Computed tomography coronary angiography after excluding myocardial infarction: high-sensitivity troponin versus risk score-guided approach
Won Jae Yoo, Shin Ahn, Bora Chae, Won Young Kim
Department of Emergency Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul 05505,Republic of Korea
KEYWORDS: Chest pain; Coronary artery disease; Acute coronary syndrome; Troponin; HEART score
INTRODUCTION
Patients presenting to the emergency department(ED) with chest pain are heterogeneous in terms of clinical presentation and outcomes including the risk of death and non-fatal ischemic events.ED assessment strategies usually focus on predicting the risk of major adverse cardiac events (MACEs) through bedside clinical assessment, electrocardiography (ECG), and serial cardiac markers.[1-4]However, even after evaluating the possibility of MACE, the risk of underlying coronary artery disease (CAD) remains and could be the main cause of future adverse outcomes.Therefore, accurate prediction of obstructive CAD as well as evaluation of the risk of MACE are essential in stratifying patients with chest pain in the ED.
A high-sensitivity troponin I (hsTnI) assay was introduced to detect low troponin levels that could not be previously detected.[5,6]With the reduction in the detection limit of troponin, its widespread use has led to changes in the diagnoses of unstable angina into myocardial infarction.[7]Using this assay, recent studies have shown that with a threshold of 5 ng/L, a negative predictive value (NPV) of >99.5% for MACE was obtained among patients identified as having low-risk chest pain.[8,9]Despite being within the normal range,patients with hsTnI concentrations between 5 ng/L and the 99thpercentile had a higher medium- and longterm risk of MACE, and this range was classified as an intermediate hsTnI concentration.Lee et al[10]used cardiac troponin to select patients for investigating occult CAD with computed tomography coronary angiography(CTCA) performed after discharge from the ED.They found that the prevalence of CAD was 3 times higher in patients with intermediate troponin concentrations than in those with low concentrations (<5 ng/L).Therefore, an intermediate troponin concentration can be used to select patients for downstream investigation after ruling out myocardial infarction.
The HEART (history, electrocardiography, age, risk factors, and troponin) score is a clinical prediction tool used to assess the risk of MACE in patients presenting with chest pain.The score ranges from 0 to 10 and is used to classify patients into low- (0–3 points), intermediate-(4–6 points), and high- (7–10 points) risk categories for MACE, which can help guide clinical decision-making(Supplementary Table 1).In our previous study, we attempted to modify the HEART pathway by adding CTCA for patients with 0–3 points and a positive troponin test result or with 4–6 points.The incorporation of CTCA into the HEART pathway for selected patients improved its prediction accuracy for MACE and increased the proportion of patients with low risk.[11]In another study,we found that the HEART score was superior to the Thrombolysis in Myocardial Infarction (TIMI) and Global Registry of Acute Coronary Events (GRACE) scores, in predicting both obstructive CAD and MACE.[4]Therefore,we hypothesized that the HEART score could be more useful than troponin concentration for selecting candidates for CTCA.In this study, we attempted to evaluate the accuracy of the HEART score in selecting patients for further investigation after ruling out myocardial infarction;we also compared the performances of the HEART score and troponin concentration in the selection of candidates for CTCA to identify occult CAD in patients who present to the ED with suspected acute coronary syndrome (ACS).
METHODS
Study setting
This study included patients from a prospective observational cohort study that was conducted to validate a chest pain accelerated-diagnostic protocol in the ED.The original cohort included 821 consecutive adult patients (≥18 years) who presented with chest pain suggestive of ACS to the ED of Asan Medical Center,Seoul, Republic of Korea, from April 2021 to March 2022.Our ED has an annual volume of approximately 120,000 patients and serves as a tertiary referral center.
Selection of participants
The inclusion criteria for this study consisted of adult patients who were suspected of having ACS in whom acute myocardial infarction had been ruled out based on normal peak cardiac hsTnI concentrations within the reference range.Additionally, all patients underwent CTCA during their ED stay.The exclusion criteria encompassed participants with elevated hsTnI concentrations above the reference range, and those with renal insufficiency, severe allergic reactions to contrast media, or any other reasons precluding CTCA.
Data collection and definition
A standardized chest pain evaluation form, including questions on the patient’s demographic data, height,weight, cardiovascular risk factors, family history, past medical history, and current medication, was used to collect relevant data.When a patient presents to our ED with chest pain suggestive of ACS, ECG is performed along with a serial hsTnI assay at a 2-hour interval.Cardiac hsTnI was used for troponin measurement using the Atellica IM hsTnI assay (Atellica hsTnI; Siemens,Germany; the 99thpercentile upper-reference limit [URL]60 ng/L) and the higher hsTnI level between each pair of samples was selected for the analysis.The patients were classified according to the hsTnI concentration and HEART score.Since patients with any elevated hsTnI levels greater than the 99thpercentile between 0 h and 2 h were excluded, hsTnI levels of <5 ng/L were considered low and levels between 5 ng/L and the 99thpercentile (60 ng/L) were considered intermediate hsTnI concentrations.HEART scores of 0 to 3 were classified as low-risk scores, whereas scores ≥4 were classified as not low-risk scores.
All patients underwent CTCA during their ED stay.Multi-detector CTCA was performed using a dual-source scanner (Somatom Definition; Siemens, Germany)with iodine-based contrast media, and the presence of obstructive CAD was defined as a stenosis of >50%in more than one major epicardial coronary artery, as interpreted by certified radiologists.Atherosclerotic plaque burden was based on the segmental involvement score, which is the total number of segments with any plaque that ranges from 0 to 16, and coronary artery calcium score, using the Agatston method.[12,13]According to the CTCA data, stenosis was classified as none (no luminal stenosis), minimal (<30%), mild(30%–49%), moderate (50%–69%), or severe (≥70%)for each coronary artery.[12]The primary outcome was the presence of obstructive CAD on CTCA.
Statistical analysis
Continuous variables with a normal distribution were expressed as means ± standard deviations and were compared using Student’st-test.Variables with non-normal distributions were expressed as medians and interquartile ranges (IQRs) and analyzed using the Mann-Whitney test.Categorical variables were calculated as absolute numbers with percentages and compared using the Chi-square test.The presence of CAD in patients with intermediate hsTnI concentrations and not low-risk HEART scores compared with patients with low hsTnI concentrations and lowrisk HEART scores using logistic regression modeling,expressed as odds ratios (ORs) and corresponding 95%confidence intervals (CIs).The performances of hsTnI concentration and HEART score were compared using the sensitivity, specificity, positive predictive value (PPV), and NPV.The area under the receiver-operating characteristic(AUROC) curve of the HEART score and hsTnI was compared.The nonparametric method was used to compare the AUROCs.[14]All statistical analyses were conducted using SPSS Statistics V21.0 (IBM, USA) and MedCalc?Statistical Software version 20.111 (MedCalc Software Ltd., Belgium).Statistical significance was set at aPvalue of <0.05.
RESULTS
Of the 821 eligible patients, 378 had elevated hsTnI levels and 10 did not undergo CTCA; therefore, 433 patients were included in this study (Figure 1).Of them,243 (56.1%) had low hsTnI concentrations (<5 ng/L)and 190 (43.9%) had intermediate hsTnI concentrations(5 ng/L to 99thpercentile); meanwhile, 172 (39.7%) had low-risk HEART scores (0–3), and 261 did not have lowrisk HEART scores (≥4).
Table 1 summarizes the baseline characteristics of the patients.The mean age was 63.9±12.5 years, and 252(58.2%) were men.The patients with intermediate hsTnI concentrations were older than those with low hsTnI concentrations (68.2 ± 12.2 years vs.60.6 ±1.8 years)and were more likely to have hypertension and a history of CAD (bothP<0.05).Similarly, patients with non-lowrisk HEART scores were older than those with low-risk HEART scores (69.5 ± 9.6 years vs.55.6 ±11.8 years)and were more likely to have hypertension, diabetes and a history of CAD (allP<0.001).Both the TIMI and GRACE scores were higher among the patients with intermediate hsTnI concentrations than those with low hsTnI concentrations (bothP<0.001).These scores were also higher among the patients with non-low-risk HEART scores than among those with low-risk HEART scores (bothP<0.001).
Overall, 25.9% of the patients had normal coronary arteries, and 74.1% had any CAD; meanwhile, 72.3%had non-obstructive CAD, and 27.7% had obstructive CAD (Table 2).The patients with intermediate hsTnI concentrations were more likely to have any CAD(83.2% vs.67.1%,P<0.001) or obstructive CAD(40.0% vs.18.1%,P<0.001) than those with low hsTnI concentrations; the former also had a higher atherosclerotic burden (bothP<0.001).Similar findings were observed for the HEART scores.However, the HEART score showed higher sensitivity and NPV for detecting obstructive CAD in each classification than the hsTnI concentration(sensitivity: 89.2% vs.63.3%; NPV: 92.4% vs.81.9%).
The HEART score showed higherORs for the detection of any CAD and obstructive CAD than hsTnI concentration (HEART score:OR9.03 [95%CI5.46–14.95] for any CAD,OR8.50 [95%CI4.59–15.75] for obstructive CAD vs.hsTnI concentration:OR2.42 [95%CI1.52–3.86] for any CAD,OR3.02 [95%CI1.95–4.68]for obstructive CAD) (Figure 2).
The AUC analysis for the HEART score and hsTnI for obstructive CAD showed a significant difference (HEART 0.746 [95%CI0.700–0.790] vs.hsTnI 0.612 [95%CI0.560–0.670],P=0.134) (Supplementary Figure 1).
There were 6 (1.4%) patients with significant extracoronary findings.These included 2 patients who had pulmonary embolism, 1 who had pericardial effusion, 2 who had lung cancer, and 1 who had aortic dissection.
DISCUSSION
This study aimed to investigate the accuracy of the HEART score in identifying candidate patients for further investigation with CTCA after ruling out myocardial infarction.Despite our patients having normal hsTnI levels,27.7% had obstructive CAD, and adding the HEART score was more accurate in identifying the patients with obstructive CAD than relying on hsTnI concentration.The incidence of obstructive CAD was similar (around 40%) in patients with intermediate hsTnI concentrations and patients with non-low-risk HEART scores.However,the sensitivity and NPV of the HEART score in detecting obstructive CAD were 89.2% and 92.4%, higher than 63.3% and 81.9% of hsTnI concentrations, respectively;therefore, adding HEART score could identify patients at low risk of CAD more accurately.Moreover, the patients with non-low-risk HEART scores were 8.5 times more likely to have obstructive CAD than those with low-risk HEART scores, and the patients with intermediate hsTnI concentrations were 3 times more likely to have obstructive CAD than those with low hsTnI concentrations.
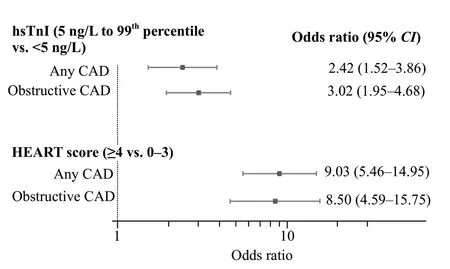
Figure 2.Association between coronary artery disease and troponin concentration or HEART score.HEART: history, electrocardiography,age, risk factors, and troponin; CAD: coronary artery disease; CI:confidence interval.

Table 1.Baseline characteristics of patients stratified by troponin concentration and HEART score

Table 2.Computed tomography coronary angiography findings stratified by troponin concentration and HEART score
Previous studies showed that patients with hsTnI levels between 5 ng/L and the 99thpercentile had a higher risk of 30-day and 1-year mortality from myocardial infarction or cardiac events than those with levels <5 ng/L at presentation; intermediate hsTnI concentration was associated with higher medium- and long-term risk of adverse events than low hsTnI concentration.[8,9]In a randomized controlled trial that evaluated the 0/1-hour hsTnI protocol for patients with suspected ACS, an intermediate hsTnI concentration was associated with higher rates of revascularization within 30 d and 12 months and death or myocardial infarction at 12 months than a low hsTnI concentration.[15]To determine the association between intermediate troponin concentration and future MACE, Lee et al[10]analyzed outpatient CTCA results of patients for whom myocardial infarction was ruled out.The patients with intermediate troponin concentrations had more CAD (71.9% vs.43.4%;OR3.33; 95%CI1.92–5.78) and atherosclerotic plaque burden (median segment involvement score: 2.0 vs.0.0,P<0.001) than those with low troponin concentrations;these findings were attributed to the possibility that patients with high atherosclerotic plaque burden in CAD and plaque instability are likely to develop subclinical myocardial necrosis.They suggested a troponin-guided CTCA application for investigation of CAD after excluding myocardial infarction.In our study, patients with intermediate hsTnI concentrations were associated with any CAD or obstructive CAD;regarding the atherosclerotic plaque burden, patients with intermediate hsTnI concentrations had higher segmental involvement scores and calcium scores than those with low concentrations.However, when the HEART score was added after ruling out myocardial infarction HEART score-guided CTCA application more accurately identified patients with obstructive CAD than CTCA application based on the hsTnI concentration.Moreover,comparing the performance of the HEART score and hsTnI concentration, the higher sensitivity and NPV of the HEART score could help identify low-risk patients more accurately, who can be discharged from the ED safely without further evaluation.
The HEART score includes both age and other cardiac risk factors such as smoking, hypertension, diabetes mellitus,hypercholesterolemia, obesity, and family history.[16]These traditional cardiac risk factors can reflect the risk of atherosclerotic plaque burden and the presence of CAD more accurately than troponin concentration, which is an indicator of myocardial damage.[17]Moreover, troponin concentration can be affected by non-coronary and even non-cardiac factors.[18,19]A previous study showed that individuals with undetectable hsTnI levels had a low risk of long-term incident atherosclerotic cardiovascular disease, similar to those with a coronary calcium score of zero;[20]however, many patients frequently showed discordances between the coronary calcium score and troponin concentrations, and an increased risk for atherosclerotic cardiovascular disease was found among these patients.
Chest pain accelerated diagnostic protocols or algorithms using very low levels of hsTnI at presentation, or the lack of change within 1–2 h, enables myocardial infarction to be ruled out rapidly.Due to the prognostic utility of hsTnI, it has become an alternative to well-known chest pain risk scores in clinical settings.However, it must be emphasized that the risk of CAD in patients with normal troponin concentrations still presents and is not negligible.Therefore, chest pain risk scores, such as the HEART score, could be utilized to assist in disposition.[21]
Limitations
Our study has several limitations.This study was carried out at a single center, and the background and ethnicity of the population differ from previous studies.Hence, the sample was not representative of the global population, implying that the results should be interpreted with caution, considering the peculiarities of healthcare systems in different countries.The definitions of obstructive CAD are different among many studies.We chose >50% stenosis of the coronary artery diameter as the reference threshold;[22-24]however, other studies have used different thresholds,[10,25]which could also limit the generalizability of our results.
Within the original study cohort from which our study population was selected, CTCA was not performed as a routine workup; it was conducted at the discretion of the attending emergency physician and since practice patterns vary among clinicians, the included patients do not represent the overall ED population of patients with undifferentiated chest pain.
CONCLUSION
In the ED, a significant proportion of patients who had normal hsTnI concentrations at presentation to the ED had obstructive CAD; the HEART score identified patients with CAD than the hsTnI concentration more accurately.After excluding myocardial infarction, adding HEART score to select candidate patients for CTCA could improve risk stratification more accurately than relying on hsTnI concentration.
Funding:None.
Ethical approval:This study was approved by the institutional review board of Asan Medical Center (No 2021-0562).
Conflicts of interest:The authors have no conflicts of interest.
Author contribution:All authors contributed to the preparation of this paper.SA, WYK conceived and designed the analysis;SA, BC, and WJY collected the data; SA and WJY performed the analysis, and wrote the paper.
All the supplementary files in this paper are available at http://wjem.com.cn.
 World journal of emergency medicine2023年6期
World journal of emergency medicine2023年6期
- World journal of emergency medicine的其它文章
- Tension urinothorax as a reversible cause of cardiac arrest: a case report
- A case of pulmonary mucormycosis presented with cardiac arrest
- Pyopneumothorax caused by Parvimonas micra and Prevotella oralis: a case report
- Hemorrhagic pancreatitis from fenofibrate and metformin toxicity: a case report
- The effect of prophylactic antibiotics in acute upper gastrointestinal bleeding patients in the emergency department
- The effects of hyperbaric oxygen therapy on paroxysmal sympathetic hyperactivity after cardiopulmonary resuscitation: a case series
