The effect of Bach flower remedies on quality of life and sleep in hospital professionals during the Covid-19 pandemic
Carme Porcar-Castell, Neus Esmel-Esmel
1 Nursing supervisor. Hospital Universitari Sant Joan de Reus. Associate professor Faculty of Nursing (URV), Tarragona, Spain.
2 PhD, Associate professor Faculty of Nursing (URV), Tarragona, Spain.
Abstract:Background:Health-related quality of life and sleep are linked for hospital staff on the night shift. In the context of COVID-19 these workers have become a vulnerable group. The World Health Organization (WHO) warns that this pandemic is likely to have short- and long-term impacts on mental health. Despite the importance of this issue, there are few studies that propose strategies and interventions for coping and adapting to the situation. Objective:To evaluate the effectiveness of Bach flower therapy for improving the quality of life and sleep of night shift workers in the hospital setting during COVID-19. Methodology: Mixed methodology. Observational, analytical, longitudinal study, with case and control groups. A total of 150 health professionals who work on the night shift took part in the study, which consisted in participants taking Bach flowers orally. The SF-12v2, Oviedo Sleep Questionnaire, and an ad hoc questionnaire were applied pre and post intervention.Results: The mental health component, insomnia and emotion management, showed significant results in the intervention group (P = 0.007, n = 26) compared to the control group (P = 0.202) in mental health and in insomnia (P = 0.490, n = 34). Other results show that 82.6% of the sample suffers from insomnia, of which 13.3% have severe symptoms and 38% show risk of depression.Conclusion: Bach Flower Remedies demonstrated to be effective in improving night shift workers’ mental health component (measured with SF-12v2), insomnia and emotion management during the COVID-19 lockdown. Bach Flower Remedies could be used as a coping strategy in complex situations within the hospital setting.
Keywords:Bach flower remedies, COVID-19, Quality of life, Sleep, Night shift, Nursing
Introduction
The coronavirus has turned the world upside down and had a huge impact on the way of caring. Healthcare professionals have adapted to the new situation without time to even reflect on these changes. The population in lockdown, the state of alarm activated in most of the world and the deaths and infectious cases have increased the workload for health professionals. A lot of health services have collapsed, especially in hospitals, which has had an enormous impact on nurses as the workforce with the largest number of professionals involved in facing the pandemic. This has significantly influenced their quality of life.
Nursing staff's quality of life can be affected by the actions that are part of their daily practice, which make them more vulnerable to emotional destress when they come into contact with situations of suffering, anguish, pain and death. Gallagher (2013) shows that complex care can promote the onset of emotional stress, depression, anxiety, sleep loss and headaches. These situations are aggravated by repeated exposure to pain and suffering, failed attempts to alleviate suffering, and to the patient's traumatic situation [1]. If suffering continues it is possible to experience fatigue out of compassion, a term described by Joison [2] and of which we still know little despite its importance. Melvin [3] identified fatigue by compassion due to exposure to repeated deaths, a situation that has been at the forefront of the pandemic.
The effects of COVID-19 will impact the mental health of health care workers, especially nurses [4, 5] and those who have been in direct contact with the disease. Multicentre studies conducted in China on health workers during the pandemic, show that there is an association between physical symptoms and psychological states, as well as an increase in insomnia [6, 7] and other factors associated with mental health. The authors show that nurses in particular had their psychological burden increased and many reported symptoms of depression, anxiety and insomnia. Similarly, the study by Erquicia et al. [8] found that a significant percentage of health professionals reported symptoms of anxiety and depression as well as acute stress. However, the increase in cases, and the lack of adequate supplies and equipment, has generated even more pressure and anxiety [8-10] as well as fear of the contagion itself and transmitting the infection to relatives [11].
In addition, sleep disorders have been exacerbated by the pandemic, leading to major sleep alterations. Poor sleep quality is one of the factors that influences the perception of loneliness, increasing the risk of depression, anxiety, suicidal ideation and deteriorating mental health. Thimmapuran et al. [12] and Huang et al. [13], researched the mental health burden and sleep quality during Covid-19. The results showed that health workers had a high risk of poor sleep quality, a significant burden of loneliness, and a high risk of having psychological problems.
Different studies [15, 14-16] on night-shift professionals’ evidence that nursing staff suffer from sleep-related problems. Bonet Porqueras et al. [17] analysed the effects on the quality of life of Catalan nurses and showed that night shifts increase the incidence of insomnia and sleep interruptions. Night-shift work already involves a readjustment of circadian rhythms and has different side effects. Adding these to the stress of the pandemic context has resulted in a set of circumstances that are harmful to the health of hospital workers, especially in night work.
Looking at the current systematic reviews and meta-analyses [7, 18-20] we observe that they all emphasize the need to implement coping strategies and make them a public health priority. Erquicia et al [8] point out that health professionals are a vulnerable group in the COVID-19 pandemic and that hospitals should develop intervention plans for those professionals who require them, especially taking into account the possibility of future health emergency situations. Wu P et al. [21] show that coping strategies are essential for ensuring psychological well-being and sound and healthy clinical care. It is vital to support health workers in all aspects to maintain a good workforce, especially in the pandemic.
Regarding sleep problems, some authors [22] propose minimizing insomnia with vigorous walks combined with music, health education, sleep hygiene, cognitive behavioural therapy and mindfulness. Grover et al. [23], recommend good sleep hygiene, relaxation techniques, detoxification from social networks, group sessions, leadership and psychotherapy, among others. Other authors who have studied fatigue through compassion propose strategies focused on empowerment, training, and resting periods [24]. Other techniques have also been proposed, such as yoga, guided meditation, music therapy and resilience therapies [25].
Authors as Fusco and Solano [26, 27] conclude in their recently published studies that Bach's Floral Therapy improves patients' anxiety, sleep quality and Rescue Remedy was effective as emergency therapy.
Another important factor arising from these situations is that workers often neglect their self-care. Hernández-Garcia [24] believes it is necessary to raise health personnel’s awareness about the psychological problems that they may experience as a result of caring for people in a palliative situation. Vidal-Blanco et al. [28] state that it is necessary to delve deeper into the construct of self-care to counteract stressful emotional situations. Erquicia et al. [8] show the importance of professionals paying attention to their mental health by observing stress reactions and seeking support if necessary.
As we mentioned above, health workers have a high risk of seeing their mental health negatively affected, especially in situations following outbreaks of infectious diseases. Coinciding with the year of nursing, the COVID-19 pandemic has revealed the need to develop and carry out interventions and actions that improve the quality of life of these professionals; especially as the WHO warns that this pandemic is likely to have short- and long-term impacts on mental health. Despite the importance of this health problem, there are few studies that propose strategies for coping and adapting.
Bach Flower Remedies
Bach Flower Remedies (BFRs) are a modality of Complementary Medicine approved by the WHO in 1976, recognized by integrative medicine [29] and which are part of the set of energetic or vibrational medicines that, by means of harmonic frequencies, help correct patterns of imbalance through resonances [30]. The therapy considers the individual as a combination of mind, body and spirit and is popularly known as "Bach flowers". It consists of 38 natural remedies and one combination of five flower essences for emergencies (Rescue Remedy).
The essences are obtained by maceration and/or boiling of wild plants and trees. They are based on the healing power of nature and are linked to the world of emotions. Each flower has its own meaning that corresponds to personality traits, emotions and moods. These meanings allow us to identify the emotions and suffering of our experiences [31] as well as discover adaptive behaviours that can promote resilience to different situations [32].
Their therapeutic effects are not yet clear, a psycho-modulatory action has been proposed and immunomodulatory effects are also attributed to them, which are responsible for improving somatic symptoms [33]. Some authors [34] propose that the action mechanism is a reduction in sympathetic activity and an increase in parasympathetic activity. Other authors argue that it is due to a placebo effect [35] that unleashes the healing potential and which we could define as an ethical placebo [36]. De Souza et al [37] suggest that the central effects of flower remedies can be partially detected through pharmacological models used in the search for psychotropic agents, and propose that they may have a certain biological effect [38]. Rivas Suárez et al. [39] argue that in order to demonstrate their action, preclinical studies should be carried out similar to those used for synthetic drugs to delimit the action of each remedy to a very elementary level that must be progressively made more complex. Based on this approach, these authors used mice specific pharmacological models in relation to some Bach remedies to evaluate their action on the central nervous system. The results showed anti-inflammatory properties with significant differences to the placebo, which supports their use in inflammatory states. However, regardless of whether or not they contain a chemically active component, they can be used to generate meaning within an optimal healing environment.
Some authors [31, 40] propose that BFRs can be a good tool for 21st century nursing care and for improving the health problems of the general population. However, the literature is very limited and experimental studies with an appropriate methodology are necessary to obtain scientific evidence [40-42].
This research aimed to assess the effectiveness of BFRs in improving the quality of life and sleep of night shift workers in the hospital setting during COVID-19.
Materials and method
Mixed methodology
Observational, analytical and longitudinal study. Pilot, controlled and randomized clinical trial with case and control groups. The sample included 150 volunteers among the night-shift health professionals of the Hospital Sant Joan de Reus (the total number of workers in the night shift is 200), of which 60 met the inclusion criteria. We randomly chose 30 for the intervention group and 30 for the control. The study was conducted from March to May 2020 (Figure 1).+
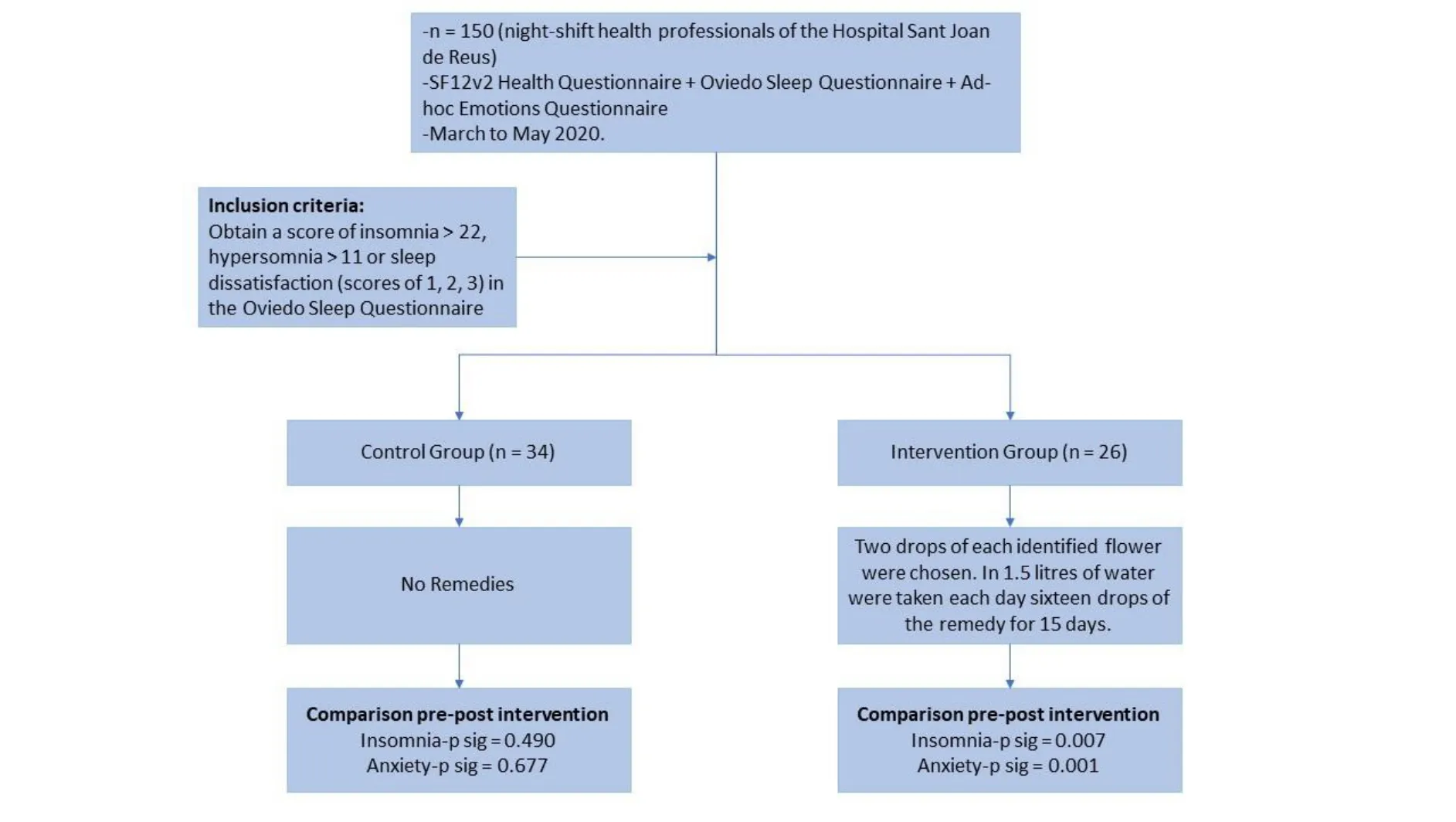
Figure 1 Mixed methodology
Inclusion criteria
Night shift staff (21:00 to 8:00) of the Hospital Sant Joan de Reus, with a minimum of 2 nights and a maximum of 5 nights worked per week. Obtain a score of insomnia > 22, hypersomnia > 11 or sleep dissatisfaction (scores of 1, 2, 3) in the Oviedo Sleep Questionnaire.
Exclusion criteria
Personnel who are on holiday, on sick leave, on leave or not working during the study period during the night shift. Failure to conclude the entire treatment established in the study and failure to meet some point of the inclusion criteria.
Instruments
SF-12v2Health Questionnaire. The SF-12v2is the short version of the SF-36v2, and is a significant improvement in measurement compared to the original SF-12. It was validated in the Catalan population by Schmidt et al [43] and recommended for research studies in this line of work. It measures quality of life from a personal perspective and can be self-administered. It consists of 12 items with 8 dimensions (physical role, body pain, general health, vitality, social function, emotional role and mental health) with which the physical (PHS) and mental (MHS) health scores are evaluated on a standardized scale based on population norms (mean = 50, DE (10)). Its reliability coefficients are close to 0.8.
Oviedo Sleep QuestionnaireThis is a hetero-administered questionnaire consisting of 15 items grouped into three subscales that assess insomnia, hypersomnia, and sleep satisfaction. It can be used to diagnose sleep disorders according to the criteria of the DSM-IV-TR and CIE 10.
Ad-hoc Emotions QuestionnaireA scale was created to measure the emotions most involved in COVID-19, based on participant observation and data published by the “Centro de Investigaciones Sociológicas” (CIS) [44] as well as the media [45] in the study time period. A numerical score from 0-10 is used to rate the subjective feeling of suffering due to these emotions. A score of 0 signifies an absence of emotion and 10 means maximum expression. The variables measured were: anxiety, fear, uncertainty, sadness and worry.
Interview
To get to know the personal experiences of the study sample, a semi-structured interview was held with participants based on the open question, "How does what you are experiencing make you feel?”
Selection criteria for flower essencesThe criteria for choosing the flower remedy were based on the qualitative analysis of the ad-hoc questionnaire, the analysis of the interview and the open-ended question. The remedy was prepared in the laboratory by health personnel accredited in Bach flower therapy.
InterventionTo prepare the formula, two drops of each identified flower were chosen. In 1.5 litres of water were taken each day sixteen drops of the remedy for 15 days. The study consisted of the pre- and post-assessment of all variables. All participants in the case group will take the same essences, chosen according to the analysis of the answers to the qualitative questions.
Data analysis
Questionnaire scores were collected to create a database with the IBM SPSS Statistics program version 22.0 for Windows XP. The SF-12v2Health Survey was validated with the OPTUM PROcoRE program, license number QM052338, according to the reference population standards.
The comparability analyses of the two groups were performed with the Chi square test for the qualitative variables, and with the Student's t test or the non-parametric U-Mann Whitney test for the quantitative variables. In the analysis of related samples (pre and post intervention) we used the Student's t test for related samples or the non-parametric Wilcoxon test. The Shapiro Wilk test was used because the sample is small.
The study was conducted with 95% confidence, and the results were considered significant at an alpha level < 0.05.
Qualitative analysis began with manual elaboration of the interview and open-ended question. The interviews were then read to determine the most significant categories, and in a second reading the subcategories. To choose the flowers to be used in the study.
Ethical considerations.
The purpose of the study was explained to the participants in writing and orally. Informed consent was requested and signed. The possibility of withdrawing from the study at any time was indicated. Anonymity and confidentiality were guaranteed. The study was approved by the centre’s management. This research has been carried out according to the ethical requirements on biomedical research of the 1964 Declaration of Helsinki.
Results
Initially 150 Oviedo Sleep questionnaires were completed (81 nurses, 1 matron, 59 nursing assistants, 1 doctor, 3 support staff and 4 cleaners). Of these, 48 people (32%) wanted to participate in the study and 30 (62.5%) of these met the inclusion criteria for the experimental group. A total of 60 subjects (40%) entered the group randomization phase, and 26 subjects (92.3%) completed the study taking the flower remedy (17 nurses, 4 nursing assistants, 1 health technician and 3 cleaning staff members). A total of 34 (56.6%) (17 nurses, 16 assistants and 1 health technician) agreed to be part of the study without taking the flower remedy, of which 18 (52.9%) (17 nurses and 1 nursing assistant) completed the study.
Quantitative analysis
The results show that the participant profile is of a professional woman, around 40 years old, with 15 years working experience and 8 years on the night shift on average.
Oviedo Sleep Questionnaire
A total 82.6% of the sample suffer from insomnia, of which 13.3% are severe cases. It was found that insomnia has an inverse relationship with satisfaction.
A total of 29.4% of the sample have hypersomnia, of which 4.7% have severe symptoms. Hypersomnia does not correlate with satisfaction. The night shift staff in this study sleep an average of 6.3 hours. In Table 3 we can see that at the time of the post-intervention the group that took flower remedies showed a significant decrease in the insomnia variable (P= 0.007; n = 26) compared to the control group (P= 0.490; n = 34).
SF-12v2
The initial results show that the average is above 50 (according to a standardized scale based on the general population) for the PHS and below 50 for the MHS, denoting a decrease in the mental health dimension of the sample and an increase in the physical health dimension. It is noteworthy that 38% of the sample is at risk of depression, as 49% of individuals have MHS below the general population, as we can see in Figure 2.
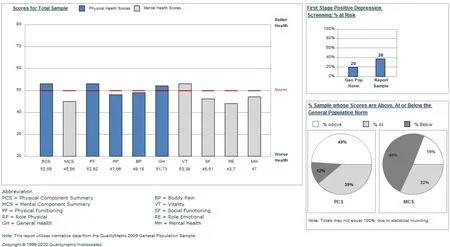
Figure 1 Quality of life assessed with the SF-12v2 compared to the general population. Source: Own elaboration.
Ad hoc questionnaire
Table 1 shows the results of the Ad-Hoc Emotions Questionnaire at baseline. It can be seen that all averages are above 3, and in particular, worry, uncertainty and anxiety. Sadness has the lowest score. Differences are observed with respect to the scores of the variables, showing that the intervention group has a higher score in all variables.
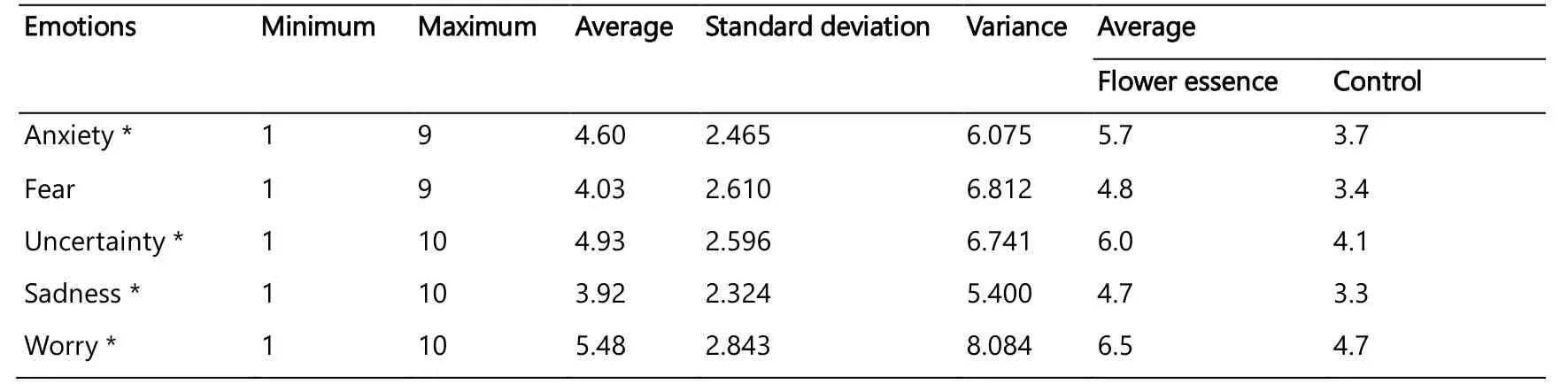
Table 1.Description of Ad-Hoc Emotions on a scale from 0 to 10. (Own elaboration)
Interview and open question
A total of 15 interviews were held with the open-ended question. From the analysis of these interviews emerged the special five-flower remedy category and three other categories: the group of fears, the group of hopelessness and despair and the group of little interest in the present. Five subcategories of flower remedies were established: Red Chestnut, Aspen, Crab Apple, Oak and Olive.
Table 2 summarizes the participants’ textual citations and the correlated flower groups, remedies, needs, and meanings. Finally, the flowers used for the study were: Rescue remedy (Impatiens+ Clematis+ Cherry Plum+ Star of Bethlehem+ Rock Rose), Red Chestnut, Aspen, Crab Apple, Oak and Olive.
Comparison pre-post intervention
Table 3 presents all the variables studied in the pre and post periods. The intervention group shows higher values than the control group at the beginning of the study; however, in the post-intervention, thegroup that took BFRs showed a decrease in almost all variables. Regarding the quality of life, the PHS remains virtually the same in both groups, but the MHS shows significant results (P= 0.007) in the intervention group, while the MHS of the control group decreased (P= 0.255). We also observe that in the intervention group there is a significant decrease in the insomnia variables (P= 0.007; n = 26) compared to the control group (P= 0.490; n = 34). It stands out that in the post intervention period most variables (P< 0.05) of the group that took flower remedies significantly decreased, unlike the control group (P> 0.05).
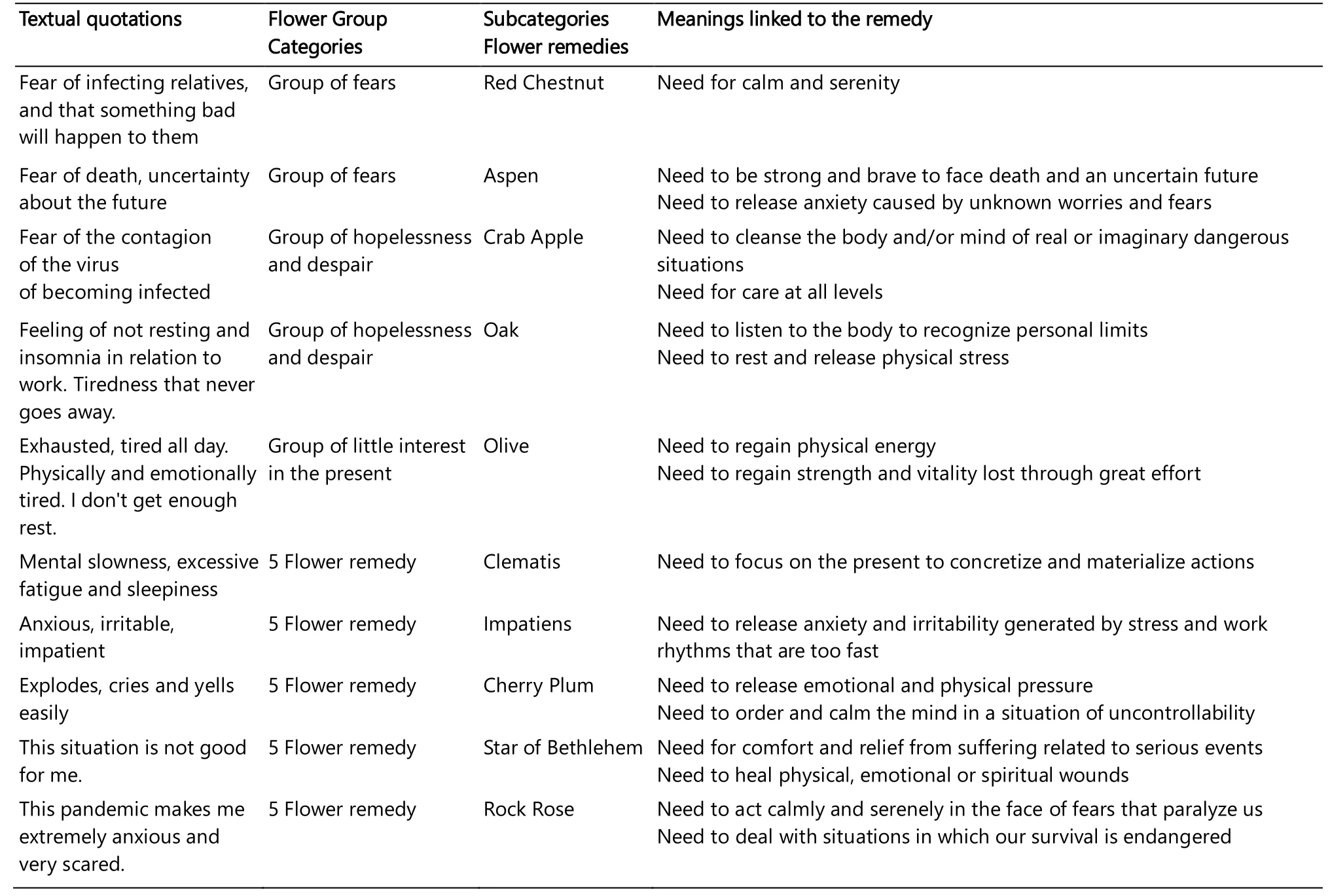
Table 2 Textual citations from the interviews in answer to the open-ended question, used in the analysis process for categorizing and subcategorizing into flower groups and flower remedies
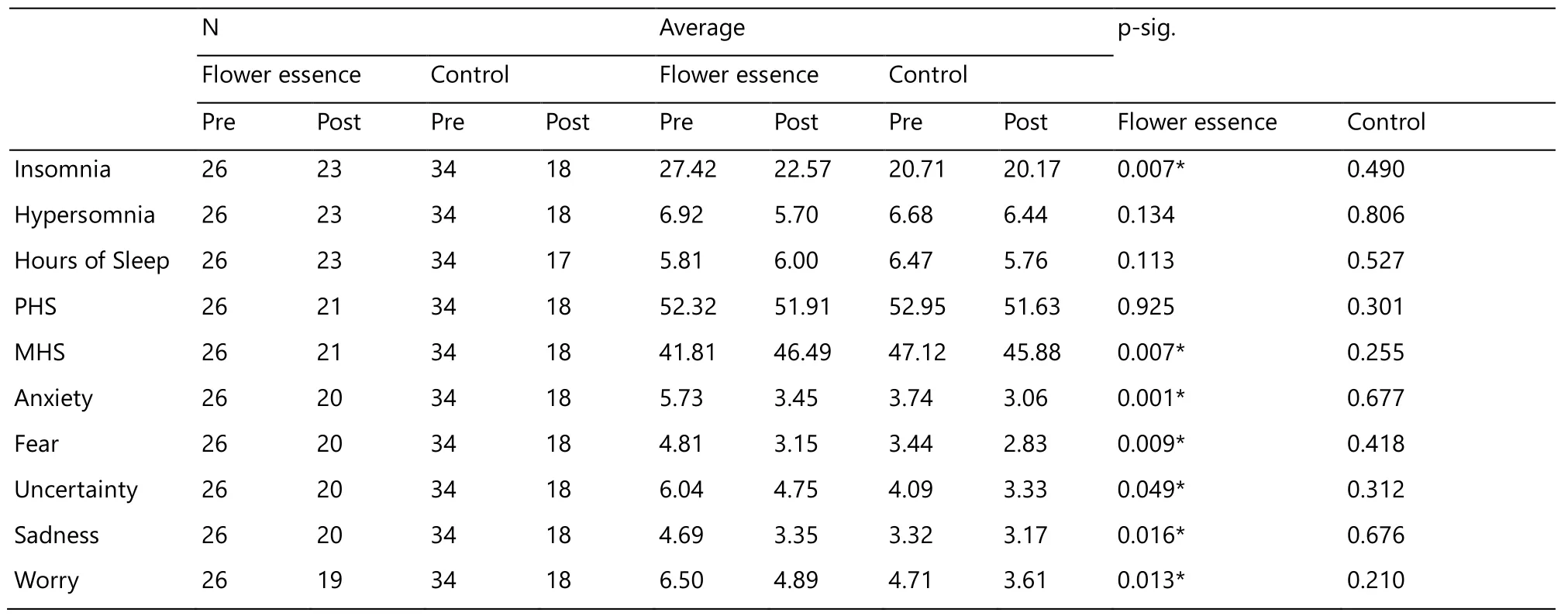
Table 3.Comparison pre-post intervention in the flower remedy group/control (own elaboration)
Discussion
Our work focuses primarily on nurses and professionals who provide care in the hospital setting. The sample studied was characterized by homogeneity, which favours the evaluation of the effectiveness of the intervention. No other remedies were taken during the intervention. The results show the participant profile of a professional woman with a mean age of 40 years, coinciding with Thimmapuran et al. [12] and Erquicia et al. [13], with 15 years working experience as a professional and 8 years on average on the night shift.
Regarding quality of life, the PHS showed better results than the MHS, which is in accordance with Rivera Rojas et al. [46], Peydró [47] and Burgos et al. [48]. In contrast, unlike these authors, in our study participants had a lower MHS at the beginning of the study. It is noteworthy that 38% of the sample is at risk of depression. This indicates that although the sample has adequate physical health, above the population average, it is necessary to improve mental health, which could be because the questionnaire was competed at the time of the national lockdown. However, in the case group the MHS was 7 points above the control group. This may be because the individuals most affected by insomnia and with a lower MHS may have been more interested in participating in a study of this kind.
At the end of the intervention, both groups presented better MHSs, but significant results were only obtained in the group that took BFRs. This indicates that participants adapted to the adverse environment of the pandemic. We can say, in accordance with Hylton Rushton et al. [49], that a certain resilience was developed which protected staff from emotional exhaustion.
As described by other authors [8-10] a significant percentage of participants also reported symptoms of anxiety, uncertainty and worry, mainly related to the feeling that there was a lack of protective measures and having to deal with traumatic events related to patient death or decision-making in a context of limited options, as well as fear of the contagion itself and of transmitting the infection to relatives [11]. These symptoms, along with fear and sadness, were the emotions that the participants experienced most intensely. We agree with Rivera Rojas et al. [46] that the perception of psychosocial risks can influence health-related quality of life. It should be noted that, at the beginning, the intervention group had higher values of all variables, this may be because the people most affected by the situation were more interested in participating in the study. At the time of the post-intervention, the results show that both groups had improved; however, only those who took BFRs achieved significant results and the level of worry, uncertainty, anxiety, sadness and fear decreased, as in other studies [32, 50].
In accordance with Thimmapuran J. et al. [12] and Huang [13] our study results show that participants have difficulty sleeping and a high prevalence of insomnia, and, in accordance with these authors, we believe that the pandemic may have worsened sleep patterns. In this study, although the group that took flower therapy slept fewer hours, their insomnia significantly improved. It is noteworthy that although White Chestnut is one of the most indicated remedies for insomnia and authors such as Torres Machado et al. [51] have used it for this health problem and Rodriguez-Martín [52] have used it for unwanted intrusive thoughts, it was not identified in the qualitative analysis. This may be because the symptom is not the indicator of the remedy, but the personal experience of the problem and the emotion that accompanies it [53].
Hernandez Garcia [24] speaks of fatigue or stress out of compassion, which may appear as a response to a person's suffering. Factors such as exposure to traumatic and stressful situations and the lack of resources [28] are situations that involve alteration of the physical, emotional, spiritual and social areas. In this study, BFRs were applied at the time of the problem as a coping strategy focused on decreasing the negative effects of the pandemic.
In accordance with Du Toit [11], the fear of the risk of infection, and especially the fear of infecting relatives, was one of the other signs that emerged in our study, as shown by other authors who have researched the psychological impact on health workers in other pandemics, such as SARS [54, 55]. In our study, Red Chestnut was the flower remedy to address the fear of infecting loved ones. This remedy gives us calm, serenity and positive thinking in relation to the suffering, anxiety and distress generated by worrying about loved ones and helps us to identify the unconscious projections of our fears reflected in others [53].
Aspen helps us deal with the anxiety generated by the fear of death and everything that is unknown to us, that is inexplicable or for which we cannot find a logical reason, unknown situations that distress us and the different related behaviours. Crap Apple is for addressing the fear of the contagion itself, as well as the fear of viruses and bacteria and thoughts related to these fears, this remedy acts when we are afraid of becoming contaminated and sick.
Olive is indicated in situations where we feel exhausted and need to continue, with this remedy we faced the secondary exhaustion coming from making a great effort due to a situation that required a great deal of personal involvement. Oak is the remedy linked to the work and professional environment, when we have an excess of responsibility and a sense of duty, we do not allow ourselves to stop or to rest, becoming run down on all levels. Both remedies belong to the group of the seven helpers. This group indicates chronicity, suggesting that, despite being a current experience, the symptoms may have a past origin. The fatigue may have accumulated over time and the pandemic worsened this situation. Analysing the results, we believe that Olive and Oak are two essential remedies when physical and mental exhaustion is related to a pandemic.
The five-flower remedy is a combined formula of flower remedies, which is indicated to relieve the acute stress of emergencies, shock and anxiety. The aim of this remedy is to obtain a quick response to overcome difficult and/or extreme situations. In accordance with Yang & Wang [34] and Halberstein et al. [32], in this study we believe this formula helped to improve fear and anxiety, as opposed to Ernst [35], who found no specific effects on anxiety.
In accordance with Erquicia et al. [8] and Hernández Garcia [24] we believe that it is necessary to raise health personnel’s awareness about the psychological problems that can be experienced in extreme situations and to encourage self-care and intervention strategies. In our study, participants had the opportunity to become more aware of the situation experienced and their emotions through the meanings linked to the flower remedies they took. They also had the opportunity to identify their needs and those attitudes that need to change.
Authors as Solano and Fusco [26, 27] also identify that Bach's floral therapy improves sleep quality, anxiety and is an effective tool in times of emergency such as the pandemic.
In general, it can be staid that the intervention had a favourable effect on quality of life and sleep. The findings of this study provide us with relevant data on the contributions of BFRs in the hospital setting in times of a pandemic. They also show us the possibility of continuing to study the effects of this modality.
Limitations
This study has several limitations that affect the possibility of generalizing the results. First, the sample size was small. Second, most participants were women, although there is no evidence that the effectiveness of BFRs varies according to gender. Another limitation is the ad-hoc questionnaire, as it only considered five variables. Using the Pittsburgh sleep quality questionnaire would have provided more accurate results in sleep quality.
The heterogeneity of the two groups is also a limitation when the data are extrapolated and generalized.
Conclusion
BFRs could be an effective intervention in managing emotions and insomnia in hospital night shift staff.
BFRs could be an effective coping strategy in pandemic or emergency situations. In addition, they could be a health education tool to raise awareness of personal needs and encourage self-care. No adverse effects were observed in the study.
More studies are needed with a good methodological design and that include larger study groups over a longer period of time to gain more evidence of the effectiveness of flower remedies.
- Nursing Communications的其它文章
- The effects of the application of WeChat as a platform combined with problem-based learning in nursing teaching in China: a systematic review and meta-analysis
- Observation on the clinical effect of abdominal massage combined with fomentation in the treatment of constipation-predominant irritable bowel syndrome
- Practice of the construction and management of TCM nursing outpatient service — takes a breast specialty in a third-grade hospital in Beijing as an example
- Analysis of ideological education status of male undergraduate nursing students