Characteristics of hospitalized patients with confirmed COVID-19 and their hospital management
Lely Indrawati,Dwi Hapsari Tjandrarini,Ning Sulistiyowati,Tin Afifah,Astridya Paramita,Felly Philipus Senewe,Pandji Wibawa Dhewantara
National Research and Innovation Agency Republic of Indonesia,Cibinong,Bogor,West Java 16911,Indonesia
ABSTRACT Objective: To determine the risk factors of mortality among hospitalized COVID-19 patients.Methods: This retrospective study used hospitalization records collected by the Indonesia Health Social Security Administrator Agency (Badan Penyelenggara Jaminan Sosial Kesehatan-BPJS Kesehatan).A total of 38 277 eligible patients with confirmed COVID-19 were analyzed.The dependent variable of the study was the discharge status (death or recovery) of COVID-19.Independent variables were history of morbidity and disease-related occurrence,type of room health facilities,length of stay and demographic variables (sex,age).The analyses use bivariate and multivariate logistic regression to determine the dominating variable associated with all these variables.Results: Of the 38 277 inpatients with PCR-confirmed COVID-19,31 051 (81.1%) were discharged and 7 226 (18.9%) died.Risk of death was positively associated with older age (aOR 5.74,95% CI 4.20-7.87 for 19-64 years old;aOR 13.75,95% CI 9.99-18.92 for 65 years above),male sex (aOR 1.13,95% CI 1.07-1.19),treated in ICU without ventilator (aOR 5.84,95% CI 5.41-6.30) and had comorbid respiratory diseases (aOR 5.39,95% CI 4.93-5.90),but negatively associated with hospital stay of 15 days or longer (aOR 0.39,95% CI 0.36-0.43).Conclusions: COVID-19 related death during hospitalization was associated with duration and type of treatment,and existing medical condition among the inpatient individuals during COVID-19 pandemic in DKI Jakarta.The findings of the study suggest importance of appropriate and timely medical intervention and care.
KEYWORDS: Inpatients;COVID-19;Death;Risk of factors;Indonesia
Significance
Information on the relationship between the characteristics of COVID-19 patients and the way they are treated during hospitalisation is needed to minimise the risk of severity and mortality.The results of the study found that the characteristics of patients who had a higher risk of death were the age group of more than 63 years,male,and had a history of respiratory system as diseases.Patients hospitalized for less than 14 days and admitted without a ventilator were also at higher risk.Mitigation and intervention are needed by patients to get through the critical period of the first 14 days after exposure to COVID-19.
1.Introduction
The World Health Organisation (WHO) has identified the SARSCoV-2 virus as the causative agent of coronavirus disease 2019(COVID-19).Indonesia has been working to address the impact of COVID-19,since the first reported case on 2 March 2020.Indonesia ranks 20th among countries that have reported the highest number of confirmed cases of COVID-19 to WHO.The number of cases recorded in Indonesia until 12 April 2023 is 5 748 308 confirmed cases and 161 095 deaths caused by COVID-19[1].
The COVID-19 outbreak has proven that all viruses have the potential to evolve over time and produce new variations.Changes can impact the characteristics of the virus affecting transmission rates,the severity of the disease it causes,thus impacting the efficacy of pharmacological treatments,diagnostic tools and broader public health interventions[2].The emergence of new virus varieties can increase the transmissibility,leading to an increase in COVID-19 cases.Globally released information shows the Alpha variant in late December 2020[3]led to an increase in COVID-19 cases and deaths in many countries.The Delta variant in July 2021 became the second wave of the COVID-19 pandemic.This variant shows increased infectiousness,rapid replication ability,and reduces the natural effective ability of the body's resistance to disease.About 50% of Delta variants are more rapidly transmissible than Alpha and are the most potent.Many countries have experienced a surge in COVID-19 due to the Delta variant,such as in India including Indonesia[4].
Similar to India,Indonesia with its sizeable number of COVID-19 patients,has caused a significant number of deaths.The continuous surge of COVID-19 cases,especially in DKI Jakarta province,has contributed to the overall caseload requiring hospitalisation.COVID-19 patients in hospitals are categorised into three: those who require ventilators in the intensive care unit (ICU),those who do not require ICU support,and those in the medical unit.Understanding the Length of Stay in hospitals is very important when assessing hospital assets,infrastructure,and facilities[5].
In 2021,the province of Jakarta is facing an increase in COVID-19 cases,yet medical infrastructure and facilities are insufficient.When the number of patients exceeds the available rooms,hospitals are forced to place patients in hospital hallways.The management strategy is to prioritise severe and critical COVID-19 cases to receive mechanical ventilators,to overcome the limitations of offering alternative approaches and ensuring proper care[6].A number of studies on COVID-19 patients show that sex and age over 49 years have a higher risk of severity.In addition,there are risk factors that co-occur with COVID-19 that result in death,such as kidney disease,cerebrovascular disease,and respiratory conditions.
The challenges that must be faced are the ongoing management of COVID-19 and the potential for virus mutations leading to the emergence of new variants that can exhibit faster transmission,severe symptoms,and increased mortality[7].The events that occurred in Jakarta during the second wave of the pandemic will become a historical record of the spread of COVID-19.
The aim of this study was to determine the association of COVID-19 patient characteristics and the associated risk of death during hospitalisation.Although the current COVID-19 pandemic has subsided,continued scientific evidence is still needed.This study not only helps in reducing the current and future mortality risk of COVID-19 patients in healthcare,but also contributes to the refinement of hospital treatment protocols to deal with similar pandemics in the future.
2.Materials and methods
2.1.Data sources
The study used hospitalization records obtained from Pcare,which is a nationwide claims database in Indonesia,maintained by the Indonesian Health Social Security Administrator Agency (Badan Penyelenggara Jaminan Sosial Kesehatan/BPJS Kesehatan).Pcare is in application that provides access for BPJS health participants to first level health facilities (FKTP),such as public health centers,clinics,and doctors.The dataset comprises individual patient details encompassing demographics attributes (e.g.age,sex),duration of hospitalization,primary and secondary diagnosis classified in accordance with the International Classification of Diseases,10th revision (ICD-10),and discharge outcomes.The study used retrospective and de-identified data.
2.2.Study design and population
This study was a retrospective study of patients records who admitted to the hospitals due to COVID-19 in Jakarta during June to November 2021.A total of 74 896 claims associated with COVID-19(e.g.,inpatient/outpatient,suspected/probable/PCR-confirmed case)were recorded in Pcare database during the period.The present study included patient (all age) who tested positive for SARS-CoV-2 by polymerase-chain-reactions (PCR) through a nasopharyngeal or throat swab according to the guideline[8]who are with or without symptoms[9].Patients who received outpatient care,patients with comorbidities linked to maternal health (chapter XV code O00-O99 in ICD-10) and patients with unknown/missing discharge status were excluded from the study.The final participants included in the analysis was 38 277 patients who received inpatient treatment.More details are shown in Figure 1 below.
2.3.Variables
The dependent variable of the study was discharge status (death or recovered) of the COVID-19 patients.Independent variables were co-morbidity,sex,age groups,length of stay in hospital,and care room types.In term of co-morbidity,based on The International Classification of Diseases X (ICD 10) code base is used for diseases classification[10],including a list of three-character categories[11],we classified co-morbidity into the six groups as follow: certain infectious and parasitic diseases (A00-B99);diseases of the blood and blood-forming organs (D50-D89);endocrine,nutritional and metabolic diseases (E00-E89);diseases of the circulatory system(I00-I99);diseases of the respiratory system (J00-J99);and factors influencing health status (Z00-Z99).Once patient have more than one co-morbidity,we incorporated morbidity that were initially recorded in the database,anticipating that the first entry represented the primary illness for which the patient sought medical attention.
Sex was categorized into male and female.Sex is known risk factor linked to severity.While both males and females contract COVID-19 at similar rates,many studied consistently indicates that males faces a higher likelihood of developing severe illness due to COVID-19[12].Age groups are divided into three groups (0-18 years,19-64 years,and 65 years old and above) which represent the group of infants and toddlers,the productive group and the elderly.Studies have shown that age is one of the factors related to higher risk of death because of COVID-19[13].
The length of stay in the hospital (in days) was classified into two categories: fewer than 14 days and more than 15 days.Due to the virus’s incubation period of to 14 days,a 14-day limit is used.Type of care was classified into three groups: ICU/isolation/room with ventilator,ICU/isolation without ventilator,and room/no room without ventilator.The first category is ideal for a room for treatment in hospital.Preliminary data for room types at health facilities for patients with confirmed COVID-19 are split into 10 categories of rooms and available equipment.Based on the preliminary data,the ten categories are no treatment room,ICU without negative pressure with a ventilator,ICU without negative pressure without a ventilator,ICU without a ventilator,ICU without a negative pressure ventilator,ICU with a negative pressure ventilator,isolation without negative pressure without a ventilator,isolation without negative pressure,isolation with negative pressure,and isolation without negative pressure without a ventilator.We did not differentiate between the presence of ICU rooms in “traditional” and “expanded” hospitals as a study found that there was no significant difference between room with traditional ICU and the extended ICU[14].
2.4.Statistical analysis
The analyses use descriptive statistics to provide an overview of the features of the data used.The statistics test utilized was multivariable logistic regression to determine the dominating variable associated with the probability of dying in COVID-19 patients being treated at hospitals in DKI Jakarta Province.Contingency tables were also used to examine the distributions of variables based on characteristic patients.The association between characteristics inpatients and the risk factors associated with inpatients final status,both before and after controlling for potential confounders,was examined using bivariable and multivariable logistic regression analyses.Every variable that the bivariable analysis showed to be significantly correlated with the inpatients’ ultimate status was also included in the multivariable logistic regression analysis.Furthermore,the test can generate an odds-adjusted value for each independent variable that is strongly related to the dependent variable.All analyses were performed using SPSS version 15 (IBM,Armonk,New York,USA)(SN: 6a45501054a0b0c57002).
2.5.Ethics statement
Ethical approval for this study was obtained from the ethic committee of health,National Instituted and Health Research and Development Ministry of Health Republic Indonesia with number ethical approval LB.02.01/2/KE.103/2020.All related procedures were followed in accordance with the Declaration of Helsinki.
3.Results
3.1.General characteristics of the patients
A total of 38 277 inpatient had been confirmed with COVID-19 who received inpatient treatment were included in this study,consisting of 19 044 (49.8%) males and 19 233 (50.2%) females(Supplementary Table 1).The average age of patients was 47.76 years (SD=17.23),ranging from 0 (0-12 months) to 101 years.Based on age group,a high proportion of patients was aged 19-64 years (79.0%).Most of the patients were treated less than 14 days(n=32 988,86.1%) and required ICU/isolation room with ventilator(n=33 958;88.7%).Among the patients,37.2% of patients had no co-morbidity (n=14 259),blood and blood-forming organs (n=1 776,46.3%),certain infection and parasitic diseases (n=1 507,39.3%),and factors influencing health status (n=1 211,31.6%) were common co-morbidities diagnoses among patients (Table 1).Figure 2 provides us with a summary of the patient’s co-morbidity condition in addition to their demographic details of the entire sample,37.3%had no comorbidities,and 62.7% had comorbidities,of which 21.5%were the highest type of comorbid cases,namely patients with comorbid diseases of the circulatory system (Figure 2).
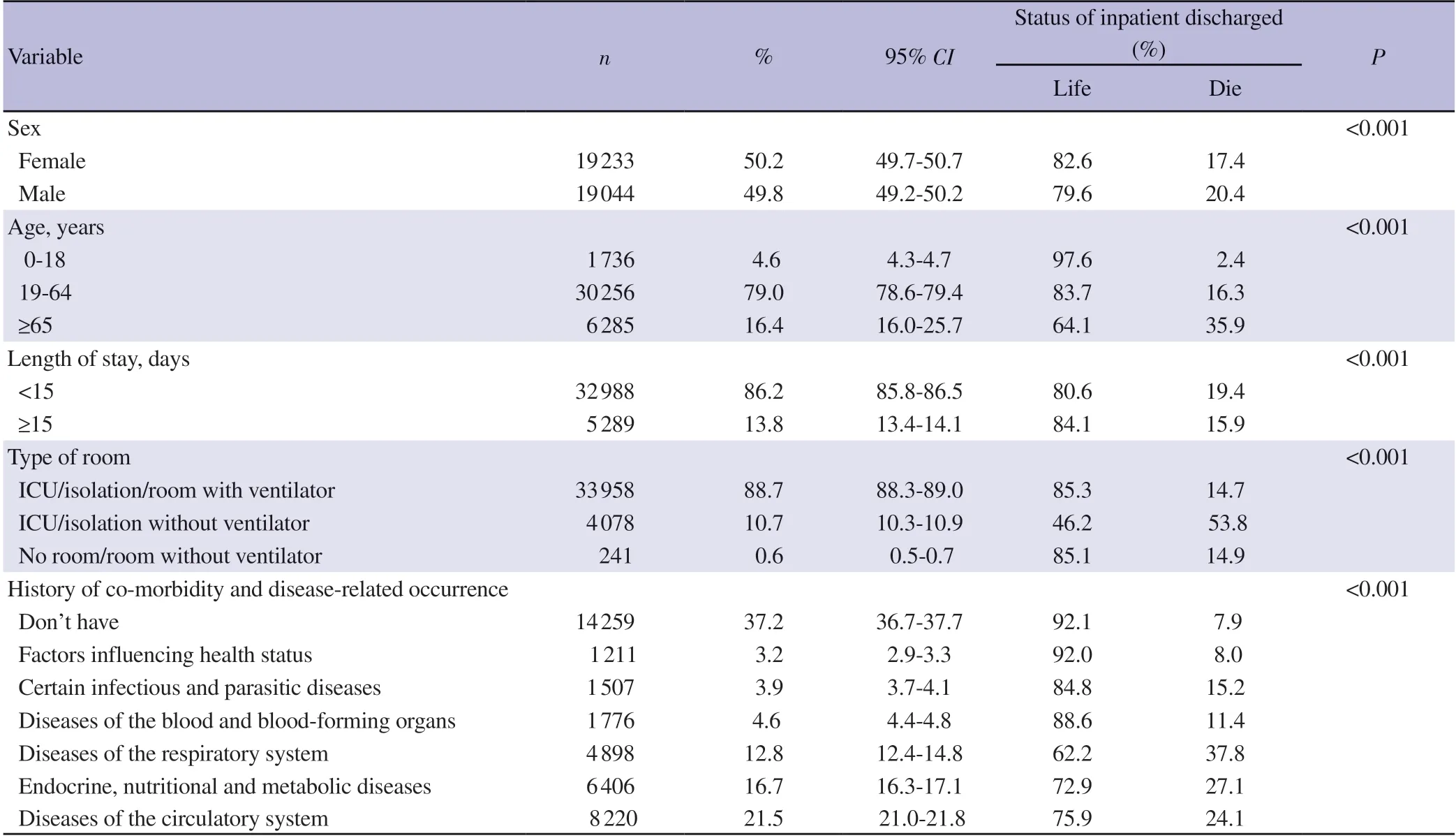
Table 1.Social demographics characteristics of the study respondents (June-November 2021 by BPJS Health).
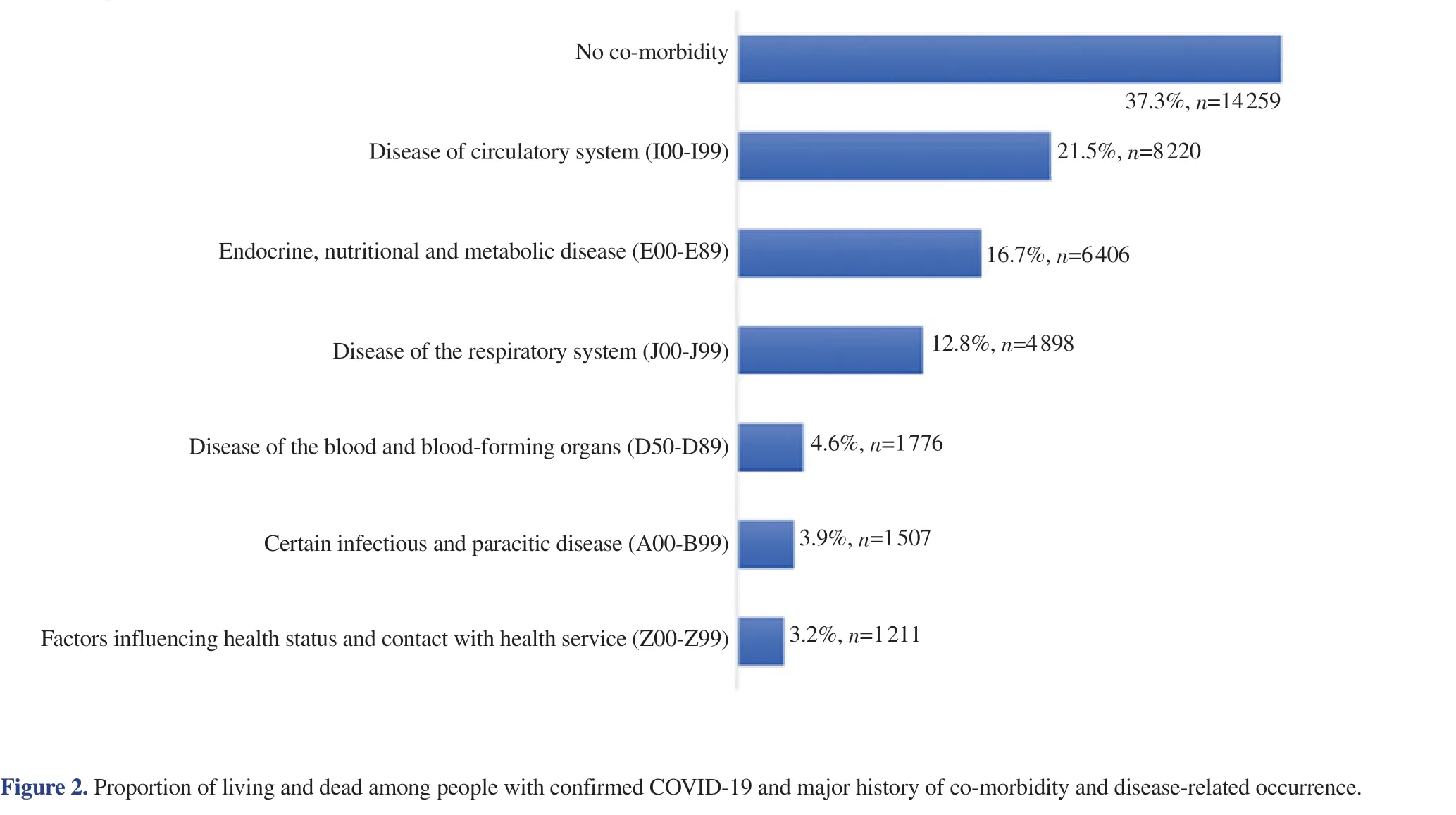
Figure 2.Proportion of living and dead among people with confirmed COVID-19 and major history of co-morbidity and disease-related occurrence.
According to the status of discharge,the largest proportion ofpatients who died due to COVID-19 during hospitalization was male(20.4%),aged 65 years or above (35.9%),length of hospital stay less than 14 days (19.4%),those who treated at ICU/isolation room without ventilators (53.8%),and those patients with respiratoryrelated co-morbidities (37.8%).More details are shown in Table 1.
3.2.Risk factors of mortality due to COVID-19 among patients who received inpatient care
The outcomes of the multivariable analysis are presented in Table 2.By taking into account all independent variables,in-hospitals mortality among patients was associated with sex,length of stay,type of care,and presence of co-morbidity.Male patients were significantly higher odds of death due to COVID-19 during inpatient care (aOR1.13,95%CI1.07-1.19;P<0.001).The odds of death among those older patients were significantly higher (aOR13.75,95%CI9.99-18.92,P<0.001) compared to patients age under 18 years.The risk of death among patients who treated for more than 14 days was significantly lower (aOR0.39,95%CI0.36-0.43,P<0.001)than patients who treated for two weeks or shorter.

Table 2.Multivariable analysis of the associations between the risk of mortality confirmed COVID-19 with history of co-morbidity and disease-related occurrence among inpatients (The 2021 BPJS Health in DKI Jakarta).
The use of ICU/isolation room without ventilators increased of death during hospitalization by 5 times among the patients (aOR5.84 95%CI: 5.41-6.30,P<0.001).The risk of death among patients who had co-morbidities was greater than those who had no underlying illness.Patients with respiratory diseases (aOR5.39,95%CI4.93-5.90),endocrine,nutritional or metabolic diseases (aOR3.17,95%CI2.91-3.46),and circulatory dysfunction (aOR2.47,95%CI2.27-2.70) were higher risk of death to COVID-19 during hospitalization(P<0.001) (Table 2).
4.Discussion
This study reveals the characteristics of hospitalised COVID-19 confirmed patients and associated factors as causes of death.In summary,the results of this study show that the risk of death in hospitalised patients is higher in the following patient characteristics:male,over 65 years old,the length of hospitalization not exceeded 14 days,treated in ICU without a ventilator,and has respiratory system comorbidities.
The results of this study found that the older age,the higher the risk of death in confirmed COVID-19 patients who were hospitalised.This shows the importance of early detection and treatment among the elderly population.The findings of a study by Surendraet al.[15]using DKI Jakarta population data in 2020 showed a marked difference in risk by age group,with patients aged over 70 years having a higher risk of death (crudeOR10.32;95%CI7.61-14.13).Our findings are consistent with the study that the risk of death for COVID-19 patients is higher with increasing age.Studies in various other countries also show similar results[15,16],for example,elderly patients in America have a higher risk of death related to COVID-19[17].Studies among South Koreans also show that age can predict mortality risk[18].
In this study,patient length of stay (LoS) ranged from 1 to 76 days(median 9 days).Further analysing by dividing the patients' LoS into two groups showed the group with a LoS of 14 days or less had an increased risk of mortality.Another study estimated a median hospital LoS of 14 days (interquartile range-IQR: 10-19 days) for China,and 5 (IQR 3-9) days outside China.For ICU,the distribution was more similar at (median 8;IQR 5-13) days for China and 7(IQR 4-11) days outside China.Based on that study,it appears that the median length of stay for COVID-19 patients in China is almost similar to those in Jakarta.Estimates of the LoS for ICU stays and overall hospital admission were provided which can be used for SARS-CoV-2 preparation and planning[19].Another study showed that LoS prediction can be used in conjunction with hospital admission predictions,which are based on the intensity of outbreaks in the surrounding area,to give hospitals the organizational support they need for hospital beds,particularly ventilated ICU beds,and does not outpace supply[20].
Our study found that the type of care was associated with the risk of death in hospitalized patients.The chance of death was seen to be relatively higher in patients who were treated in ICU/isolation without any intervention (e.g.ventilator).This finding suggests that the type of care that best suits the patient's condition is required.A study[21]showed that COVID-19-confirmed patients with severe conditions who received mechanical ventilation had a higher survival rate.
Our study also shows that confirmed COVID-19 patients with comorbidities such as respiratory diseases,endocrine diseases,nutritional problems,and metabolic,and circulation-related diseases have a higher risk of death and is consistent with studies elsewhere.For example,chronic obstructive pulmonary disease and chronic respiratory disease[22]have a close relationship with the severity of COVID-19[23].According to a systematic review and metaanalysis study,it was found that respiratory system diseases correlate with COVID-19 severity.The severity of COVID-19 disease for individuals of all ages is significantly affected by the comorbidity of cardiovascular disease and its risk factors (hypertension and diabetes)[24],regardless of age.Hypertension,type 2 diabetes,nonspecific pneumonia,and other coagulation disorders were shown to be common comorbidities in hospitalised COVID-19 patients.The types of comorbidities in the findings of this study differ from the findings of a study by Ejazet al.who reported obesity,liver disease,kidney disease,malignancy,and HIV as the most life-threatening diseases of COVID-19 patients in the United States,China,and Italy[25].
The limitations of this study are the limited availability of independent variables that cannot provide much information,and there are around 3 000 cases of confirmed COVID-19 patients who were not included in this analysis due to incomplete information.The strength of this study is that there are not many studies that use data at the hospitalised patient level to comprehensively look at the affecting factors of fatality among COVID-19 confirmed patients.The findings of this study underscore the importance of prompt and appropriate medical intervention and treatment of COVID-19 patients by taking into account the characteristics of high-risk patients,including their history of comorbidities to see the priority scale of care.
Conflict of interest statement
The authors declare that they have no competing of interests.
Acknowledgments
The authors would like to express their gratitude to the Social Security Administrator Agency (BPJS Health) for providing the data required for completing this study.
Funding
The authors received no funding for the study.
Data availability statement
Since neither the authors nor any third parties possess the right to distribute the data,the author is unable to make it publicly available.For researchers who fulfill the requirements for access to confidential data,the survey data set can be requested from the Social Security Administrator Agency (BPJS Health).
Authors’ contributions
LI and PWD developed the proposal,and analyzed,and interpreted the patient data.LI and DHT contributed to data analysis and interpretation.LI wrote the initial draft and finalized the manuscript.DHT,NS,TA,FPS,AP,PWD wrote and reviewed the manuscript.All authors read and approved the final manuscript.
Publisher’s note
The Publisher of theJournalremains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
 Asian Pacific Journal of Tropical Medicine2024年3期
Asian Pacific Journal of Tropical Medicine2024年3期
- Asian Pacific Journal of Tropical Medicine的其它文章
- Mitigating fire risks in hospitals: Are we primed and geared up?
- Navigating the future of malaria control: Insights from India's pioneering malaria slide bank
- Smoking of Carica papaya in Nigeria: The rationale,the public health effects and policies for intervention
- Dengue hemorrhagic fever with rectus sheath hematoma: A case report
- Prevalence and risk factors associated with long COVID symptoms in children and adolescents in a southern province of Vietnam
- Epidemic management in a measles outbreak in 2023,the return of vaccinepreventable diseases: A single center,retrospective observational study
