Undifferentiated carcinoma with osteoclast-like giant cells of the pancreas mimicking pancreatic pseudocyst
Emin Tlkic ′ , Jsmink Igrec , Ann-Ktrin Kufmnn-Bühler, Elmr Jnek ,Sygull Stephn , Peter Schemmer, Michel Fuchsj?ger
a Division of General Radiology, Department of Radiology, Medical University of Graz, Graz, Austria
b Diagnostic and Research Institute of Pathology, Medical University of Graz, Graz, Austria
c General, Visceral and Transplant Surgery, Department of Surgery, Medical University of Graz, Graz, Austria
TotheEditor:
Undifferentiated carcinoma with osteoclast-like giant cells (UCOGC) is one of eight histological subtypes of pancreatic ductal adenocarcinoma (PDAC) according to the 2019 WHO classification[1].It accounts for<1% of exocrine pancreatic carcinomas.This rare variant occurs in slightly younger patients than conventional PDAC,with a slight female predominance (male:female,7:10).On imaging,UC-OGC appears as a large cystic-solid mass with areas of hemorrhage and necrosis.Thus, they may potentially resemble pancreatic pseudocysts.Given the rarity of this variant, the prognosis is unclear, with reports of a median survival of 11 months for unresectable tumors on the one hand, and long-term survival>5 years on the other hand.Mucinous cystic neoplasms are predisposing factors for their development in 20% of the cases.Common clinical signs and symptoms include abdominal pain, weight loss, and jaundice, but UC-OGC tends to be asymptomatic in early stages.We reported one rare case of UC-OGC together with a review of previously published cases in English language using the search term“undifferentiated carcinoma osteoclastic giant cell pancreas”.
A 47-year-old male obese patient was admitted for right upper abdominal pain.He denied any nausea, pyrexia, or bowl movement irregularity.Symptoms evolved 2 weeks ago and gradually worsened over time.The patient’s previous medical history included type II diabetes and morbid obesity.He underwent laparoscopic gastric banding ten years ago.His vital parameters were stable and within normal limits.The abdomen was soft, with a mild right upper quadrant pain and tenderness to palpation.Laboratory findings included an almost 20-fold increase of C-reactive protein (CRP)(93.1 mg/L) along with increased gamma-glutamyl transpeptidase(GGT), aspartate aminotransferase (AST), and creatine kinase (CK)values.
Contrast-enhanced computed tomography (CT) of the abdomen demonstrated several encapsulated serous fluid collections without evidence of infection and a 5.8 cm cystic lesion (density 20 HU) with thickened wall in the pancreatic body (Fig.1A-D).Theentire findings were interpreted as pancreatic pseudocysts.Also,a regular positioned gastric band was detected.Due to the lack of history of pancreatitis, further assessment with magnetic resonance imaging (MRI) was recommended.Images demonstrated a thick-walled cystic lesion in the pancreatic body with suspicious wall-adherent nodular proliferations and a single enlarged lymph node measuring 3.3 ×1.7 cm in the hepatoduodenal ligament(Fig.1E-H).The pancreatic lesion showed moderate to low signal intensity on T1WI, and moderate to high signal intensity on T2WI with fluid-fluid level indicating blood products (Fig.1).There was a rapid arterial contrast-enhancement in the solid tumor portions.On magnetic resonance cholangiopancreatography, the main pancreatic duct revealed no focal areas of dilation or stenosis.Although well circumscribed, with no evidence of infiltration into the surrounding large vessels or organs, the lesion imaging appearance was strongly suspicious of malignancy.Additional imaging, such as positron emission tomography-computed tomography(PET-CT)/MRI, was not performed because the lesion in pancreas showed clear nodular proliferation and contrast enhancement on MRI, suspicious for malignancy.The very same information would have been given by PET-CT/MRI without providing additive aspects.Further, indication for oncological pancreatic left resection was given including surgical treatment of the abscess formations in the left upper quadrant.
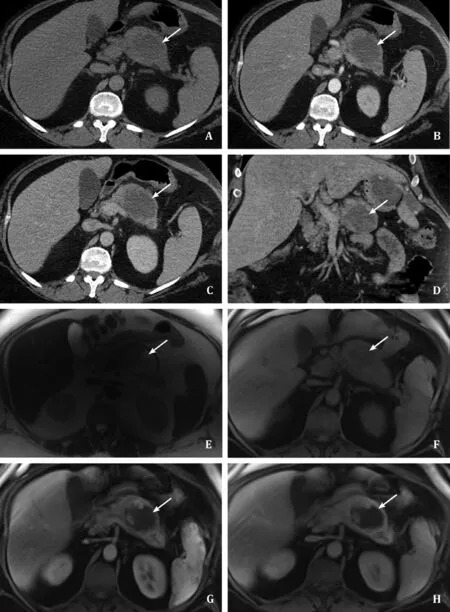
Fig.1.A-D: Preoperative contrast enhanced computed tomography of the abdomen.Axial ( A, B, C) and coronal ( D) images demonstrate a thick-walled cystic lesion in the pancreatic body (white arrow).E-H: Preoperative magnetic resonance imaging scan of the abdomen with intravenous Gadolinium administration.Images reveal a complex cystic lesion of the pancreatic body with fluid-fluid level on axial T2 weighted images ( E ).Axial pre- ( F) and post-Gd ( G, H) T1 weighted images demonstrate internal nodular proliferations and peripheral contrast media uptake, suggestive for a cystic pancreatic tumor (white arrow).
No preoperative biopsy was performed since surgical strategy would not have been influenced.Carbohydrate antigen (CA) 19-9 was not measured since it is also likely to be increased in cases with intraabdominal abscess.
In a multidisciplinary setting, it was decided to perform a left pancreatic resection.Intraoperatively, a large cystic pancreatic tumor and multiple intraabdominal abscesses due to disconnection of the gastric band line were identified.
The patient underwent open oncological pancreatic left resection including resection of the spleen.Access to the abdomen was established with a median laparotomy.After exploration of the abdomen to exclude metastatic disease, the major omentum was resected and the omental bursa was opened for access to the pancreas.During this operative step, the gastric band, including the disconnected gastric band line with associated abscess formations, was removed.Subsequently, the short gastric vessels were occluded, and both the splenic artery and vein were dissected free and divided between vessel clips laterally to the pancreatichead.The tail of the pancreas was resected with an Endo GIATMstapler(Medtronic, Vienna, Austria).To prevent pancreatic fistula, the stapler line was over-sutured, including z-stitches of the pancreatic duct.The pancreatic tail was removed together with the spleen and a lymphadenectomy was performed.The immediate postoperative course was uneventful.Adjuvant chemotherapy was suggested by the tumor board.
The histologic workup of the operating room (OR) specimen revealed partially necrotic and hemorrhagic UC-OGC of the pancreas body (Fig.2), with intraductal tumor invasion and infiltration of the peripancreatic fat tissue.Tumor cells stained positive for Vimentin, STAT6, CAM5.2 and AE1/2 by immunohistochemistry.Malignant cells were negative for S100, CD34, SOX-10, E-cadherin and desmin.
No combination with conventional PDAC or intraepithelial pancreatic neoplasia was identified.The surgical margins and lymph nodes were negative for neoplastic infiltration.Also, there was no evidence of distant metastases in the staging CT of the head, thorax, abdomen and pelvis, thus resulting in a surgical-pathological tumor staging G4 pT3 N0 R0 according to Union for International Cancer Control (UICC) 2017 TNM staging system.
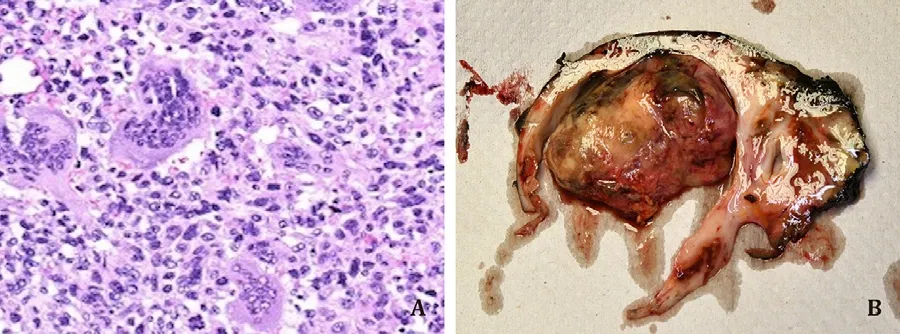
Fig.2.Postoperative histopathological specimen of UG-OGC.A: The tumor is a hypercellular mass composed mainly of poorly cohesive neoplastic cells that diffusely infiltrate the tissue.The neoplastic cells are densely packed with sparse stroma,sometimes arranged in small aggregates.Glandular differentiation is absent.Tumor cells exhibit a high degree of pleomorphism with scant cytoplasm.Bizarre tumor cells, hemorrhage foci and necrosis are also seen.A variable number of nuclei is characteristic of this type of undifferentiated carcinoma with osteoclast-like giant cells.B: The macroscopic images of the pancreatic specimen after resection showing a cavity of about 5 cm with a nodule filling the cavity.UG-OGC: undifferentiated carcinoma with osteoclast-like giant cells.
UC-OGC is a rare variant, accounting for<1% of exocrine pancreatic carcinomas.The first case was described in 1968[2].We identified 148 cases in the English literature, including three larger series of 13, 22 and 38 cases [3,11,12].Data on prognosis are limited, but current research suggests that UC-OGC has a more favorable 5-year survival than conventional PDAC (59.1% vs.15.6%)[4].Several studies reported on long-term survival of several years,with a maximum of 120 months [3,14].Several parameters were associated with shorter survival in recent studies, [13,15]including expression of programmed death-ligand 1 (PD-L1), older age, male sex, smaller tumor size, positive lymph node metastasis, as well as concomitant components of ductal adenocarcinoma and pleomorphic giant cell carcinoma [13,16].
Typical symptoms include abdominal pain, weight loss and jaundice.In our particular case, the patient was asymptomatic for UC-OGC and pancreatic carcinoma was discovered incidentally during evaluation of chronic leakage from a disconnected gastric banding line.
This tumor entity is more common in the pancreas body and tail and usually appears as a large thick-walled cystic mass with nodular solid portions and clear boundary.Similar to our case,previous studies described that solid internal proliferations showrapid contrast enhancement in the arterial phase with continuous enhancement at portal venous and delayed phasen [4,5].Although small calcifications are occasionally visible, mostly resembling osteoid formations [5,7], in our case calcification was absent.Internal fluid-fluid levels in our case were in line with areas of hemorrhage and necrosis, which are previously described as common features of UC-OGC.As in our case, a previous work found that UC-OGC resembles pancreatic pseudocyst on imaging[6].
Sixty percent of OC-OGCs showintraductal or intracystic growth.Moreover, perineural and lympohvascular infiltration, as well as infiltration of large surrounding vessels and abdominal organs are common features.In our case, the tumor infiltrated into the main pancreatic duct and the peripancreatic fat tissue.Our patient had one pathologic enlarged lymph node in the hepatic hilum, but histology showed reactive changes and chronic infection probably due to gastric bandage leakage.In advanced stages, distant metastases occur most of all in the lungs, liver,adrenal glands and bone[7].There is no uniform treatment strategy.Complete surgical resection proved to be curative if the tumor is limited to the pancreas[8].Several studies report adjuvant chemotherapy with gemcitabine, whereby one study demonstrated that chemotherapy with gemcitabine plus nab-paclitaxel could improve survival in a cohort of unresectable undifferentiated carcinoma (UDC) and UC-OGC [9,12].We identified one case that reported on radiation therapy following surgery[10].Our patient underwent combined pancreatic left resection with splenectomy, left adrenalectomy, cholecystectomy and omentectomy, as well as removal of the dysfunctional gastric band.The surgicalmargins were negative and there was no evidence of lymph node metastases.Due to increasing inflammatory markers in the postoperative course, a CT of the abdomen was performed to search for a local infection.The images showed encapsulated peripancreatic fluid formation in the former surgical area, suspicious for an abscess.Puncture and drainage insertion identifiedEnterobacterspecies, and the infection resolved completely with systemic antibiotic therapy.For this reason and contrary to the recommendation of the tumor board, the patient could not receive chemotherapy immediately after surgery.Further, the patient developed a severe acute respiratory syndrome corona virus 2 (SARS-CoV2) infection and virus associated pneumonia.Thus, the suggested adjuvant chemotherapy with FOLFIRINOX (oxaliplatin, irinotecan, fluorouracil) was delayed once again.At the last follow-up, 8 months after surgery, a CT scan showed suspected liver metastases and unclear lung lesion in the right lower lobe.
It remains unclear to what extent adjuvant therapy would benefit metastasis-free progression.The aggressiveness of the tumor despite R0 resection could be confirmed.Potential underlying mechanism of the aggressive PD-L1 positive UC-OGC behavior most likely is an inhibition of anti-tumor immunity by PD-L1, allowing neoplastic cells to escape the cytotoxic activity of T-lymphocytes.UC-OGC is characterized by inflammatory changes including tumor infiltrating CD3+and CD8+lymphocytes.This is in contrast to conventional PDAC.Therefore, novel therapeutic strategies are based on immune checkpoint immunotherapy in these patients [11–13].
In conclusion, this case demonstrates the importance of a systematic approach in the diagnostic evaluation of pancreatic cysts.Accurate systematic exploration and additional imaging with MRI is essential and can detect this rare entity.Early and complete resection of UC-OGC improves prognosis compared with conventional PDAC when tumor is limited to the pancreas.
Acknowledgments
We thank Prof.Dr.Armin Gerger, Division of Oncology, Department of Internal Medicine, Medical University of Graz, for communicating information on the chemotherapy protocol.
CRediT authorship contribution statement
Emina Talaki ′c:Conceptualization, Data curation, Formal analysis, Methodology, Supervision, Writing – original draft, Writing –review & editing.Jasminka Igrec:Conceptualization, Supervision,Writing – review & editing.Ann-Katrin Kaufmann-Bühler:Conceptualization, Supervision, Writing –review & editing.Elmar Janek:Conceptualization, Supervision, Writing –review & editing.Sygulla Stephan:Conceptualization, Supervision, Writing –review & editing.Peter Schemmer:Conceptualization, Methodology,Supervision, Writing – original draft, Writing – review & editing.Michael Fuchsj?ger:Conceptualization, Supervision, Writing – review & editing.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this report and any accompanying images.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
 Hepatobiliary & Pancreatic Diseases International2022年4期
Hepatobiliary & Pancreatic Diseases International2022年4期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Hepatobiliary&Pancreatic Diseases International
- Meetings and Courses
- Adenovirus and severe acute hepatitis of unknown etiology in children: Offender or bystander?
- Safety of rectal indomethacin (100 mg) for the prevention of post-ERCP pancreatitis in the Japanese population: A single-center prospective pilot study
- Branching patterns of the left portal vein and consequent implications in liver surgery: The left anterior sector
- Recurrent pyogenic cholangitis: An indication for liver transplantation
