Comparison of macular changes according to the etiology of optic neuritis: a cross-sectional study
Yeji Moon, Sung-Min Kim, Jae Ho Jung
1Department of Ophthalmology, Asan Medical Center,University of Ulsan College of Medicine, Seoul 05505,Republic of Korea
2Department of Neurology, Seoul National University Hospital,Seoul 03080, Republic of Korea
3Department of Ophthalmology, Seoul National University Hospital, Seoul 03080, Republic of Korea
4Department of Ophthalmology, Seoul National University College of Medicine, Seoul 03080, Republic of Korea
Abstract
· KEYWORDS: foveal thickness; optic neuritis;aquaporin-4 immunoglobulin; myelin oligodendrocyte glycoprotein; multiple sclerosis
INTRODUCTION
Optic neuritis (ON) is an inflammatory demyelinating disease of the optic nerve.Although most patients recover visual function within six to eight weeks of the onset of acute ON as shown in the Optic Neuritis Treatment Trial(ONTT)[1], structural changes such as optic disc pallor and atrophy of the retinal nerve fiber layer (RNFL) remain as footprints of inflammation.
Optical coherence tomography (OCT) non-invasively provides high-resolutionin vivoimages of the optic disc and retina[2].Since the first report on the role of OCT in the study and treatment of ON was published in 1999[3], many studies have evaluated post-ON structural change using OCT, which has shown pathological changes in the visual system more clearly than ever before.Most of those studies focused on changes in RNFL and ganglion cell-inner plexiform layer (GCIPL)thicknesses[4-8].In fact, RNFL and GCIPL analyses performed using OCT have helped to characterize ON according to the etiology, such as aquaporin-4 (AQP4) immunoglobulin G (IgG)-related ON (AQP4-ON), myelin oligodendrocyte glycoprotein (MOG) IgG-related ON (MOG-ON), and multiple sclerosis (MS)-related ON (MS-ON)[9-17].Meanwhile, several recent studies have measured retinal layers other than the RNFL and GCIPL to evaluate retinal damage independently of ON-caused neuroaxonal damage.In particular, foveal changes have been reported in patients with AQP4-IgG-positive neuromyelitis optica spectrum disorder(NMOSD), which suggests Müller cell dysfunction[18-23].Meanwhile, the studies on retinal changes in patients with MOG-ON or MS-ON have been limited to changes of RNFL and/or GCIPL thickness.Moreover, little is known about the clinical implications of changes to retinal layers other than the RNFL and GCIPL, mainly because the association between foveal changes and post-ON visual function has not yet been clearly revealed.
Therefore, in this study, we aimed to compare the macular structure, including foveal thickness, among ON patients according to the etiology.Further, we investigated the possible correlation between structural changes in the macula and visual outcomes among the different etiologies.
SUBJECTS AND METHODS
Ethical ApprovalThe study was approved by the Institutional Review Board of Seoul National University Hospital (IRB No.2104-114-1212) and followed the tenets of the Declaration of Helsinki.The requirement for informed consent was waived due to the retrospective study design.
Study PopulationThis retrospective cohort study included patients aged 15y or more who had been diagnosed with ON at Seoul National University Hospital.The diagnosis of ON was based on the ONTT guidelines[1].Serum samples were obtained at the time of an acute attack and tested for the presence of AQP4 and MOG antibodies using a cellbased assay, as reported[24-25].On that basis, the patients were classified into three groups according to the following criteria:1) AQP4-IgG-related ON group (AQP4 group): patients who were AQP4-IgG seropositive and MOG-IgG seronegative; 2)MOG-IgG-related ON group (MOG group): patients who were AQP4-IgG seronegative and MOG-IgG seropositive; 3) MSrelated ON group (MS group): patients who were AQP4-IgG and MOG-IgG seronegative and had been diagnosed with MS according to the McDonald criteria[26].
In the acute stage, the patients were given intravenous methylprednisolone (IVMP) 250 mg every 6h for 3 or 5d.Subsequently, oral prednisone was administered and tapered at the clinician’s discretion.Plasmapheresis treatment was performed when severe visual dysfunction continued or worsened after IVMP therapy.
The present study’s exclusion criteria were as follows: 1)incomplete data on serological status for AQP4-IgG or MOG-IgG; 2) both AQP4-IgG and MOG-IgG seropositivity(double-positivity) for ON; 3) both AQP4-IgG and MOGIgG seronegativity (double-negativity) and failure to meet the diagnostic criteria for MS (idiopathic ON or clinically isolated syndrome); 4) systemic or other ophthalmological diseases possibly affecting visual function or OCT results.
For the patients with simultaneous or sequential bilateral ON,only the eye with the more severe visual dysfunction was selected for the final analysis, so as to eliminate any withinsubject factors.
Neuro-ophthalmology ExaminationsWe reviewed the patients’ medical records for basic demographic data and the results of prior ophthalmological examinations.We collected data on final-visit neuro-ophthalmology examinations for each of the patients.To eliminate the effect of acute inflammation,we included the data from the examination performed at least 6mo after the onset of ON.
As for visual outcomes, we obtained data from visual acuity(VA) and visual field (VF) tests.VA was converted into logarithm of minimum angle of resolution (logMAR) for the analysis.Poor vision, classified as count finger (CF), hand motion (HM), light perception (LP), and no light perception(NLP), was converted to logMAR 1.7, 2.0, 2.3, and 3.0,respectively[27].The VF test was conducted using Humphrey perimetry Swedish Interactive Threshold Algorithm 24-2 (Carl Zeiss Meditec, Inc., Dublin, CA, USA).Visual field index(VFI) and mean deviation (MD) measurements were used in the final analysis.
OCT scanning was performed using spectral-domain OCT(Cirrus HD OCT, Carl Zeiss Meditec, Inc).Images of signal strength ≥6 were accepted, and the quality of each image and segmentation of the retinal layers were manually checked by a single clinician (Moon Y).Average RNFL and GCIPL thicknesses were automatically measured based on,respectively, the optic disc cube 200×200 protocol covering a 6 mm×6 mm area centered on the optic disc and the macular cube 200×200 protocol covering a 6 mm×6 mm area centered on the fovea.Average GCIPL thickness was measured within a fovea-centered annulus area of 1.0 mm×1.2 mm inner diameter and 4.0 mm×4.8 mm outer diameter.We additionally obtained,by the macular cube protocol, retinal thickness from the inner limiting membrane (ILM) to the retinal pigment epithelium(RPE) for the following 9 sectors of the macula: superior,nasal, inferior, and temporal perifoveal retina; superior, nasal,inferior, and temporal parafoveal retina, and fovea.These 9 regions were defined according to the ETDRS map with its 3 concentric rings 1, 3, and 6 mm centered on the fovea.
Statistical AnalysisContinuous data were recorded as mean±standard deviations, while categorical data were obtained in proportions and percentages.Clinical characteristics were compared among the three groups using the analysis of variance(ANOVA) and Bonferroni post hoc tests.Any correlation between structural and visual outcomes was evaluated usingSpearman’s rank correlation coefficient.All of the statistical analyses were performed using SPSS version 23.0 (SPSS, Inc.,Chicago, IL, USA).
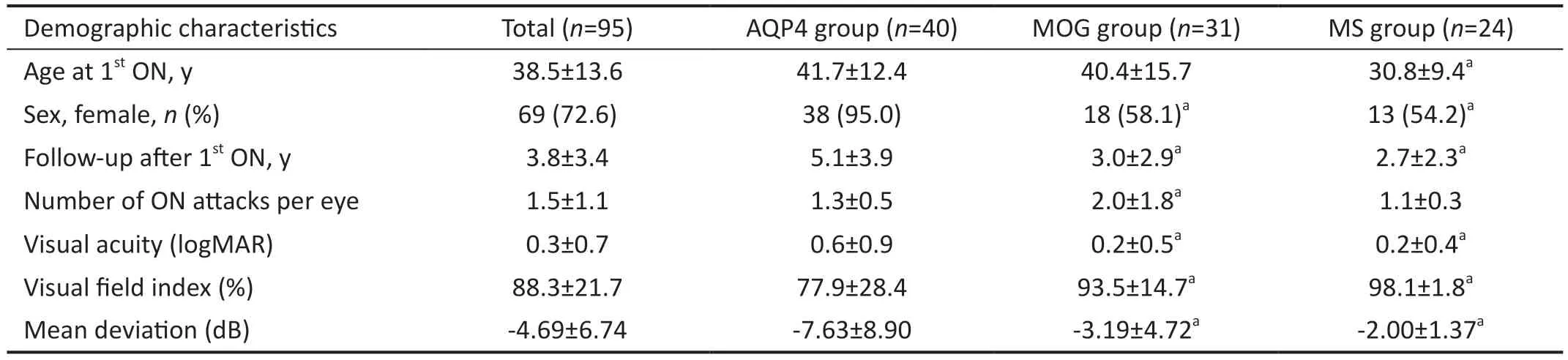
Table 1 Baseline demographic and clinical data on the study population mean±SD
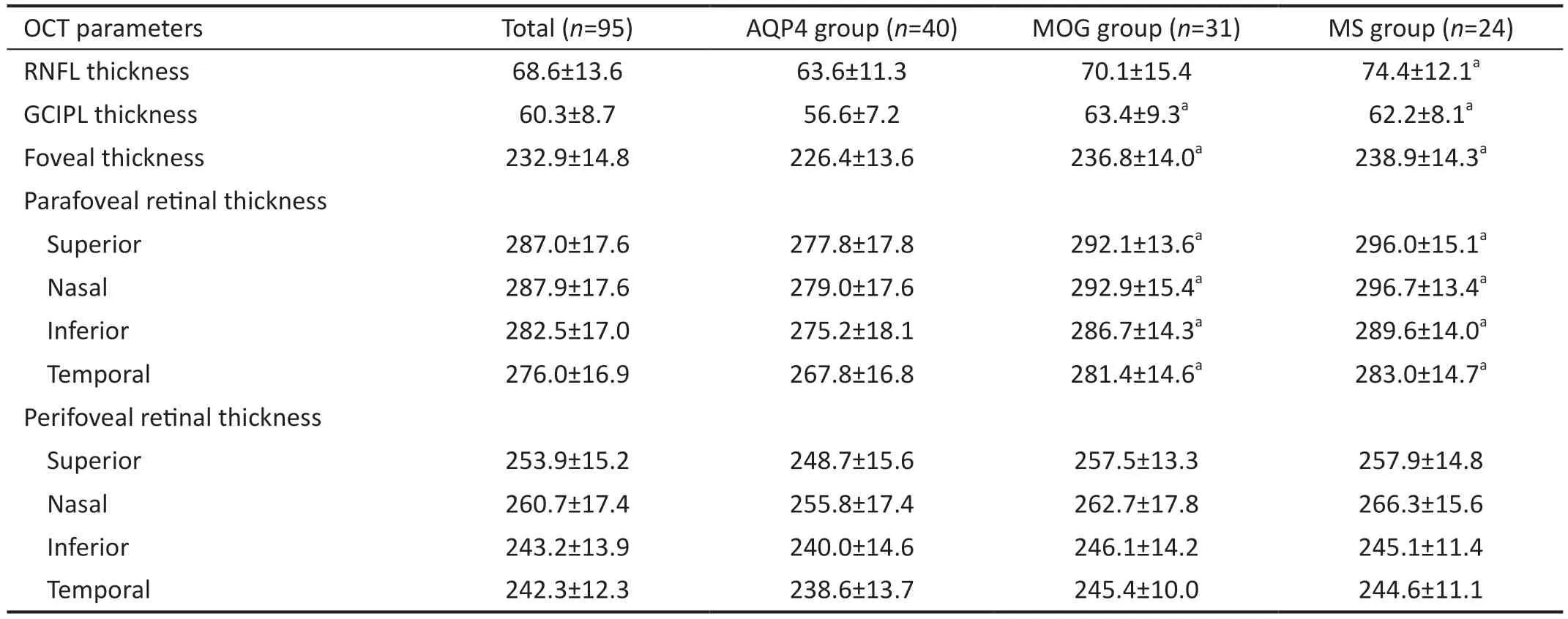
Table 2 Comparison of structural changes among the AQP4, MOG, and MS groups mean±SD, μm
RESULTS
The total study population consisted of 95 eyes of 95 patients:40 eyes in the AQP4 group, 31 eyes in the MOG group,and 24 eyes in the MS group.The baseline demographics and clinical information of the patients are summarized in Table 1.The mean age at first ON onset was 38.5±13.6y, and 72.6% of patients were female.During an average 3.8±3.4-year follow-up period, the mean number of attacks per eye was 1.5±1.1.The MS group was younger than the other two groups at the first attack of ON.The AQP4 group showed strong female predominance compared with the MOG and MS groups.The mean number of attacks during the followup period was 2.0±1.8 per eye in the MOG group, which was significantly larger than those in the AQP4 and MS groups.Visual outcomes, which were measured as VA, VFI and MD,were poorer in the AQP4 group than in the MOG and MS groups.However, there was no significant difference in visual outcomes between the MOG and MS groups.
Accordingly, structural damage was more severe in the AQP4 group.The mean RNFL thickness was 63.6±11.3, 70.1±15.4,and 74.4±12.1 μm in the AQP4, MOG, and MS groups,respectively.The average RNFL thickness was significantly thinner in the AQP4 group than in the MS group (P=0.005);however, the difference between the AQP4 and MOG groups was not statistically significant (P=0.102).The mean GCIPL thickness in the AQP4 group was 56.6±7.2 μm, which was significantly thinner than in either the MOG group (63.4±9.3 μm,P=0.003) and the MS group (62.2±8.1 μm,P=0.035; Table 2).In the comparison of macular thickness, the AQP4 group showed significantly severe damage in the fovea and parafoveal regions relative to the other two groups.However,the retinal thickness in the perifoveal area was not significantly different among the three groups (Table 2).
We next investigated the possible correlation between structural changes and visual outcomes for each group(Table 3).In the AQP4 group, RNFL and GCIPL thicknesses were both correlated with all of the measurement of the visual outcomes, namely VA, VFI, and MD.Additionally, foveal thickness was negatively correlated with VA as measured bylogMAR; the thinner the foveal thickness was, the worse was VA.However, foveal thickness was not associated with VFI or MD.Parafoveal and perifoveal retinal thicknesses also were negatively correlated with VA, not VFI or MD.In the MOG group, the thicknesses of the parafoveal and perifoveal retinas as well as the thicknesses of the RNFL and GCIPL showed significant correlations with all of the visual outcomes.Foveal thickness, though, was not correlated with any of the visual outcomes.In the MS group, RNFL thickness was not correlated with visual outcomes, while GCIPL thickness was associated with VA.The parafoveal and perifoveal retinal thicknesses,except for the nasal parafoveal area, were significantly correlated with VA.However, there was no significant correlation between foveal thickness and visual outcomes.

Table 3 Correlation between structural changes and visual outcomes after optic neuritis Correlation coefficient (P)
Case PresentationFigure 1highlights the significance of foveal thickness as a potential predictor of VA in the AQP4 group.Two cases of APQ4-ON presenting similar degrees of RNFL and GCIPL loss at the final visit demonstrated the VA dependence on foveal thickness.Case 1 (24.7y, female)exhibited diffuse RNFL and GCIPL thinning, whereas foveal thickness had been preserved in her right eye after 1.5y since the initial onset of ON.Her VA was 0.0 logMAR (Snellen visual acuity: 20/20) at the final visit.Case 2 (41.3y, female)showed similar RNFL and GCIPL thinning in her right eye 10.7y after the first attack.Her foveal thickness had decreased and was measured to 204 μm.Her VA was 0.5 logMAR(Snellen visual acuity: 20/63).
DISCUSSION
Previously, numerous studies have compared changes of RNFL and GCIPL thickness in AQP4-ON, MOG-ON, and MS-ON,and a recent systematic review article reported a comparison of structural and visual outcomes among those three groups[14].In that study, AQP4-ON had worse VA than did MOG-ON or MS-ON.Meanwhile AQP-ON and MOG-ON showed similar severities of RNFL and GCIPL thinning, which were more prominent than that in MS-ON.In our study cohort, we also found poor visual outcomes in the AQP4 group.The AQP4 group also showed more severe RNFL and GCIPL thinning than did the MOG and MS groups, and there was no significant difference in RNFL or GCIPL between the MOG and MS groups.These differences between the previous study and our study were partially caused by differences of ON-recurrence rate and cohort age.
In the present study, we investigated post-ON structural changes according to the etiology.As expected, we found severe structural and functional damage from ON in the AQP4 group.We found a significant loss of foveal thickness in the AQP4 group relative to the two other groups.Like foveal thickness, parafoveal retinal thickness was lower in the AQP4 group than in the MOG and MS groups.Because we measured retinal thickness from the ILM to the RPE in the parafoveal and perifoveal areas, the retinal thinning that we found would have been partially due to GCIPL thinning.However, it should be noted that the GCIPL thickness difference between the AQP4 group and the other two groups was 6-7 μm, whereas the total retinal thickness difference was 12-15 μm.Therefore,the changes in macular structure cannot be fully explained by the change in GCIPL thickness, which fact supports the possibility of primary retinal pathology in AQP4-ON[19-20,23].Fovea consists of all retinal layers except the RNFL, and the Müller cells are concentrated around the fovea.Müller cells,which are glial cells expressing AQP4 in the retina, might be a direct target in NMOSD immunopathogenesis.As such, they can cause primary retinopathy and change of retinal thickness,additionally to the neuroaxonal loss from ON.
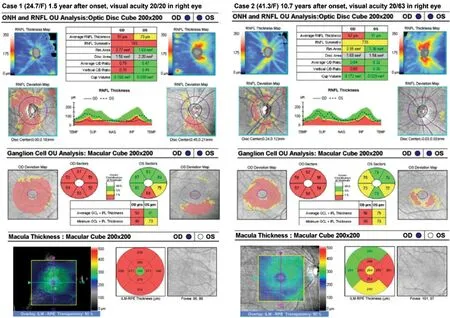
Figure 1 Different visual outcomes according to foveal thickness with similar retinal nerve fiber layer (RNFL) and ganglion cell-inner plexiform layer (GCIPL) thicknesses in AQP4-ON Two cases showed similar RNFL and GCIPL thinning in the right eye: Case 1, with swell-preserved foveal thickness, exhibited a better visual prognosis, whereas Case 2, with diminished foveal thickness, displayed a worse visual outcome.
In the current study, we investigated the correlation between structural changes of macula and visual function in each group, and the correlation between foveal thickness and VA was significant only in patients with AQP4-ON.This finding is consistent with previous studies.Sotirchoset al[28]noted microcystic macular edema of the inner nuclear layer in patients with NMOSD, and those patients had lower rates of high- and low-contrast VA.Jeonget al[18]reported a correlation between foveal thickness and low-contrast VA for eyes with or without a history of ON in patients with AQP4-IgG-positive NMOSD.This reveals that Müller cell dysfunction presenting as foveal change can have an effect on clinical visual function in AQP4-ON.
We included not only VA but also VFI and MD as visual outcomes, which was distinct from the previous studies.Interestingly, in the AQP4 group, foveal thickness was correlated only with VA, not with VF test results.Also,retinal thickness in the parafoveal and perifoveal areas was not correlated with VFI or MD, whereas RNFL and GCIPL thicknesses were correlated with all of the visual function measurements.Therefore, it can be inferred that a pathology other than retrograde neuroaxonal degeneration from AQP4-ON can also cause macular changes and that such changes more affect central VA than peripheral VF.
Meanwhile, in the MOG group, parafoveal and perifoveal retinal thicknesses as well as RNFL and GCIPL thicknesses were correlated with VA, VFI and MD.In the MS group,as with GCIPL, thinner parafoveal and perifoveal retinal thicknesses were associated with worse VA.Therefore, it can be inferred that parafoveal and perifoveal thinning in the MOG and MS groups corresponded well with the GCIPL thinning,suggesting that parafoveal and perifoveal thinning may be induced by the retrograde neuroaxonal damage following ON.However, the correlation coefficient between macular thickness and visual function was larger than that between GCIPL thickness and visual function.This suggests that mechanisms other than retrograde degeneration, such as photoreceptor damage, may also contribute to macular changes[29-30].
Several limitations of our study should be noted.First, it is a retrospective study with a small number of subjects from a single referral center.Therefore, the possibility of selection bias needs to be considered.In particular, our MS cohort showed perfect visual outcomes on the VF test, which fact could render the correlation between structural damage and VF result insignificant.Further studies with a larger number of subjects are needed.Second, we did not include normal subjects as a control.Therefore, retinal change relative to a normal control could not be quantified.Finally, the number of ON recurrences could affect retina structure.However, the number of recurrences in the MOG group was higher than in the other groups.We, therefore, suggested that significant retinal structure damage may occur even with a single optic nerve inflammatory event in AQP4-ON.
Despite these limitations, we did compare the macular structure according to the etiology of ON and found significant thinning in the fovea in the AQP4 group.The results of our study could provide the possibility of more severe retrograde and/or primary retinal damage in AQP4-ON distinct from MOG-ON and MS-ON, which would shed light on its clinical implications.Additionally, we investigated the correlation between structural and visual outcomes.We found not only inner retina parameters, including RNFL and GCIPL, but also the macular parameters showed a significant correlation with visual outcomes in AQP4-ON.We, therefore, suggested that evaluating the macular using OCT can be useful in patients who have acute demyelinating optic neuritis.
ACKNOWLEDGEMENTS
Authors’ contributions:Moon Y, Kim SM, and Jung JH contributed to the data acquisition and interpretation.Moon Y analyzed the data and drafted the manuscript.Kim SM and Jung JH designed and led the study.All authors commented on, revised and approved the manuscript.
Foundation: Supported by the New Faculty Startup Fund of Seoul National University (Jung JH).
Conflicts of Interest: Moon Y,None;Kim SM,None;Jung JH,None.
 International Journal of Ophthalmology2024年4期
International Journal of Ophthalmology2024年4期
- International Journal of Ophthalmology的其它文章
- Comment on: Recurrence after spontaneous separation of epiretinal membrane in a young woman: a case report
- When to repair a retinal detachment?
- Bilateral iridocorneal endothelial syndrome-Chandler’s syndrome: a case report and literature review
- Penetrating canaloplasty in corticosteroid-induced glaucoma: a report of two cases
- On-spot preparation of EDTA solution for the treatment of band keratopathy: a case report
- Non-contact wide-field viewing system-assisted scleral buckling surgery for retinal detachment in silicone oilfilled eyes
