chronic nasolacrimal duct obstruction, and previous eye infections[3-4], with varying degrees of prognosis, and in severe cases, can be visionthreatening[5].With keratitis and conjunctivitis as the two most common types of infections[6-7], eye infections can damage patients’ eye tissues, resulting in decreased vision and, in severe cases, corneal perforation and eyeball atrophy[8], which can seriously affect patients’ normal life and even lead to blindness[9-10].
Despite the natural resistance of human corneas to infection,factors such as trauma, corneal surgery, contact lens wearing[11], ocular surface diseases[12], systemic diseases[13],and immunosuppression can alter the defense mechanisms of the ocular surface, resulting in bacterial invasion of the cornea.If left undiagnosed and untreated, keratitis may develop into endophthalmitis[14], a serious eye infection caused by bacteria and other microorganisms entering the vitreous body.In a study by Wanet al[15], the etiological characteristics of 531 cases of suppurative endophthalmitis in Qingdao Eye Hospital of Shandong Eye Institute from January 2006 to December 2015 were retrospectively analyzed.A total of 224 strains of pathogenic bacteria were obtained in culture, of which gram-positive bacteria (54%) were predominant, withStaphylococcus epidermidis(25%) being the most common,followed by fungi (29.5%) and gram-negative bacteria (16.5%).Bacterial conjunctivitis, which accounts for about 50%-70%of infectious conjunctivitis[16], affects not only the conjunctiva but also adjacent tissue structures and is a potential risk factor for other intraocular or extraocular infections[17].About 90%of individuals can isolate bacteria from conjunctival sac,includingStaphylococcus epidermidis,Diphtheroid bacillusandPropionibacterium acnes, which deter other pathogenic bacteria from attacking by releasing antibiotic-like substances and metabolites.Infection occurs in a situation where the defenses of the host are weaker than the invasion ability of pathogenic bacteria[18].Yanget al[19]reportedStreptococcus pneumoniae,Haemophilus influenzaeandStaphylococcus aureusas common causative agents of acute bacterial conjunctivitis, whose incubation period and duration of infection depends on the organismal status of the infected person, with infection latency and duration depending on the organism status of the infected person.
Socioeconomic development and environmental changes have witnessed an upward trend in the incidence of eye infections[20-22].Eye infections are generally treated with antibacterial drugs, but their types and biological characteristics are constantly changing with the widespread use of antibacterial drugs and the popularity of contact lenses.Accordingly, the therapeutic effect of antibacterial drugs on bacterial infections and bacterial resistance are constantly changing as well[23].Given the increased difficulty in the treatment and diagnosis of bacterial eye infection, treatment with effective antimicrobial drugs at an early stage of eye infection is of great importance for the preservation and restoration of visual function in patients[24-25].For a better treatment of patients with ocular bacterial infections, a periodic summary evaluation of eye pathogenic bacterial resistance is needed to provide a scientific basis for the diagnosis of eye infections and the use of antimicrobial drugs.In this study, 155 patients admitted to Lixiang Eye Hospital of Soochow University from January 2020 to March 2023 were retrospectively collected, and their clinical data were retrospectively analyzed to figure out the types, composition and drug resistance of bacterial infections, so as to provide a basis for the rational use of antibacterial drugs in clinic.
SUBJECTS AND METHODS
Ethical ApprovalThis study was conducted in accordance with the Declaration of Helsinki and approved by the Research Ethics Committee of Lixiang Eye Hospital of Soochow University (ethical batch number: SLER2023101), and informed consent was obtained from all participants and their guardians.All methods were carried out in accordance with relevant guidelines and regulations.
SubjectsThe clinical data of 155 patients admitted to Lixiang Eye Hospital of Soochow University in Suzhou from January 2020 to March 2023 were retrospectively collected, including corneal specimens (108 cases), lacrimal sac specimens(20 cases), aqueous humor or vitreous body (17 cases)and other parts (10 cases).Inclusion criteria: 1) clinically diagnosed diseases such as keratitis, eyelid/orbital cellulitis,endophthalmitis, lacrimal gland and lacrimal duct infection;2) clinical microbial culture specimens of conjunctival sac secretions, lacrimal passage specimens, conjunctival/corneal scrapings, aqueous humor, vitreous body, foreign bodies caused by ocular trauma and ocular pathological tissues.Exclusion criteria: 1) non-ocular infectious diseases; 2) microbial culture specimens that are non-ocular biological specimens, such as urine and sputum; 3) duplicate strains isolated from the same part of the same case and suspected contaminated strains.Specimens were collected in strict accordance with the aseptic operating procedures and sent to the microbiology laboratory of the Department of Laboratory Medicine for isolation and identification.
Specimen CollectionConjunctival sac specimens were collected as follows: the patient was placed in a sitting position and instructed to gaze upward and turn the lower eyelid.A saline-soaked cotton swab was then used to gently wipe the conjunctival sac of the lower lid, including the medial canthus.After sampling, bacterial culture was performed.Corneal specimens were collected as follows: the patient was placed in the lying position, and after surface anesthesia, necrotic tissue was first scraped from the surface of the corneal ulcer under the microscope to expose the corneal lesion.Then, as much of the corneal tissue as possible was scraped with an ophthalmic scalpel and cultured with bacteria.Eyelid margin specimens were collected as follows: the patient was placed in a sitting position, a hot compress was applied and a lid gland massage was performed.Subsequently, a saline-soaked cotton swab was used to gently wipe the lipid secretions draining from the lid gland and cultured with bacteria.Specimens of aqueous humor, vitreous body, lacrimal passage and orbital contents were all taken intraoperatively.
Strain Identification and Antimicrobial Sensitivity TestBacterial culture identification was performed in strict accordance with the routine clinical microbiology identification procedures.Specimens were inoculated into bacterial culture medium, fungal culture medium and enrichment culture medium for culture and separation, and then single colonies were selected and identified by Hunan Mindray TDR-300B PLUS microbial identification instrument.The operation of the antimicrobial sensitivity test and the interpretation of the results were carried out in strict accordance with the M100-S20 rules and standards of the Clinical and Laboratory Standards Institute (CLSI)[26].The antimicrobial sensitivity test was carried out using the “broth microdilution method”recommended by CLSI to detect the susceptibility and MIC values of the drugs separately.After processing by intelligent expert analysis software, the report results were obtained and reasonable expert evaluation was put forward.The quality control strains wereStaphylococcus aureus(ATCC25923),Enterococcus faecalis(ATCC29212),Escherichia coli(ATCC25922) andPseudomonas aeruginosa(ATCC27853).Statistical AnalysisAll data in this study were statistically analyzed using SPSS 23.0 software.χ2test was utilized to compare categorical variables, withP<0.05 indicating a statistically significant difference.
RESULTS
Distribution Results of Pathogenic BacteriaAmong the patients with positive bacterial culture, 84 were male and 71 were female, with a ratio of 1.18:1 and a mean age of 49.65±22.21y.Of the 155 strains of pathogenic bacteria,gram-positive bacteria predominated at 45.81%, followed by fungi at 39.35%, and gram-negative bacteria accounted for the lowest percentage of 14.84%.Staphylococcus epidermidisandStreptococcus pneumoniaeaccounted for the top two gram-positive bacteria infections with 38.06%and 1.94%, respectively.Pseudomonas aeruginosa(6.45%)andStenotrophomonas maltophilia(1.94%) were the top two pathogens accounting for the gram-negative bacteria infections, respectively.Mucor(20%) andFusarium(15.48%)were the top two pathogens in fungi (Table 1).
Analysis of Specimen Collection Sites and Positive Culture of SpecimensThe distribution of bacterial infections in different parts of the eye from January 2020 to March 2023(Table 2).Staphylococcus epidermidiswas the most common strain in the conjunctiva, cornea, aqueous humor or vitreous body and other eye parts.Besides,FusariumandPseudomonas aeruginosawere also among the most common strains of conjunctival and corneal infections.
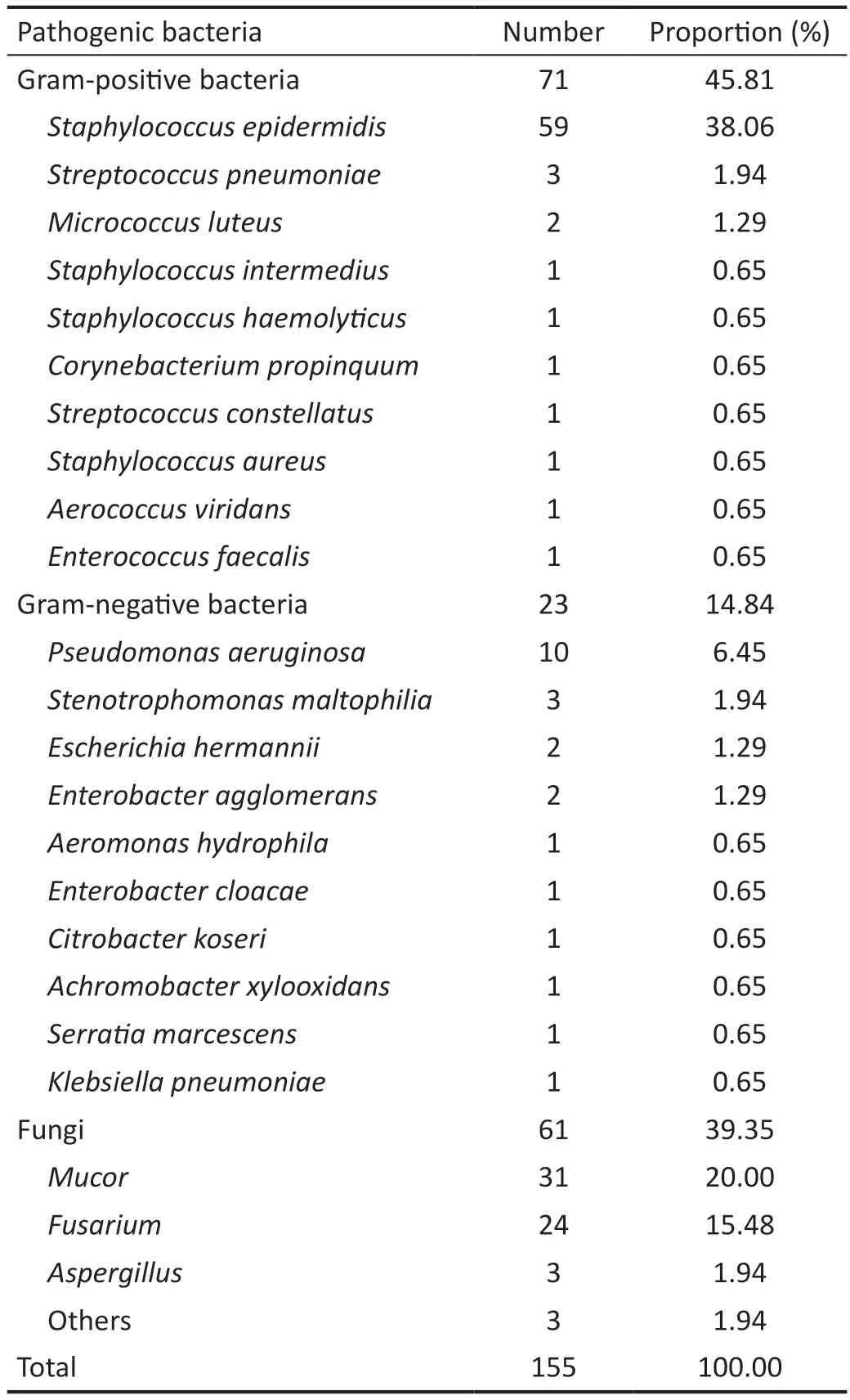
Table 1 Distribution and composition ratio of pathogenic bacteria in patients with eye infections
Drug Resistance of Bacterial StrainsThe results of the antimicrobial sensitivity test showed that gram-positive bacteria were highly resistant to penicillin and erythromycin(78.87% and 46.48% respectively), but least resistant to vancomycin at 0.Gram-negative bacteria were highly resistant to cefoxitin and compound sulfamethoxazole (100% and 95.65% respectively), but least resistant to meropenem at 0 (Table 3).Further comparison of the resistance of gramnegative bacteria and gram-positive bacteria to various drugs revealed statistically significant differences (P<0.05) in the resistance of both to cefoxitin, cotrimoxazole, levofloxacin,cefuroxime, ceftriaxone and ceftazidime, and both had higher rates of resistance to gram-negative bacteria than to grampositive bacteria (Table 4).

Table 2 Distribution of bacterial infections in different parts of the eye
DISCUSSION
The eyes, as a vital visual structure in people’s lives, are the basis for normal visual function in a healthy state.Infections in ophthalmic patients may easily cause vision loss and affectthe effectiveness of treatment.Therefore, in case of persistent ocular discomfort, medical attention should be sought as soon as possible and ophthalmic antimicrobial drugs should be used appropriately to treat infectious ophthalmic diseases thoroughly and effectively and to improve their treatment outcome[27-29].Farmers, construction workers and other groups are more prone to infection among the many people with eye infections because of their frequent farming and labor.Specifically,farmers are easily scratched by plants and splashed with seeds during labor, which leads to fungal infection; Construction workers are more likely to be infected with gram-positive bacteria because they are often hooked by wires or hit by stones.For this reason, protective eyewear should be used properly during labor to reduce the incidence of eye infections.Supplemented by the increasing use of electronic products in the context of the rapid changes in technology, eye fatigue and reduced eye immunity are becoming more common,eventually leading to eye infections.Meanwhile, people’s pursuit of beauty has improved under the rising standard of living, contributing to a rapid increase in the use of contacts lenses and cosmetic contact lenses.But with this comes their unregulated use, causing adverse eye consequences such as eye dryness, fatigue and discomfort, and eye infections[30].
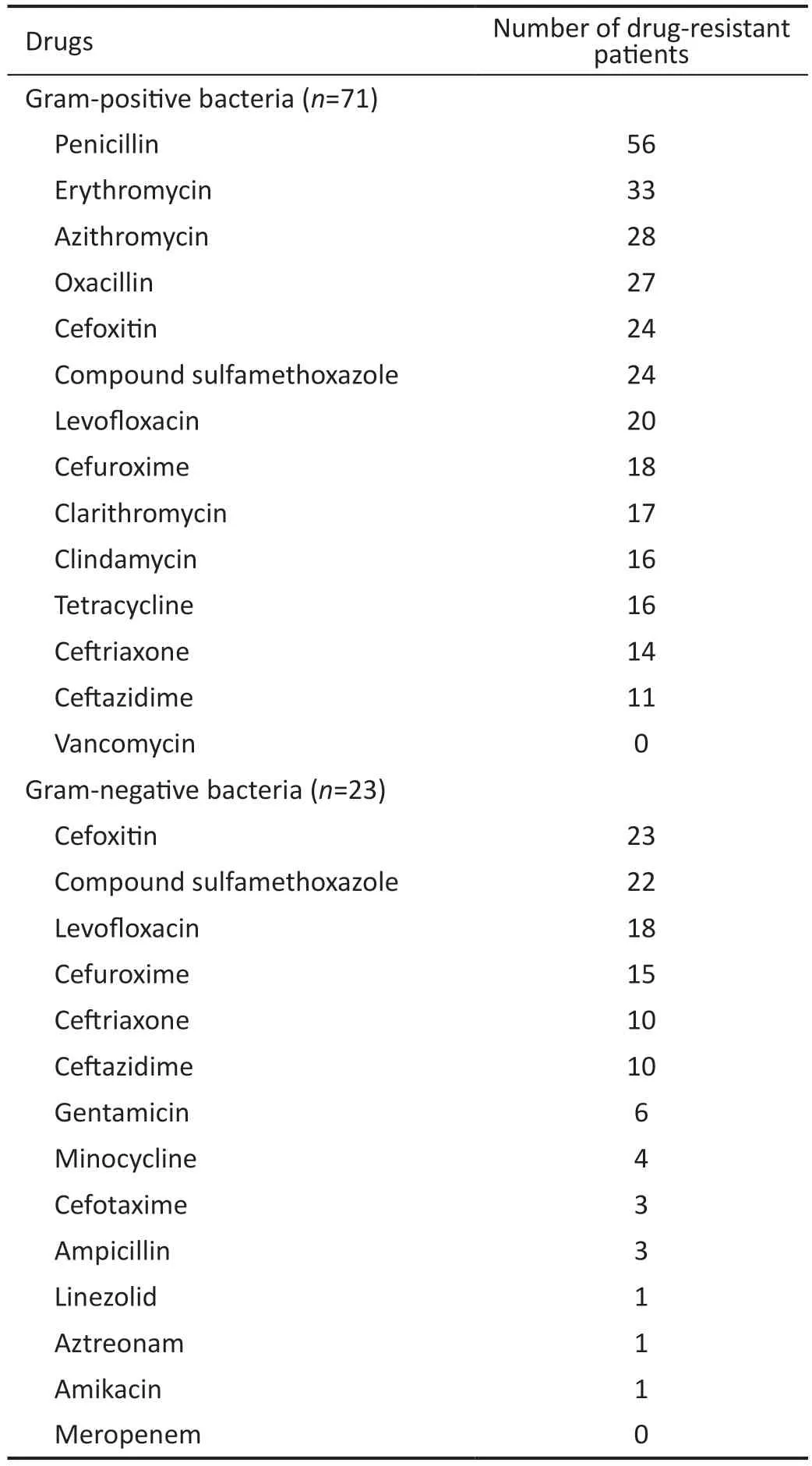
Table 3 Drug resistance of bacterial strains

Table 4 Comparison of resistance of gram-positive and gram-negative bacteria to some drugs
Bacterial infections, as the most common pathogenic bacteria in eye infections, are constantly changing due to the continuous application and even abuse of antimicrobial drugs and hormones, resulting in changing drug resistance as well[31].Early identification of pathogenic bacteria species as well as a timely and accurate selection of antimicrobial drugs are key to treating patients with eye infections[32-33].In this study, the clinical data of 155 patients admitted to Lixiang Eye Hospital of Soochow University in Suzhou from January 2020 to March 2023 were retrospectively collected, and the pathogenic bacteria species and drug resistance of each pathogenic bacteria were analyzed.The results showed that the pathogens infecting patients with eye infections were mainly gram-positive bacteria, followed by fungi and gram-negative bacteria.The main gram-positive bacteria wereStaphylococcus epidermidis(45.04%) andStreptococcus pneumoniae(2.29%), whereas the main gram-negative bacteria werePseudomonas aeruginosa(7.63%) andStenotrophomonas maltophilia(2.29%), which was consistent with the predominance of gram-positive bacteria in eye infections reported in related studies[34].The analysis of the infected site shows that the most infected site was the conjunctiva (50.38%), followed by the cornea (31.30%)and finally the aqueous humor or vitreous body (9.92%).
In previous reports, no bacteria isolated from all types of eye infections were found to be resistant to vancomycin and the sensitivity of the drug was definitive[35-36].Comparison of the resistance of gram-positive and gram-negative bacteria to some drugs revealed that gram-positive bacteria were highly resistant to penicillin and erythromycin (78.87% and 46.48% respectively), but least resistant to vancomycin at 0 and that gram-negative bacteria were highly resistant to cefoxitin and compound sulfamethoxazole (100% and 95.65%respectively), but least resistant to meropenem at 0.Therefore,patients diagnosed with gram-positive bacteria can be treated with vancomycin, and treatment with ceftazidime is equally effective; while those diagnosed with gram-negative bacteria are recommended to be treated with meropenem, amikacin,and aztreonam.Further comparison of the resistance of grampositive bacteria and gram-negative bacteria to some drugs revealed statistically significant differences (P<0.05) in the resistance of both to cefoxitin, compound sulfamethoxazole,levofloxacin, cefuroxime, ceftriaxone and ceftazidime, and both had higher rates of resistance to gram-negative bacteria than to gram-positive bacteria.This suggests that the above drugs are less effective in gram-negative bacterial infections,and can be used in those with gram-positive bacterial infections.Considering that the resistance of pathogenic bacteria may be attributed to improper or abusive use of previous antimicrobial drugs, there is a need to improve the norms and systems of drug use in the hospital and to provide targeted treatment for postoperative patients with different pathogenic bacterial infections, so as to achieve the best therapeutic effect[37].
Based on the results of this study, ophthalmologists may make more appropriate decisions in the treatment of eye-bacterial infections.Nevertheless, certain limitations are also visible in the present study.First, this study was a single-center study with accidental results, which led to differences in the distribution of pathogenic bacteria in this paper compared with other literature.Second, a small sample size was included in this study, resulting in low test efficiency and incomplete results.Therefore, the sample size should be further increased in subsequent studies.Finally, the retrospective approach to the study and the time available for the study are limited due to the nature of the methods, which limits our ability to perform a more objective analysis of trends in pathogen distribution and antibiotic sensitivity.To address this, studies of eye bacterial infections with larger sample sizes, longer duration, and using more advanced technology will be conducted in the future.
To put it in a nutshell,Staphylococcus epidermidisis the main isolated strain of all eye bacterial specimens in Suzhou,China.Antibiotics such as penicillin and erythromycin, used for the treatment of gram-positive bacterial infections, are less effective, and vancomycin is the best, followed by ceftazidime.Cefoxitin and compound sulfamethoxazole are less effective in the treatment of gram-negative bacterial infections, so meropenem is recommended.By further classifying bacteria and comparing their sensitivity to antibiotics through statistical analysis, more accurate results of antibiotic sensitivity analysis can be obtained.
ACKNOWLEDGEMENTS
Conflicts of Interest: Zhang L,None;You HZ,None;Wang GH,None;Xu W,None;Li JS,None;Zhao QL,None;Du S,None.
 International Journal of Ophthalmology2024年4期
International Journal of Ophthalmology2024年4期
- International Journal of Ophthalmology的其它文章
- Comment on: Recurrence after spontaneous separation of epiretinal membrane in a young woman: a case report
- When to repair a retinal detachment?
- Bilateral iridocorneal endothelial syndrome-Chandler’s syndrome: a case report and literature review
- Penetrating canaloplasty in corticosteroid-induced glaucoma: a report of two cases
- On-spot preparation of EDTA solution for the treatment of band keratopathy: a case report
- Non-contact wide-field viewing system-assisted scleral buckling surgery for retinal detachment in silicone oilfilled eyes
