Recurrent ovarian endometrioma after conservative surgery: A retrospective study
Kuntima Kantawee, Woraluk Somboonporn
Department of Obstetrics and Gynecology, Faculty of Medicine, Khon Kaen University, 40002, Thailand
ABSTRACT
Objective: To study the prevalence and associated factors of recurrent ovarian endometrioma after ovarian cystectomy.
Methods: This retrospective study analyzed 303 patients who underwent cystectomy for ovarian endometrioma and had at least a 2-year follow-up at Srinagarind Hospital from January 2013 to December 2018. The patients were divided into the recurrent and nonrecurrent groups according to the findings from postoperative transvaginal ultrasonography 6 months after undergoing surgery.Nineteen factors were collected for risk evaluation. The prevalence of recurrent ovarian endometrioma and its 95% confident interval(CI) were calculated. Univariate and multivariable logistic regression analyses were performed to determine the association between factors and recurrence.
Results: Recurrent ovarian endometrioma occurred in 33%(95% CI 27.7%-38.3%) patients. The median duration of followup was 36 months. during the median follow-up period of 36 months. Preoperative history of parity, preoperative infertility history, endometriosis surgery, moderate to severe dysmenorrhea,dyspareunia, intraoperative stage 4 according to revised American Society for Reproductive Medicine classification, presence of adenomyosis, and postoperative pain relief were associated factors based on univariate analysis. In contrast, infertility [odds ratio (OR)2.22, 95% CI 1.14-4.33], moderate to severe dysmenorrhea (OR 2.13,95% CI 1.09-4.15), and postoperative pelvic pain relief (OR 0.22,95% CI 0.12-0.42) were independently associated factors based on multivariable logistic regression analysis.
Conclusions: In our setting, preoperative infertility history and moderate to severe dysmenorrhea were associated with a higher recurrent ovarian endometrioma risk. In contrast, postoperative pain relief was significantly associated with lower recurrence risk.
KEYWORDS: Endometriosis; Recurrent ovarian endometrioma;Associated factors; Conservative surgery; Gynecologic surgical procedures; Prevalence; Cystectomy; Prognosis; Risk factors
Significance
Recurrent rates of ovarian endometrioma vary from 9.6%-33.1%. A high recurrent rate was previously reported by many studies conducted in training centers. Finding of the high recurrent rate in our university hospital adds another evidence that several levels of surgical skill partly contribute to the rate of recurrence. Our findings on associated factors suggest that the actual risk factors of recurrent ovarian endometrioma may be unique for each study center.
1. Introduction
Endometriosis prevalence is roughly 10% globally[1] and significantly impacts women and societies across different countries and ethnicities[2]. The Global Study of Women’s Health has demonstrated that each affected woman lost around (10.8±12.2) hours of work a week, mainly due to diminished work effectiveness[2]. Loss of work productivity amounted to substantial costs per woman weekly, ranging from US$4 in Nigeria, a lowermiddle-income country, to US$456 in Italy, a high-income country[2].
Endometriosis is a chronic disease, and endometriomas, a more severe form, can present additional long-term complications[3].Treatment of ovarian endometriomas is likely effective for patients temporally; though, the ovarian endometrioma has a high recurrent rate post-treatment[3]. In Asian countries, the reported recurrent rates vary from 16.2% to 26.1%[4-7]. In concordance, the recurrent rates in European countries vary from 9.6% to 33.1%[8,9]. For a significant number of recurrent cases, preventive strategy is crucial and includes appropriate surgical techniques and postoperative medical therapy, as suggested in a guideline by the European Society of Human Reproduction and Embryology[10]. Results from the most recent systematic review and network meta-analysis have confirmed that long-term use of hormonal treatment had a significantly lower risk of endometrioma recurrence than expectant treatment[11].
Examining risk factors associated with recurrent endometrioma is another area of interest, particularly in countries with limited resources. If the risk factors could be documented, investing in preventive intervention specific to those at risk will reduce disease recurrence and thus reduce the cost of treatment associated with disease recurrence. In our extensive review, the severity of disease, commonly classified by the revised American Society for Reproductive Medicine (rASRM) score, was found the most frequently associated factor for recurrent endometrioma in both high-income and upper-middle-income countries[4,8]. Age at surgery and severity of dysmenorrhea have also been reported as common associated factors[5,6,9,12].
Race and ethnicity differences may also differently affect recurrent ovarian endometrioma[13]. As a result, it would be beneficial to determine the prevalence of recurrent endometrioma and explore risk factors associated with recurrent endometrioma in Thailand. Hence,the study was to determine the prevalence and associated factors of recurrent ovarian endometrioma after ovarian cystectomy. This study may help us develop an appropriate program for a cost-effective,preventive strategy in the future.
2. Material and methods
2.1. Patients
This retrospective study was composed of 303 women, aged 20–50 years old, who underwent conservative cystectomy by either laparoscopy or laparotomy as a treatment for ovarian endometrioma during January 2013–December 2018 at Srinagarind Hospital,Khon Kaen University, Thailand. All included patients had histopathological confirmation of ovarian endometrioma and had a minimum follow-up of 2 years. We excluded patients who had gynecologic cancer or underwent oophorectomy or hysterectomy.Patients with incomplete information in medical records were excluded. After operation, the first follow-up visit was one month.The subsequent appointments varied from one to six months according to doctor preference and patient symptoms. In each follow-up visit, the patient was assessed for clinical symptoms.Per-vagina examinations were performed based on the clinician’s judgment. Decisions to perform transvaginal ultrasounds were made and performed by board-certified gynecologists. However, pervaginal examination and transvaginal ultrasound were performed in all included patients at least every six months.
2.2. Surgery
The type of operation performed (either laparoscopy or laparotomy)was agreed upon by the patient and doctors, with the decision based on several factors, such as whether there was a previous abdominal operation, the severity of the disease, individual surgeon experience,economic status, and health care insurance. The surgical procedures were performed by either staff or third-year resident doctors of the gynecologic department or the reproductive medicine unit fellows.However, every operation was performed under staff responsibility.
2.3. Data collection
A total of 886 medical records were reviewed against the inclusion and exclusion criteria and then 583 records were excluded due to their ineligibility. With the remaining records, we independently extracted demographic data, preoperative endometriosis-related symptoms, intraoperative findings such as rASRM stage, evidence of deep infiltrating endometriosis, and endometrioma side and diameter into data collection form. Postoperative information regarding pelvic pain, pregnancy, and medication was also recorded. Then we doublecomputed the pertinent data into Excel to prevent imputing errors.
2.4. Sample size
The sample size was calculated using a formula for determining a proportion in a single proportion. The formula was n = z21-a/2 p(1-p)/d2. The imput alpha error was 0.05 and beta error was 0.05.The imputing prevalence of recurrent endometrioma was adopted from Tanprasertkul et al[14], and as a result, the total required sample size was 303 patients.
In Srinagarind Hospital, patients underwent surgery with endometriosis around 160 cases per year. Due to 30% of treated patients were transferred back to the primary healthcare, we decided to include the eligible patients during 2013-2018 by quota sampling.Therefore, when the recruitment of eligible women was complete,we then ended the enrollment.
2.5. Variables
Recurrent cysts were defined as cysts detected any time after 6 months post-surgery with the following ultrasonographic findings: a unilocular cyst (or multi-loculated cysts) with acoustic enhancement and diffuse homogeneous ground-glass echoes as minimum criteria, no papillary projections, and persist either for at least two consecutive menstrual cycles or, in the cases with a missed period caused by postoperative hormone therapy, one month.Diagnoses of recurrent endometriomas were made by board-certified gynecologists. The control group was nonrecurrent endometrioma cases during the follow-up period.
Deep infiltrating endometriosis was acknowledged if one of the following criteria were recorded in operative findings: 1) direct visualization of a deep pelvic endometriotic lesion that, if biopsied,showed only fibrosis or, if not biopsied, was proven histologically to have at least one other site of endometriotic involvement; 2)complete cul-de-sac obliteration secondary to endometriosis.
Dysmenorrhea severity was noted in the medical charts as a visual analog scale (VAS) score. We then classified the VAS score (0 to 10)into four severity levels: 0 as no pain, 1-4 as mild, 5-7 as moderate,and 8-10 as severe.
2.6. Statistical analysis
For descriptive data synthesis, mean±standard deviation (mean±SD), median [interquartile range (IQR)], or percentage would be presented as appropriate. The recurrent rate was presented as a percentage and 95% confident interval (CI). Testing the differences of demographic data between the recurrent and the nonrecurrent groups was performed by either an independent t-test or Wilcoxon rank-sum test for continuous data and by either a Chi-square test or Fisher’s exact test for categorical variables. In addition, logistic regression was used to evaluate the associated factors for recurrent endometriosis. We included the meaningful factors retrieving from literature review and the variables with P value less than 0.05 under univariate analysis into the model. These factors were infertility,the endometrioma diameter, preoperative dysmenorrhea severity,preoperative dyspareunia, rASRM stage, adenomyosis presence,postoperative pelvic pain relief, and postoperative hormone treatment. Statistical analysis was performed using the Stata statistical softwareversion 10.1 (StataCorp. 2007. Stata Statistical Software: Release 10. College Station, TX: StataCorp LP., KKU Licenses). The level of statistical significance was defined as P<0.05.
2.7. Ethical approval
This study was approved by the Center for Ethics in Human Research, Khon Kaen University (ethics approval No. HE631412),with Clinical Trial Registration: Thai Clinical Trials Registry TCTR20210911001.
3. Results
3.1. Characteristics of the included patients
We screened 886 medical records; 583 were ineligible. Of 583 excluded cases, 324 cases underwent oophorectomy, 14 cases underwent hysterectomy, 17 cases were ovarian cancer and 228 cases were either lost to follow-up or transferred back to their nearby hospital. Of 303 included patients, all pertinent data were used for analyses (Figure 1).

Figure 1. The study flowchart.
The mean age was (33.2±6.2) years. The median gravida, parity,and body mass index were 0 (IQR: 0, 1), 0 (IQR: 0,1), and 20.8 kg/m2(IQR: 19.1, 23.5), respectively. Previous cesarean section and previous other abdominal surgeries were performed in 34(11.2%) patients and 67 (22.1%) patients, respectively. One hundred and ninthy-one (63%) patient were infertility. The median of dysmenorrhea severity (VAS score) was 6 (3, 8). The laparotomy was performed in 83 (27.4%) patients. Postoperative medication was used in 188 (62%) patients and the median duration of medication was 6 (IQR: 0, 24) months. The most commonly used medication was progestin in 106 (35%) patients. The median follow-up period was 36 months (IQR: 24-60 months) (Table 1).
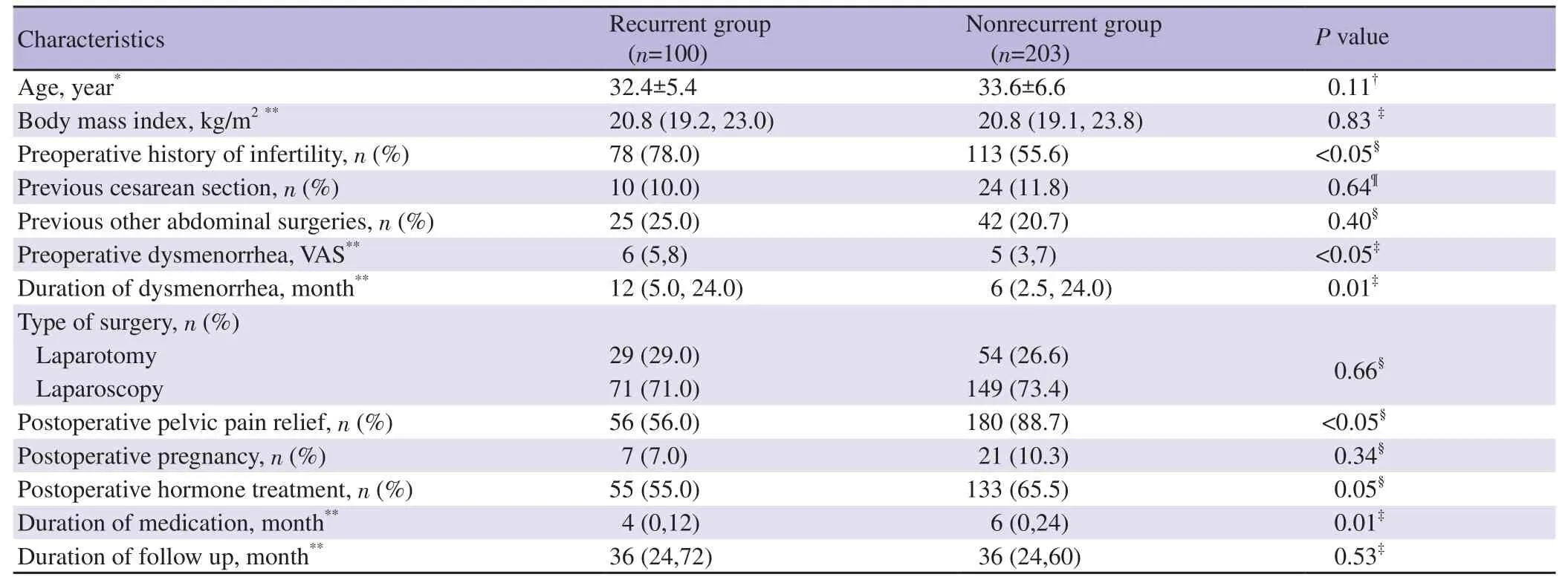
Table 1. Baseline demographic, medical history and type of surgery of patients in the recurrent endometrioma and nonrecurrent endometrioma groups.
The median of the largest-diameters of endometrioma was 5 cm(IQR: 4, 6). One hundred and forty-seven (48.5%) patients had stage 4 endometriosis according to rASRM classification. The operative finding recorded of 103 patients (34%) had complete culde-sac obliteration and 19 patients (6.3%) had deep infiltrating endometriosis. Leiomyoma was recorded in 65 patients (21.5%) and adenomyosis in 40 patients (13.2%) (Table 2).
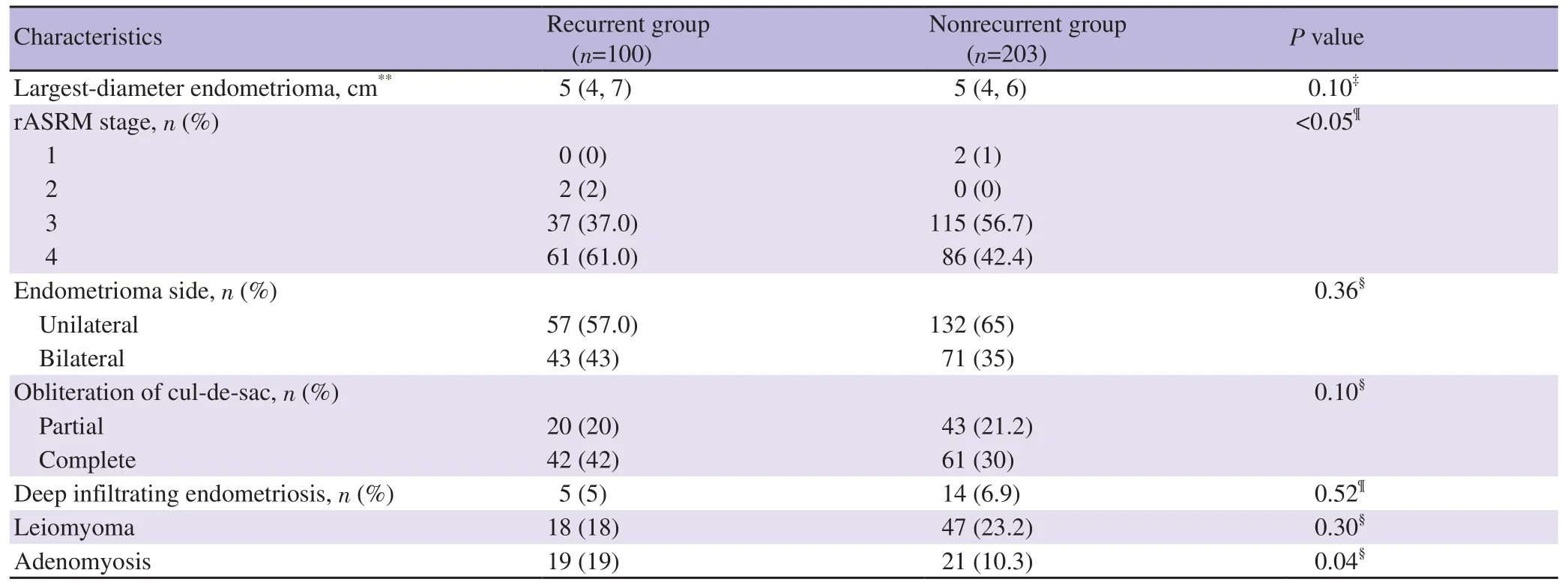
Table 2. Intraoperative findings of patients in the recurrent endometrioma and nonrecurrent endometrioma groups.
3.2. The prevalence rate of recurrent ovarian endometrioma
Recurrent ovarian endometrioma occurred 33% (100/303) (95% CI 27.7%-38.3%). The recurrent and nonrecurrent groups were similar in the age at the surgery, menarche, and gravida. The characteristics that differed between the recurrent and nonrecurrent groups are shown in Table 1. Infertility, dysmenorrhear severity, duration of dysmenorrhea, postoperative pelvic pain relief, and duration of medicatiom were different between the two groups (Table 1).
3.3. Associated factors of recurrent ovarian endometrioma
When we examined potentially-associated factors for recurrent endometrioma by univariate analysis, the significant factors were infertility [odds ratio (OR) 2.82, 95% CI 1.63-4.89], preoperative moderate and severe dysmenorrhea (OR 3.28, 95% CI 1.79-6.00),preoperative dyspareunia (OR 2.10, 95% CI 1.27-3.49), previous surgery for endometriosis (OR 2.38, 95% CI 1.01-5.60), rASRM stage 4 (OR 2.13, 95% CI 1.31-3.47), adenomyosis presence (OR 2.03, 95% CI 1.04-3.99), postoperative pelvic pain relief (OR 0.16,95% CI 0.09-0.29) and postoperative progestin use (OR 0.53, 95% CI 0.30-0.95) (Table 3).
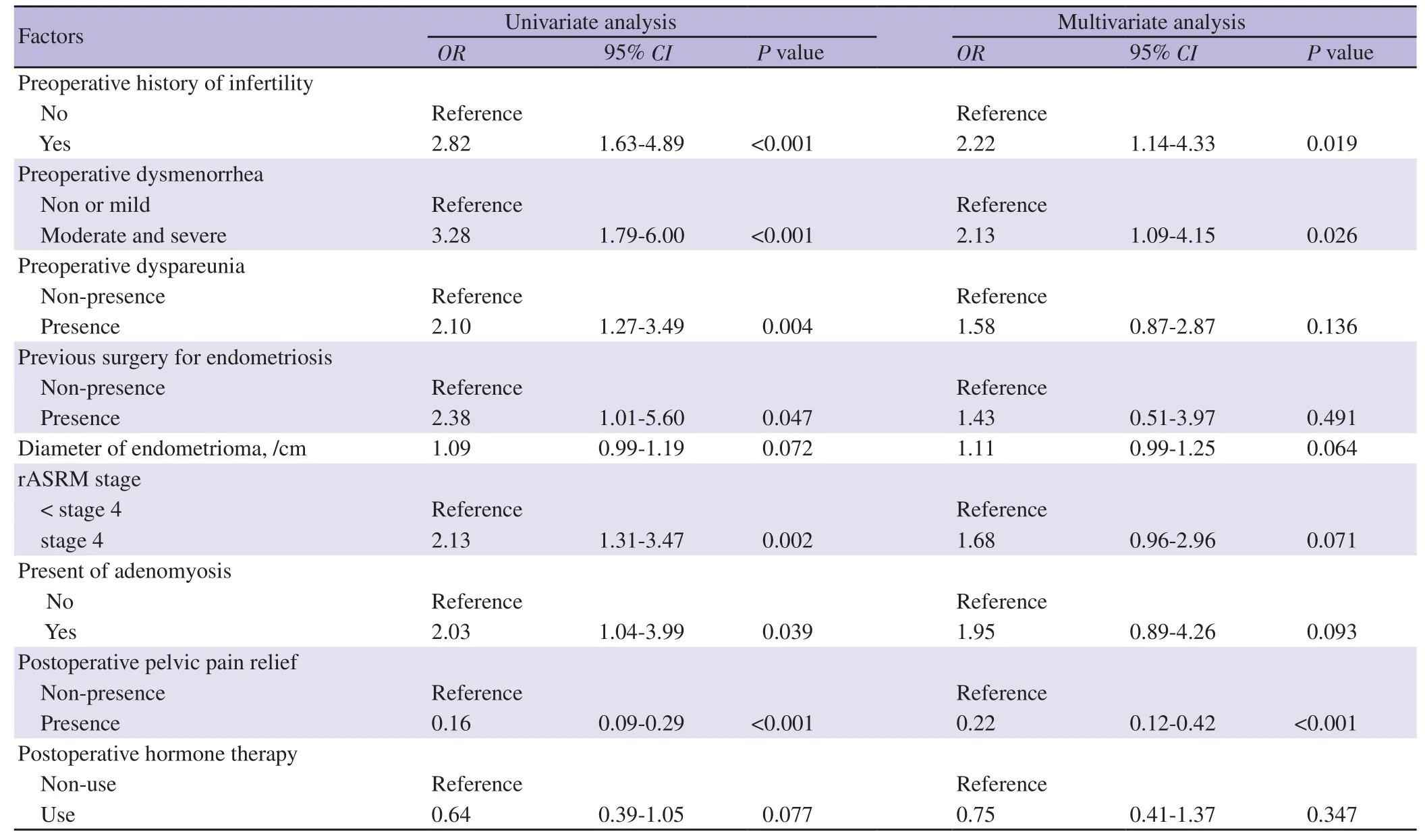
Table 3. Assessment for associated factors of the recurrent endometrioma and nonrecurrent endometrioma groups.
However, multivariable logistic regression analysis found that preoperative dyspareunia, previous surgery for endometriosis,rASRM stage 4, adenomyosis presence, and postoperative progestin use were no longer associated with the recurrent endometrioma.The independent significant associated factors for higher recurrent endometrioma were infertility and moderate and severe dysmenorrhea before surgery, and postoperative pelvic pain relief was associated factor of lower recurrent endometrioma (Table 3).
4. Discussion
In this study, the prevalence of recurrent endometrioma was 33%(95% CI 27.7%-38.3%), higher than that in most previous studies in Asiaand, comparable to the 33.1% that Kucukbas et al[9] showed but lower than the 45.1% that Hayasak et al reported[15]. Taking a closer look at the settings from which the studies data were collected, we find that the settings for our study and the study of Hayasaka et al[15]were both in university hospital, while for the study of Kucukbas et al[9], it was a training center. In these settings, one would expect to find varying surgical skill levels[9,15]. In contrast, the study by Lee et al reported a recurrent endometrioma prevalence of only 8.3% in an average of 32 months of follow-up, and it included 22 surgeons experienced with more than 300 cases of laparoscopic surgeries and more than 100 cases of laparotomies[16]. A study by Porpora et al reported a recurrent prevalence of 9.6%, and ovarian cystectomies were performed by a senior surgeon[15]. The above findings suggest that recurrent endometrioma prevalence is likely impacted by surgeon experience.
In this study, based on the multivariable analysis findings,preoperative history of infertility and moderate to severe dysmenorrhea were associated with a higher risk of recurrent ovarian endometrioma, whereas postoperative pelvic pain relief was associated with a lower risk. Comparable to our study, several retrospective studies and a systematic review of retrospective studies found preoperative dysmenorrhea a consistent risk factor; however,three retrospective studies did not show this association[8,17,18]. In contrast, several retrospective studies reported that infertility was not associated with recurrence and the systematic review of retrospective studies indicated above by Jiang et al did not evaluate infertility[12,18-21]. Consistent with our findings, the study of Tobiume et al reported that postoperative pain improvement contributed to an 80.9% accuracy rate of predicting recurrence[4]. Nevertheless, the study by Jiang et al did not assess this factor[21].
In our study, the number of patients who received postoperative hormone therapy with rASRM stage 3 and stage 4 was 60.5% and 64.6%, respectively (data not shown). In the univariate analysis, rASRM stage 4 and postoperative progestin therapy were factors related to a higher risk of recurrence. However, there was no significance after taking other factors into account in the multivariable model. For postoperative hormone treatment,a systematic review of 4 cohorts and 13 randomized controlled trials showed that there was a significantly decreased risk of endometriosis recurrence in patients who received postoperative hormonal suppression compared to those who received expectant management or a placebo [relative risk (RR) 0.41, 95% CI 0.26-0.65][22]. When the analysis was limited to six high-quality studies,the result still suggested that the recurrence risk was reduced (RR 0.36, 95% CI 0.18-0.72; 843 patients)[22]. As mentioned earlier, the systematic review of retrospective studies did not show a significant reduction[21]. One explanation for the contrary results of the two systematic reviews is that the type of included studies between the reviews varies[21,22]. If we refer to the hierarchy of evidence for therapeutic studies, the systematic review of randomized controlled trials is at level 1A, the highest level, while the systematic review of retrospective studies is at level 3A[23].
Regarding the level of evidence for risk factors, the results from the systematic review of retrospective studies are considered level 2[23]. The systematic review of retrospective studies showed that other factors related to recurrent ovarian endometrioma were age at surgery, serum CA125 level, cyst size, dysmenorrhea, endometriosisrelated surgery history, preoperative medication, rASRM score, and postoperative pregnancy[21]. In our study, endometriosis-related surgery history and intraoperative severity of endometriosis were factors related in univariate analysis but not in multivariable analysis.Age at surgery, the diameter of endometrioma, and postoperative pregnancy were not found factors associated with the recurrence in both univariate and multivariable models. After the systematic review, the retrospective studies were published by Han et al[5], Li et al[6] , and Lee et al[16]. The studies by Han et al[5] and Li et al[6]showed that younger age was a risk factor, while Lee et al[16] found that the endometrioma size was a risk. In addition, Li et al found that postoperative pregnancy was a protective factor for the recurrence with the RR of 0.649 (95% CI 0.460-0.914)[6]. We did not collect the serum CA 125 level and preoperative medication information, as we did not routinely measure the serum CA 125 level, and preoperative hormone was used for symptom relief in most patients due to the long surgery queue. In the systematic review, cyst diameter in the recurrent group was significantly larger than in the nonrecurrent group of 0.35 cm (95% CI 0.08-0.62)[21]. The mean rASRM score was 0.33 (95% CI 0.20-0.46) higher than those in the nonrecurrent endometrioma, while the mean level of CA 125 (U/mL) was 0.51(95% CI 0.14-0.88) higher. The mean age of the recurrent group was 0.51 (95% CI 0.14-0.88) years younger. As we know, the effect estimation calculated from a meta-analysis should be more accurate and precise due to the larger sample size created by pooling results from several studies[24]. However, statistically significant results may not always directly apply to clinical practice. Recognizing common risk factors may help identify patients at risk of recurrent ovarian endometrioma but how we can tell which patient would be likely to recur according to the results from the systematic review. Therefore,a predictive tool should be developed based on the best available evidence and then, for testing its applicability, validated in several settings.
Determining the actual risk factors of recurrent ovarian endometrioma is problematic for several reasons, such as variation across medical centers in clinical situations for treatment management (e.g., indicating surgery, deciding to start medical therapy, selecting a hormone treatment and surgical skill) and dissimilarity across studies in collecting factors to be assessed.Moreover, methods of statistical analysis also influence the study results. For example, in Thailand, Wacharachawana et al conducted a retrospective study in 106 patients who underwent laparoscopic ovarian cystectomy[25]. Based on univariate analyses, postoperative medical treatment (OR 3.15, 95% CI 1.14-8.74, P=0.02) and postoperative pregnancy (OR 2.86, 95% CI 1.03-7.93, P=0.04)were factors associated with recurrence reduction. The recurrence rate of ovarian endometrioma after laparoscopic cystectomy was 22.6%. Postoperative medical treatment and postoperative pregnancy significantly lowered ovarian endometrioma recurrence[25]. Although our studies were conducted in the same country, their results differed from ours.
The results of this study provide level 3 evidence for recurrent ovarian endometrioma risk factors. We established recurrent ovarian endometrioma-associated factors, such as infertility and moderate to severe dysmenorrhea, disease remission-indicating factors, such as postoperative pain relief, specifically for our center. Nevertheless,surgical skill is also essential. Hence, for further study, surgeon experience should be considered for analysis. A study limitation included retrospective data collection. If we prospectively collected the data, data collection may have been better standardized, which may have reduced any classification and detection biases.
Preoperative history of infertility, moderate to severe dysmenorrhea,and postoperative pelvic pain relief are factors identified as associated factors for recurrent ovarian endometrioma. Guidelines could be created around those factors for such beneficial actions as offering assisted reproductive technology for infertility couples or postoperative medication when appropriate.
Considering that it is highly likely that factors relating to recurrent endometrioma will depend on the specific treatment protocols,availability of investigative resources, medicine, surgical skill and other resources of individual health care centers, the generalizability of our results may be limited to a center with a similar setting.
In conclusion, recurrent ovarian endometrioma occurs 33%. History of infertility and severity of dysmenorrhea are associated with a higher risk for recurrent ovarian endometrioma in our setting. Pain relief after operation is significantly associated with a lower chance of recurrence.
Conflict of interest statement
The authors have no conflicts of interest to disclose.
Acknowledgments
We want to thank Mr. Kevin McCracken for his assistance with the English language presentation of the manuscript under the aegis of the Khon Kaen University Publication Clinic, Thailand. We want to thank Miss Kaewjai Thepsuthammarat, Clinical Epidemiology Unit, Khon Kaen University, for generously supporting the statistical analysis of this work.
Authors’ contributions
Kuntima Kantawee and Woraluk Somboonporn contributed to the design and implementation of the research, to the analysis of the results and to the writing of the manuscript.
 Asian Pacific Journal of Reproduction2022年1期
Asian Pacific Journal of Reproduction2022年1期
- Asian Pacific Journal of Reproduction的其它文章
- Successful live birth after intracytoplasmic sperm injection using testicular sperm in non-mosaic Klinefelter syndrome
- Effects of enzymatic and non-enzymatic antioxidants in diluents on cryopreserved bull epididymal sperm
- Taurine in semen extender modulates post–thaw semen quality, sperm kinematics and oxidative stress status in mithun (Bos frontalis) spermatozoa
- Blepharis persica increases testosterone biosynthesis by modulating StAR and 3 β-HSD expression in rat testicular tissues
- Uptake of in-vitro fertilization among couples attending fertility clinic in a tertiary health institution
- An implementation study of barriers to universal cervical length screening for preterm birth prevention at tertiary hospitals in Thailand: Healthcare managers’ perspectives
