Efficacy of propofol versus ketamine in modified electroconvulsive therapy: A prospective randomized control trial
Debarshi Guha, Kiran Sheshadri, Shalendra Singh, Sonia Bhan
Department of Anaesthesiology and Critical Care, Armed Forces Medical College, Pune 411040, India
ABSTRACT
KEYWORDS: Electroconvulsive therapy; ECT; Propofol; Ketamine;Motor seizure duration; EEG seizure duration; Haemodynamic effects
1. Introduction
Electroconvulsive therapy (ECT) is the first-line treatment for patients with acute mania, mood disorders, severe depression,and catatonia[1-3]. The literature revealed treatment effectiveness is associated with the seizure duration during ECT[4,5]. An ECT treatment has uncertain therapeutic benefits if motor seizure duration is less than 15 s or if motor seizure duration persists for a prolonged time. Treatment may be considered adequate only if the patient has had a generalized seizure that exceeds a predetermined minimum duration, in which 20 to 30 s are requested for motor seizure or 30 to 40 s are requested for electroencephalographic(EEG) manifestations.
The purpose of anesthesia during ECT is to induce an unconscious state, and the agents used should not impact motor seizure[6,7].Thus, the type of anesthetic agents used in modified ECT becomes very important as all anesthetic agents have some seizure modifying properties. The ideal hypnotic drug for ECT would have a series of characteristics of rapid onset, minimal effect on seizure duration,and smooth recovery. The most commonly used drug propofol has rapid induction and smooth recovery profile and anti-convulsion properties whereas ketamine is also frequently used for ECT anesthesia, which has less effect on seizure duration, adequate anesthesia, and analgesia with additional anti-depressive effect[8,9].Thus, it is important to provide a patient-oriented approach for both anesthesia and electric current administration, and communication between the anesthesiologist and the psychiatrist.
This study aimed to compare the effects of propofol and ketamine during modified ECT on seizure duration and to compare the hemodynamic profile during the procedure as well as the time taken for eye-opening after the procedure.
2. Patients and methods
2.1. Study design
This randomized, prospective control trial was carried out at a tertiary care center from May 2019 to May 2020..
2.2. Ethical approval and trial registration
After clearance from the institutional ethical committee (EC/OCT/2018 dt 22 Oct 2018), the study was initiated. Written informed consent was sought from the next of kin of the patients. The trial was registered at the clinical trials registry of India (Registration No:CTRI/2019/05/018890).
2.3. Inclusion and exclusion criteria
An entire 44 patients with a physical status of American Society of Anaesthesiologists GradeⅠ-Ⅲ, with an age older than 18 years and planned for modified ECT under anesthesia were included.Unwilling patients, patients having raised intracranial pressure, and pregnant patients were excluded.
2.4. Grouping
During the study period, they were randomly allocated into two groups. In the Propofol group (n=22) each patient received injection of propofol 1.5 mg/kg i.v.. In the ketamine group (n=22) each patient received ketamine 0.8-1.2 mg/kg i.v.. Randomization was done using a computer-generated list of numbers and assigned to one of the two groups. Each number was enclosed in an opaque sealed envelope and patients were asked to select and hand it over to the anesthesiologist,who compared it with the computer-generated list and assigned the patient to one of the two groups.
2.5. Intervention
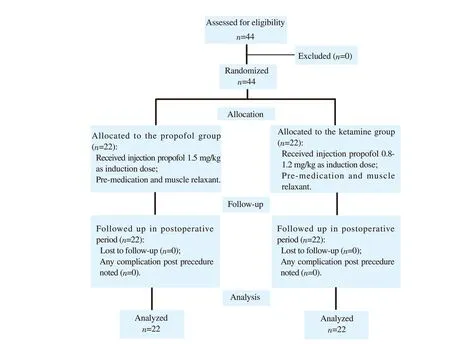
Figure 1. The study flowchart.
On the arrival of the patient in the ECT suite, an intravenous line was secured. Minimum mandatory monitoring was applied which includes heart rate, non-invasive blood pressure , pulse oximetry (SpO2), and electrocardiogram (ECG). All patients were pre-oxygenated with 100% oxygen for 3-4 min and the following drugs were administered. All patients were given injection of glycopyrrolate 0.2 mg i.v.. Patients received propofol 1.5 mg/kg i.v. or ketamine 0.8-1.2 mg/kg i.v., as per their randomization to the two groups. Muscle relaxation was achieved with injection of succinylcholine 0.3-0.5 mg/kg. After succinylcholine-induced fasciculation was over, the patient was handed over to the psychiatrist for the procedure. The ECT was applied to the head through two electrodes kept on both sides of the temporal-frontal regions (bitemporal ECT) after applying ECT gel onto the electrodes. Modified ECT was given to all patients in the study using a pulse of 60 Hz of 0.8 ms duration with a total stimulus time not exceeding 1.25 s.The vital parameters were recorded before induction of anesthesia(baseline) and after applying ECT. The motor seizure duration was recorded by the psychiatrist through the right arm cuff method using a stopwatch. The EEG graph was recorded and displayed on the ECT machine and later the stored graph was analyzed by another experienced psychiatrist not involved in the ECT procedure to determine the EEG seizure duration. The assessment of recovery was done based on time for eye-opening on command. Post-procedure the patients were shifted to the post-anesthesia care unit and any adverse effect such as nausea, vomiting, respiratory depression,and hypoxemia was noted and managed as per the directions of the anesthesiologist.
2.6. Statistical analysis
Sample size calculation based on a previous study[10] to detect a significant difference in EEG seizure duration (α=0.05, power=80%)indicated that 22 patients were needed in each group. Thus, we considered at least 6 s difference between the means of EEG seizure duration to be clinically relevant and considering the other factors remain the same as per the previous study[10]. With α=0.05 and power of 80% with μ1=36.75 and μ2=42.75 and SD1=8.84 and SD2=5.50, the minimum required sample size is 22 in each arm.
The entire data is statistically analyzed using Statistical Package for Social Sciences (SPSS ver. 22.0, IBM Corporation, USA) for MS Windows. The descriptive data were expressed as frequency and percentage, and qualitative. The inter-group statistical comparison of the distribution of categorical variables was tested using the Chisquare test or Fisher’s exact probability test for a 2×2 contingency table. The inter-group statistical comparison of means of continuous variables was done using the independent sample t-test. The significant level of this study was set at α=0.05.
3. Results
The efficacy of propofol and ketamine in modified ECT was studied in 44 patients from May 2019 to May 2020 (Figure 1). The demographic and baseline information were comparable between the two groups (Table 1).
The majority of patients were of depressive disorders. The mean dose of propofol and ketamine used was (105.68±25.27) mg and(81.36±24.55) mg, respectively. The motor seizure and EEG seizure duration (s) were prolonged in the ketamine group (46.45±6.89 v.s. 32.73±8.58 and 61.27±9.22 v.s. 44.27±10.00, P<0.001). The baseline hemodynamic indices like systolic blood pressure (SBP),diastolic mean blood pressure (DBP) and mean blood pressure,oxygen saturation (SpO2), and heart rate (HR) were comparable(Table 1) whereas the distribution of mean maximum intra-operation SBP was significantly higher in the ketamine group compared to that of the propofol group (P<0.05) (Table 2). In propofol group,1 (4.5%) had vomiting and 2 (9.1%) had a headache. In ketamine group, 2 (9.1%) had vomiting and 1 (4.5%) had a headache, and there was no significant difference between the two groups. Besides,the propofol group showed a significantly shorter time to open eye(P=0.001)(Table 3).

Table 1. Demographic and baseline clinical characteristics of the two groups.
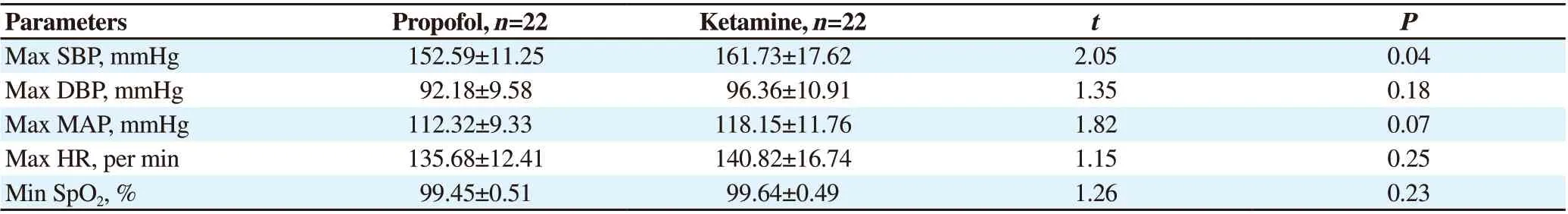
Table 2. Hemodynamics outcomes during electroconvulsive therapy.

Table 3. ECT outcomes and complications between the two groups.
4. Discussion
Since the introduction of anesthesia in ECT, the selection of anesthetic drugs remained a matter of discussion and controversy. There is always an ongoing search for an ideal anesthetic for ECT which will work instantly and for a brief period, not affect the seizure duration or quality of ECT, and will have minimum impact on the patient’s hemodynamic profile[4,6]. There are innumerable studies that compared different drugs in terms of their effect on seizure duration, hemodynamics, awakening time, and complications. Methohexital is the first intravenous anesthetic used in ECT and because of its safety, less effect on seizure duration,and low cost, it remained the gold standard for many years[11,12]. The use of methohexital was stopped until the introduction of alternatives like thiopentone, propofol, etomidate, ketamine, and recently ketofol[(1∶1 mixture of ketamine (10 mg/mL) + propofol (10 mg/mL)][13-16].
Hoyer et al. compared the impact of ketamine, thiopental, etomidate,and propofol on seizure parameters and quality in a retrospective study[17]. Yalcin et al. compared propofol, ketamine, and ketofol along with motor seizure quality, and they also compared duration for eyeopening, obeying a command, and hemodynamics[16]. Wang et al.used propofol, ketamine, and ketofol in their study to compare EEG seizure duration[10]. In their review article, Stripp et al. reviewed 80 articles to compare etomidate, ketamine, propofol, and ketofol for seizure quality and duration[18]. Jaitawat et al. compared propofol,etomidate, and Ketofol[19]. From these studies we have chosen the 2 most common drugs generally used in our center i.e., propofol (1.5 mg/kg) and ketamine (0.8 mg/kg) in the dosage commonly used in these studies[10,18].
The result of this study is similar to the other studies. Yalcin et al. in their study of 90 patients found a statistically significant difference(P<0.001) in motor seizure duration between the propofol group[(29.3±5.1) s] and ketamine group [(37.2±3.2) s][16]. In a study by Wang et al., they found significantly longer EEG seizures in the ketamine group [(55.87±7.55) s] compared to the propofol group[(36.75±8.84)] s[10]. Hoyer et al. also had noted the motor and EEG seizures of [(23.9±10.8) s] and [(43.7±15.7) s], respectively for the propofol group and [(29.1±12.2) s] and [(44.6±17.5) s] for the ketamine group in their study. The seizure durations in the ketamine group were significantly longer (P<0.001)[17].
The intra-procedure hemodynamic status of the patients recorded in this study matches with the other studies of similar interest. In our study distribution of mean maximum intra-op SBP is significantly higher in the ketamine group [(161.73±17.62) mmHg] compared to the propofol group [(152.59±11.25) mmHg] (P<0.05). Yelcin et al.recorded induction MAP values significantly increased from baseline in the ketamine group whereas induction MAP values significantly decreased from baseline in the propofol group (P=0.001)[16]. Also, in the study by Hoyer et al., 47.3% of cases in the ketamine group witnessed SBP>200 mmHg in the postictal period in comparison to 7.1% of the cases in the propofol group (P<0.001)[17]. In our study, the maximum intra-op heart rate among the cases studied in the propofol group [(135.68±12.41) per min] and the ketamine group [(140.82±16.74) per min] did not differ significantly between the two study groups (P>0.05), though Yelcin et al. found induction heart rate in comparison to baseline significantly decreased in the propofol group and significantly increased in the ketamine group (P<0.001)[16]. Also,Hoyer et al. suggested in their studies patients in the propofol group had significantly lower maximal heart rate (101.5/min) compared to the ketamine group (130.2/min)[17].
The distribution of mean time to eye-opening of cases studied is significantly higher in the ketamine group compared to mean time to eye-opening in the propofol group (P<0.001). The observation of our study matches with the study of Yalcin et al. where there was a statistically significant (P<0.001) delay in eye-opening in the ketamine group [(538.8±43.2) s] in comparison to the propofol group[(413.1±19.8) s][16].
Similar to our study, adverse events registered in the study of Wang et al. also include headache, nausea, delirium, and hypertension but there was no significant difference between the propofol and the ketamine group in the occurrence of adverse effects[10].
There are some limitations to our study. Firstly, this study is from a single hospital so our results cannot be simply generalized to the entire general population in all aspects. In this study, we had accepted multiple ECT sessions on a single patient as separate ECTs and treated those sessions as the same, however, the seizure duration can differ in a single patient from the first ECT to subsequent ECTs. Ketamine nowadays has been widely recognized for its antidepressant effects but the assessment of the anti-depressant effect of ketamine was not carried out.
To sum up, different anesthetic agents modify the ECT procedure differently in terms of seizure duration after administering ECT shock,hemodynamics, time to eye-opening, and the antidepressant effects.propofol and ketamine both can safely be used as anesthetic agents for modified ECT with ketamine providing longer seizure duration with no hemodynamic instability or any significant complication.
Conflict of interest statement
The authors report no conflict of interest.
Funding
This study received no extramural funding.
Authors’ contributionsD.G. and K.S. collected and curated the data; K.S. and S.S. guide and concept of Study; S.S., S.B., and K.S. contributed to writing the manuscript; All authors read and approved the final manuscript.
 Journal of Acute Disease2022年3期
Journal of Acute Disease2022年3期
- Journal of Acute Disease的其它文章
- A rare fatal case of rabies coexisting with COVID-19
- Ophthalmovigilance in COVID-19: Retinal vascular occlusion
- Lymphocyte count and A-DROP score in COVID-19 patients: A retrospective observational study
- Knowledge, attitude, and practice of house officers towards COVID-19: A multicentered crosssectional study in Egypt
- Comparison of impact of adjuvant treatment of midazolam, fentanyl, and magnesium sulfate with intrathecal bupivacaine on block characteristics and postoperative analgesia in knee arthroplasty: A randomized clinical trial
- Sudden cardiac death in a case of Crohn's disease with COVID-19: A case report
