Importance of the creation of a short musculofascial tunnel in peritoneal dialysis catheter placement
INTRODUCTION
Peritoneal dialysis (PD) is a widely applied therapy for long-term renal replacement.During PD,a catheter is essential for infusion and drainage of the dialysate.PD catheter implantation is performed by inserting a catheter through the abdominal wall and positioning the tip in the pelvic cavity,which is an ideal drainage site.However,in some patients,the catheter tip may migrate postoperatively,leading to flow dysfunction.
According to the guidelines published by the International Society for Peritoneal Dialysis (ISPD) in 2019[1],a 2.5-cm long musculofascial tunnel beneath the anterior sheath of the rectus abdominis is suggested to orient the catheter tip in the pelvis using the shape-memory of the straight catheter,which was first described in 1981[2].Nevertheless,there is no current literature comparing the efficacy of this tunneling technique in reducing catheter migration with other procedures.Moreover,several studies[3-5] have described the “traditional” open surgical dissection technique without a musculofascial tunnel.However,those studies reported a higher catheter migration rate in comparison to other modified procedures,in which an additional skin incision[4] or supplementary sutures[5] were needed to “orient” the catheter downward.
In this study,we performed catheter insertion through the abdominal wall without a musculofascial tunnel before 2017 and noticed occasional catheter migration.In the subsequent year,we introduced the musculofascial tunnel technique as a routine procedure in our center.This retrospective study aimed to examine the efficacy of creating a short musculofascial tunnel beneath the anterior sheath of the rectus abdominis in PD implantation by comparing the catheter migration rates with those of PD implantation following the traditional procedure.
And in his heart were hidden chords, which might havesounded far out into the world if he had been placed anywhere elsethan in the fisherman s hut by the North Sea
MATERIALS AND METHODS
Patients
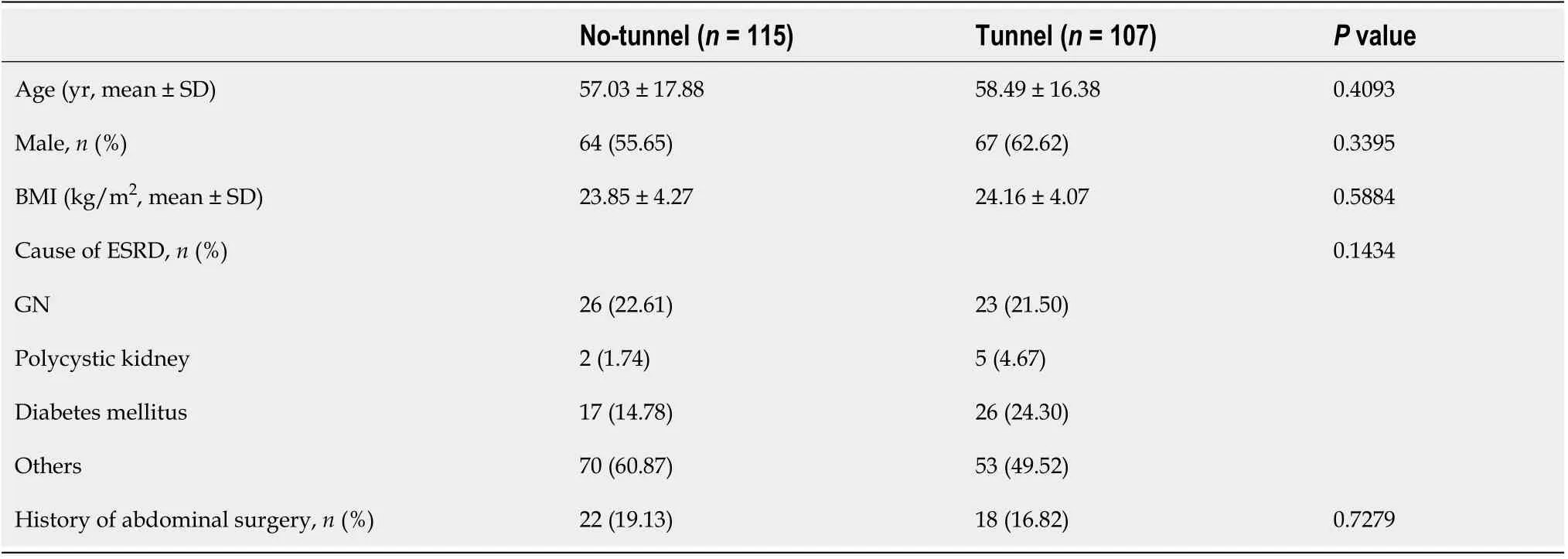
We retrospectively analyzed the medical records of patients who underwent PD catheter implantation from 2015 to 2019 at our hospital.The same surgical team performed all of the procedures,and all patients underwent open dissection surgery.Patients were divided into two groups:Patients who underwent catheter implantation without a musculofascial tunnel before 2017 and those who underwent the modified procedure with a tunnel after 2017.This retrospective study was approved by the Research Ethics Committee of NTUH (202106072RINA).
Operation
But the hermit bade him call the man who had the fog in his sack, and the sack was opened and the fog flew out, and hung right round the king s ships, so that they could see nothing
Various current modifications for open surgery[4,5] involve performing additional incisions or sutures to extend the catheter route,reducing malfunction episodes,and prolonging catheter survival.However,our musculofascial tunnel modification required only a brief extension of surgical time and did not necessitate a significant procedure alteration.In addition,according to our experience,there is no need to make a long skin incision for the tunnel.
Measurement of the catheter angle
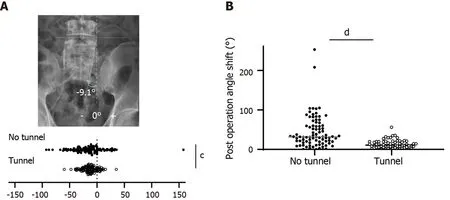
Postoperative plain film radiographs were reviewed to determine the angle of the catheter (Figure 2A).The catheter was placed into the pelvis perpendicularly during the procedure (ideal angle 0°).The angle of the catheter was calculated based on the axis of the catheter 5 cm below the deep cuff.All patients underwent radiography on the same day of the operation.We also reviewed all available radiographs taken within 2 years following the implantation.All angles of the catheter direction were recorded.The maximal migration angle was defined as the maximal disparity between any two measurements within the 2 years.
Catheter survival
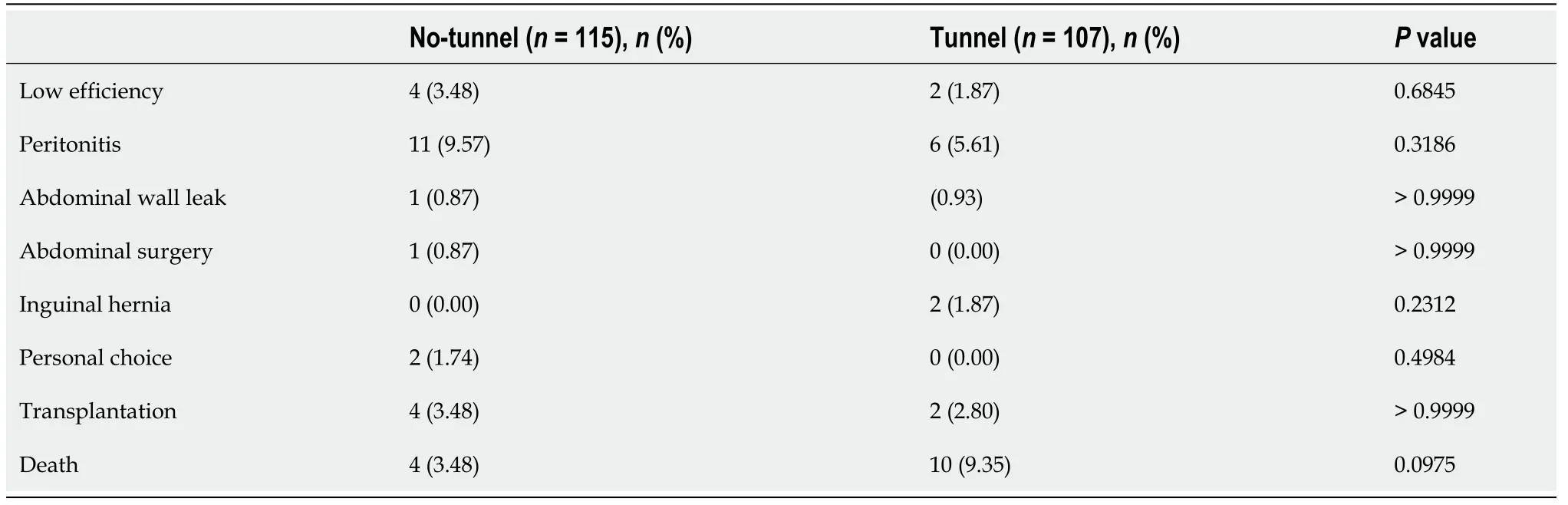
Overall catheter survival was determined at the time when patients discontinued PD for any reason.Therefore,patients were included if catheter function remained normal,but PD was ceased due to factors not attributed to the catheter itself,such as death,transplantation,personal choice,inguinal hernia,or subsequent abdominal surgery.The data of patients included in this category were censored.
47. Fattened so slowly: Trickery is one of the most popular methods for dealing115 with the evil in fairy tales. This implies that the trickster has experienced and accepted evil within him or her self, allowing insight into the strategy of the adversary116 (Jacoby 1992).Return to place in story.
Statistical analysis
Continuous variables are presented as mean ± SD.A two-sample-test with Welch’s correction was used to compare nominal data sets.Data proportions were compared using Fisher’s exact test.Two-sidedvalues<0.05 were considered statistically significant.We presented the data using Kaplan-Meier curves for the overall and functional catheter survival rates and analyzed them using a log-rank test.Statistical analysis was performed using the software GraphPad Prism 9.1.0 (GraphPad Software,LLC,CA,United States).
RESULTS
Demographic data of the patients
It was only then that I realized I did not teach my father. He taught me. It was he who had engaged me in the conquest of language. It was he who told me to be direct, to be watchful25, to listen with my eyes and to ask with my mouth. From his silence, my father taught me the true power of speech.
Postoperative position of the catheter
49.A thousand civilities:Cinderella s ability to graciously interact with her stepsisters highlights her charm and goodness while emphasizing the stepsisters vanity. They are unable to recognize the very woman who helped them dress for the ball a short time earlier.Return to place in story.
Catheter migration in the 2 years following surgery
All patients had at least one radiograph taken in the two-year period following catheter placement.Patients who underwent catheter placement with an associated musculofascial tunnel displayed a significantly lower shift in the catheter angle than the patients who underwent catheter placement without a tunnel (Figure 2B,13.48 ± 10.7144.34 ± 41.29°,<0.0001),implying that the catheter tip remained more stable in the pelvic cavity when the musculofascial tunnel was created.
On the day before Christmas, snowflakes mingled11 with the howling wind. As the pastor unlocked the church doors, he noticed an older woman standing12 at the nearby bus stop. He knew the bus wouldn’t be there for at least half an hour, so he invited her inside to keep warm.
Catheter complications
Dysfunction of the catheter due to migration was observed in four patients over the two-year follow-up period,and all affected patients were in the no-tunnel group.In addition,both groups had two cases of catheter obstruction due to omental wrapping.PD was resumed successfully in all four patients following laparoscopic omentectomy.
Catheter survival
I shall take good care to keep by your side, and when the right fish comes I will give you a little push, and with that you will seize the fish and cut it up

DISCUSSION
Catheter migration is a common complication following catheter implantation,with a reported incidence of 10%-30%[6,7].This retrospective study demonstrated that PD catheter orientation was improved by creating a short musculofascial tunnel.Further,this tunnel helped maintain catheter position within the pelvis of all patients throughout a two-year follow-up period.In contrast,four patients in the no-tunnel group (3.4%) experienced catheter dysfunction due to migration.
At the end of the two-year follow-up period,more than 70% of patients in both groups continued PD (Figure 3).The most common reasons for discontinuation were peritonitis and death (Table 2).After censoring the causes of discontinuation that were not attributed to the catheter (mentioned above),we performed a “function” survival analysis of the catheter,which revealed a two-year survival rate of 88.90% and 84.79% in the tunnel and no-tunnel groups,respectively.Although the survival curve seemed superior in the tunnel group,the difference was not statistically significant (=0.3799).
That s dumb, he said. You hardly need a costume. You re already a perfect scarecrow! I was used to these observations. Furthermore, he spoke2 the truth. At twelve, I was already six feet tall and weighed eighty-nine pounds. Tack3 on red hair and freckles4 and it added up to one thing: I was a scarecrow.
This study included 222 patients who underwent PD catheter implantation from 2015 to 2019.Among these patients,115 underwent the procedure without a musculofascial tunnel before July 2017,and 107 underwent the modified procedure with a tunnel starting from August 2017.There was no difference in age,sex ratio,or primary renal disease incidence between the no-tunnel and tunnel groups (Table 1).In addition,no differences in body mass index or abdominal surgery history were observed between the two groups.
Laparoscopic surgery is also a practical method for rectus sheath tunneling or preperitoneal tunneling[8] to prevent catheter migration.However,general anesthesia with a muscle relaxant is necessary for laparoscopy,increasing anesthesia-related risk and prolonging perioperative preparation.Moreover,laparoscopic surgery is associated with additional costs for anesthesia and surgical instruments.
We suggest placing the catheter approximately 1.5 cm outside the purse-string suture of the peritoneum with the inner cuff just beneath the anterior fascia.This placement allows the catheter to be well fixed away from the peritoneum,thus preventing possible peritonitis induced by a tissue reaction around the deep cuff[9].In addition,when discontinuing the use of the catheter,it is easier to remove the inner cuff in the presence of a musculofascial tunnel because the cuff lies superior to the rectus abdominis.On the contrary,the inner cuff is buried deeply in the rectus abdominis near the peritoneum in the no-tunnel method.Thus,increasing the risk of injuring the peritoneum and intestines during removal of the cuff due to extensive dissection.
This study had several limitations.First,this was a retrospective study conducted in a single center.As patients underwent different procedures in two separate periods,bias in patient selection and care was inevitable.However,we compared the patient characteristics between the two groups,and there were no significant differences in terms of kidney disease status and factors related to surgical concerns.In addition,all operations were performed by the same surgical team (Lee CY and Chen CC).Therefore,perioperative preparation and surgical materials remained unchanged throughout the study;thus,we believe that bias was minimal although present.Second,the patients in the study had an average body mass index of 24 kg/m,which is similar to that of most Asians but lower than those of Europeans and Americans[10].The thickness of subcutaneous adipose tissue is critical for determining incision length,and deep subcutaneous adipose tissue may result in technical difficulty during open surgery.Further investigation involving patients with a high body mass index is needed in the future.
The absolute value of the catheter angle was significantly smaller in the tunnel group than in the no-tunnel group (15.51 ± 11.3025.00 ± 23.08°,=0.0002).Moreover,there were fewer cases of catheter migration greater than 45 in the tunnel group than in the no-tunnel group (1.87%13.04%,=0.0018).
CONCLUSION
The results from this study provide evidence supporting the ISPD guideline for improving the quality of PD care.However,the addition of a short musculofascial tunnel,a simple but usually neglected step in catheter implantation,helped tilt the catheter and orient it downward toward the pelvis,which reduced catheter migration and prevented catheter dysfunction.This preemptive modification does not require specialized training,and therefore,can be readily adopted by surgical teams.
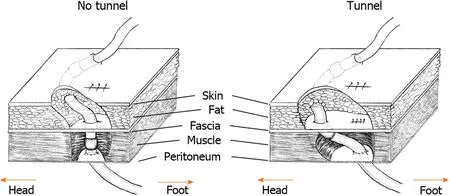
All patients received local anesthesia with intravenous sedation.The left side was preferred for surgery as the patients might be considered for future kidney transplantation using a right-sided approach.A 2–3-cm vertical incision was made over the lower rectus abdominis,and a small opening was created over the anterior sheath at the lower part of the incision.We then split the rectus abdominis bluntly to open the posterior sheath and peritoneum.After placing a purse-string suture,a 41 cm straight catheter with two cuffs (Covidien,Mansfield,United States) was inserted blindly toward the pelvis.In the no-tunnel group,the catheter was extracted from the rectus abdoministhe same opening in the anterior sheath,and the deep cuff was left in the muscle layer (Figure 1,left).In the tunnel group,we pierced the anterior sheath approximately 1-2 cm superior to the previous opening to extract the catheter and left the deep cuff beneath the sheath (Figure 1,right).A subcutaneous tunnel was created similarly in both groups to exit the site and orient the catheter downward.
ARTICLE HIGHLIGHTS
Research background
Creation of a musculofascial tunnel is usually neglected in the procedure of peritoneal dialysis catheter implantation.
Research motivation
We would like to see if the tunnel reduces catheter migration.
Research objectives
Patients undergoing peritoneal dialysis implantation with or without a musculofascial tunnel were retrospectively reviewed.
Research methods
Plain film after catheter implantation were reviewed to compare the migration angle.
Research results
Patients with the musculofascial tunnel had lower migration rate.
Research conclusions
Creating of a musculofascial tunnel is an important step for reducing catheter migration.
Research perspectives
Long term follow up is need for the function survival benefit.
The authors would like to acknowledge the peritoneal dialysis team for providing clinical support with the surgical procedures.In addition,we thank Mr.Shi-Yi Yang for his assistance with the statistics used in this report.
 World Journal of Clinical Cases2022年4期
World Journal of Clinical Cases2022年4期
- World Journal of Clinical Cases的其它文章
- Surgical treatment of acute cholecystitis in patients with confirmed COVID-19:Ten case reports and review of literature
- Rituximab as a treatment for human immunodeficiency virusassociated nemaline myopathy:What does the literature have to tell us?
- Eustachian tube involvement in a patient with relapsing polychondritis detected by magnetic resonance imaging:A case report
- Endoscopic clipping for the secondary prophylaxis of bleeding gastric varices in a patient with cirrhosis:A case report
- Inflammatory myofibroblastic tumor after breast prosthesis:A case report and literature review
- Langerhans cell histiocytosis presenting as an isolated brain tumour:A case report
