Combined ab-interno trabeculectomy and cataract surgery induces comparable intraocular pressure reduction in supine and sitting positions
Caroline Gietzelt, David Kiessling, Randolf A. Widder, Ludwig M. Heindl, Claus Cursiefen,Thomas S. Dietlein, Philip Enders
1Department of Ophthalmology, University of Cologne,Faculty of Medicine and University Hospital Cologne,Kerpener Stra?e 62, Cologne 50924, Germany
2Glaucoma Imaging Center University of Cologne (GICC),Faculty of Medicine and University Hospital Cologne,Kerpener Stra?e 62, Cologne 50924, Germany
3Department of Ophthalmology, St Martinus-Krankenhaus Duesseldorf, Gladbacher Stra?e 26, Düsseldorf 40219,Germany
Abstract
INTRODUCTION
Glaucoma is one of the three most frequent causes for blindness both in Europe and worldwide[1]. The intraocular pressure (IOP) is one of the most important risk factors for glaucoma and glaucoma progression and yet the only parameter accessible for ophthalmologic treatment[1]. A change in body posture is known to induce a change in IOP with higher IOP levels in supine than in sitting positions[2-3].Elevation of episcleral venous pressure, choroidal vascular congestion and reduced capacity of trabecular outflow are possible reasons for this posture‐induced IOP increase[4].Numerous studies have shown posture-induced IOP elevation to be higher in glaucoma patients with a 3.5-8.0 mm Hg increase from sitting to supine position than in healthy subjects with an increase of 2.0-3.0 mm Hg[2,4-6]. Posture-induced IOP elevation seems to have increased relevance in normal tension glaucoma (NTG) compared to open angle glaucoma[6-7]. While evidence on the clinical importance of elevated supine IOP(suIOP) levels in glaucoma is still only limited[8], some studies suggest that elevated suIOP and higher fluctuations in IOP are risk factors for an accelerated progression of glaucoma[9-11].
Based on the currently available evidence, aim of glaucoma treatment should not only address reaching the target IOP during daytime but also to reduce nocturnal IOP levels in supine posture. Topical anti-glaucomatous therapy[12-13], laser trabeculoplasty[14], cataract surgery[15], and canaloplasty[16]seem to have only a limited reducing effect on IOP levels in a supine position. Trabeculectomy however has been shown to significantly lower posture‐induced IOP peaks in a supine position and to flatten IOP fluctuations in a 24‐hour IOP profile[12,16]. Any successful trabeculectomy creates a long term drainage pathway into a newly created subtennonal compartment and bypasses the conventional aqueous humor drainage pathway[4,16].
Even though outflow of aqueous humour can be visualized and studied by aqueous angiography[17], the contribution of each step of this pathway to the mechanism of this posture-induced IOP increase remains not fully understood.
Ab-interno trabeculectomy by electroablation of the trabecular meshwork is a comparably new surgical procedure to treat glaucoma, which can be conducted both as stand-alone procedure or combined with cataract surgery. Significant IOP lowering effects of ab‐interno trabeculectomy have been demonstrated by Meta-analyses for both stand-alone and combined approaches[18-19]. Chowet al[18]showed a 25%-34%reduction in IOP and reduction in topical antiglaucomatous medications (TAM) of between 0.17 and 1.1 medications after stand-alone ab-interno trabeculectomy and Kaplowitzet al[19]found a mean IOP reduction of 27% and reduction in TAM of 0.76 medications twelve months after combined ab-interno trabeculectomy and cataract surgery. A study by Tojoet al[20]found a significant reduction in IOP fluctuations three months after ab-interno trabeculectomy measured by a Triggerfish?contact lens sensor. The duration of the IOP decreasing effect of ab-interno trabeculectomy is thought to be at least up to 2y with a success rate after 2y of 85% for combined cataract surgery and ab-interno trabeculectomy and 46%-51% for standalone surgery (success rate was defined as a postoperative IOP?21 mm Hg and a ≥20% reduction from baseline in both studies)[19,21].
Newer surgical therapies for glaucoma as the ab-interno tabeculectomy still lack data on the IOP lowering effect for different body postures and different time points during a 24-hour IOP profile. Main objective of this retrospective analysis was to evaluate the therapeutic effect of ab-interno trabeculectomy for glaucoma on IOP levels in supine and sitting postures. Further goal was to compare the change in patients’ suIOP increase before and after treatment with abinterno trabeculectomy in cases where preoperative supine data was available.
SUBJECTS AND METHODS
Ethical ApprovalAccording to regional medical regulations on retrospective single-centre clinical studies (§15 of the Professional code of conduct, General Medical Council for the Northern Rhine in accordance with the General Data Protection Regulation GDPR of the European Union), the Ethics Committee of the University of Cologne ruled that approval was not required for this retrospective analysis.Throughout the whole study, the 1964 Helsinki Declaration and its later amendments as well as all applicable national regulations and laws were observed.
All 297 patients treated by ab-interno trabeculectomy at the Department of Ophthalmology, University Hospital of Cologne, Germany between January 2016 and December 2017 were retrospectively reviewed. Cases fulfilling the following inclusion criteria were included: 1) history of ab-interno trabeculectomy by electroablation of the trabecular meshwork either as stand-alone procedure or combined with cataract surgery in one eye; 2) availability of a postoperative 24-hour IOP profile with a minimum of three IOP measurements in a sitting position during the day and one in supine position in the early morning one month to two years after surgery; 3)patients diagnosed with primary open angle glaucoma (POAG)or pseudoexfoliation glaucoma based on the criteria defined by the European Glaucoma Society (EGS) including typical visual field defects in 30:2 perimetry and alterations to the neuroretinal tissue of the optic nerve head in optical coherence tomography (OCT) and funduscopy. Exclusion criteria were:1) any history of trabeculectomy, canaloplasty or glaucoma drainage device surgery in either eye; cases with selective laser trabeculoplasty (SLT) within six months before surgery were excluded as well 2) history of ab-interno trabeculectomy in the fellow eye; 3) intake of systemic carboanhydrase inhibitors at the time of the postoperative 24‐hour IOP profile;4) secondary glaucoma diagnosis (for example due to uveitis or rubeosis iridis). Twenty‐six patients fulfilling all inclusion and no exclusion criteria could be included. The main reasons for exclusion of patients were a lack of full 24h IOP profile available or prior history of glaucoma surgery in the study eye or history of ab-interno trabeculectomy in the fellow eye.
Clinical data on patients’ medical history including ophthalmologic diagnoses, best corrected visual acuity (BCVA),topical medication, epidemiologic data and results of visual field testing were collected from patients’ files.
In clinical routine at our center, visual field testing was conducted separately for each eye using an Octopus 101 visual field analyzer (Haag-Streit AG, Koeniz, Switzerland) with a 30/2 white-on-white standard pattern using a tendency-oriented perimetry (TOP) strategy, according to standard operating procedures of the center[22-24]. Data were analyzed with Peridata 3.1 (PeriData Software GmbH, Huerth, Germany).
Ab-interno trabeculectomy was performed using the trabectome surgical system (Microsurgical Technology,Redmond, WA, USA). The surgical technique followed standard operating procedures of the center as previously described[25-26].
Hospitalization of Patients to Obtain 24-hour IOP Profiles in GermanyThe 24-hour IOP profiles were obtained in patients following standard operating procedures based on recommendations of the German Ophthalmological Society[27].Data of 24-hour IOP profiles before and after surgery were extracted from the patients’ medical files. IOP was assessed by corneal rebound tonometry (Icare tonometer TA01i, Icare Finland Oy, Vantaa, Finland) at 8a.m., 3p.m., 8p.m.and 11p.m.(±1h respectively) in a sitting position and at 6a.m.(±1h)in supine position (suIOP) after at least 3h of uninterrupted bedrest. Patients with known nycturia were instructed to prepare for that period of 3h. In case of a hospitalization for more than 24-hours, mean IOP values were calculated for all timepoints that are stated above independently. Furthermore,for all patients a mean sitting IOP (siIOP) value was calculated from measurements at 8a.m., 3p.m., 8p.m.and 11p.m.Peak siIOP was evaluated as the maximum IOP registered between 8a.m.and 11p.m.
Statistical AnalysisStatistical analyses were conducted using the software SPSS (Version 25.0; IBM Corp, Armonk, New York, USA). Presence of normal distribution was confirmed with the Shapiro-Wilk test. Student’st-test for paired samples was used to compare means for parameters with normal distribution. For parameters without normal distribution,Mann-WhitneyUor Wilcoxon tests were used to test for differences. The threshold for statistical significance was set toP<0.05. Figures displayed in the manuscript were created with SPSS accordingly. Boxplot graphs indicate the median, the 25% and 75% inter-quartile ranges (IQR). Whiskers span to the 1.5× of the IQR. Outliers are indicated by small circles.
RESULTS
Twenty-six patients could be identified, who fulfilled all inclusion and no exclusion criteria. In twenty-four (92.3%)patients ab-interno trabeculectomy was combined with cataract surgery, two (7.7%) patients received ab-interno trabeculectomy as stand-alone procedure. Mean time span between the ab-interno trabeculectomy and postoperative 24-hour IOP profile was 9.6±6.8mo (range, 2.0 to 24.3mo after the ab-interno trabeculectomy). Patients enrolled in this study were selected according to the inclusion criteria to present homogeneous glaucoma diagnoses. POAG was present in 24 eyes (92.3%) and pseudoexfoliation glaucoma in 2 eyes(7.7%). One study eye (3.8%) and 2 fellow eyes (7.7%)had already received uncomplicated cataract surgery before undergoing ab-interno trabeculectomy. Preoperative BCVAwas significantly worse in study eyes (0.24±0.19 logMAR)compared to the fellow eyes (0.13±0.14 logMAR,P<0.001;Table 1). Mean deviation (MD) of visual field function was marginally not significantly different between the study eyes and the fellow eyes [MD (study eyes) =-8.7±7.0, MD (fellow eyes)= -5.3±5.2,P=0.057].

Table 1 Epidemiologic data
Preoperatively, siIOP was 17.6±5.3 mm Hg in study and 17.1±4.7 mm Hg in fellow eyes (P=0.347). Study eyes were treated topically on average with 2.8±1.0 TAM prior to surgery.
After surgery, study eyes had a mean siIOP of 14.5±3.6 mm Hg.This IOP change of -3.2 mm Hg (18%) was statistically significant (P=0.009,n=23). TAM could be reduced from 2.8±1.0 medications to 1.3±1.34 in these eyes (P<0.001).
Fellow eyes, which were not treated by ab-interno trabeculectomy,had a significantly higher mean siIOP of 16.2±3.4 mm Hg(P=0.048).
Similarly, postoperative mean suIOP in study eyes was 18.0±3.5 mm Hg and thereby significantly lower than in fellow eyes with 20.5±5.1 mm Hg (P=0.013). In both study and fellow eyes, suIOP was significantly higher than siIOP(P<0.001 respectively). In study eyes, IOP increased on average by 3.5±4.1 mm Hg between sitting and supine positions. In fellow eyes, this IOP change was more pronounced with 4.4±4.8 mm Hg. This difference of posture induced IOP increases was not statistically significant (P=0.45). The difference between peak siIOP and suIOP was lower in study eyes (0.9±4.3 mm Hg) compared to fellow eyes (1.7±5.4 mm Hg,P=0.58). Regarding relative IOP changes between sitting and supine postures, study and fellow eyes showed comparable patterns. In study eyes, IOP went up by 30.0%±34.5% while fellow eyes saw an IOP increase of 30.0%±31.1% (P=0.99).Figures 1 and 2 display postoperative 24‐hour IOP profiles of study and fellow eyes.
A subgroup analysis of 16 patients who received the 24-hour IOP profile less than twelve months after surgery demonstrated comparable results.
We conducted a subgroup analysis including only patients with POAG and excluding the two patients with pseudoexfoliation glaucoma. In this subgroup, results were comparable: after surgery, the mean siIOP of study eyes decreased significantly by 3.4 mm Hg (19%) to 14.4±3.6 mm Hg (P=0.01,n=21).
Fellow eyes in this subgroup, which were not treated by ab-interno trabeculectomy, had a higher mean siIOP of 15.9±3.3 mm Hg, this difference however was not statistically significant due to reduced sample size (P=0.108).
Postoperative mean suIOP in study eyes was 17.9±3.7 mm Hg and thereby significantly lower than in fellow eyes with 20.3±5.2 mm Hg (P=0.029). In both study and fellow eyes, suIOP was significantly higher than siIOP (P<0.001 respectively). In study eyes, IOP increased on average by 3.4±4.3 mm Hg between sitting and supine positions. In fellow eyes, this IOP change was more pronounced with 4.4±5.1 mm Hg.Regarding relative IOP changes between sitting and supine postures, study and fellow eyes showed comparable patterns.In study eyes, IOP went up by 30.5%±35.9% while fellow eyes saw an IOP increase of 30.9%±32.3%.
We conducted a second subgroup analysis on 22 patients excluding those with history of SLT (n=4). Also, in this subgroup, we found comparable results: Before surgery,the mean siIOP of study eyes was 17.8±5.7 mm Hg. After surgery, the mean siIOP of study eyes decreased significantly by 3.1 mm Hg (17%) to 14.7±3.6 mm Hg (P=0.03). After surgery, fellow eyes had a higher mean siIOP than study eyes(mean difference 1.6±4.2 mm HgP=0.10). Also, suIOP was significantly higher in fellow eyes than study eyes after surgery(mean suIOP study eyes=18.1±3.5 mm Hg, mean suIOP fellow eyes=21.1±5.0 mm Hg,P=0.01). In both study and fellow eyes, suIOP was significantly higher than siIOP (P≤0.001 respectively). The relative increase from sitting to suIOP was comparable between study eyes [increase of 28.5%±32.9%(3.3±4.0 mm Hg)] and fellow eyes [increase of 31.8%±31.1%(4.7±4.8 mm Hg)].
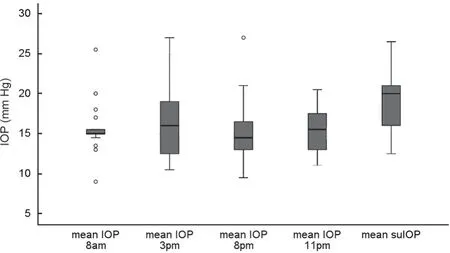
Figure 1 The 24-hour IOP profile of study eyes after surgery (n=26)Boxplot graphs indicate the median, the 25% and 75% IQR. Whiskers span to the 1.5× of the IQR. Outliers are indicated by small circles.

Figure 2 The 24-hour IOP profile of fellow eyes after surgery (n=26)Boxplot graphs indicate the median, the 25% and 75% IQR. Whiskers span to the 1.5× of the IQR. Outliers are indicated by small circles.
Preoperative suIOP measurement was available only in eleven study eyes of all included patients. The reason for this was to avoid waking patients up early in the morning on the day of the surgery without clinical relevance of the suIOP measurement.In this subgroup, mean baseline suIOP was 22.4±6.1 mm Hg.After surgery, mean suIOP was reduced to 19.5±3.8 mm Hg.The change in suIOP of -2.9 mm Hg (13%) was not statistically significant due to small sample size (P=0.203,n=11).
The mean posture-induced change of IOP between sitting and supine positions was comparable before and after surgery in this subgroup. Preoperatively, IOP rose by 30.7%±33.0%during bed rest while postoperative IOP change was 37.1%±36.5% (P=0.66). Figures 3 and 4 show dynamics of siIOP and suIOP before and after surgery in this subgroup and 24‐hour IOP profile of study eyes before surgery.
DISCUSSION
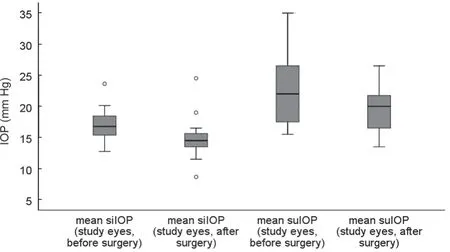
Figure 3 Dynamics of siIOP and suIOP before and after surgery in study eyes (n=11) Boxplot graphs indicate the median, the 25%and 75% IQR. Whiskers span to the 1.5× of the IQR. Outliers are indicated by small circles.
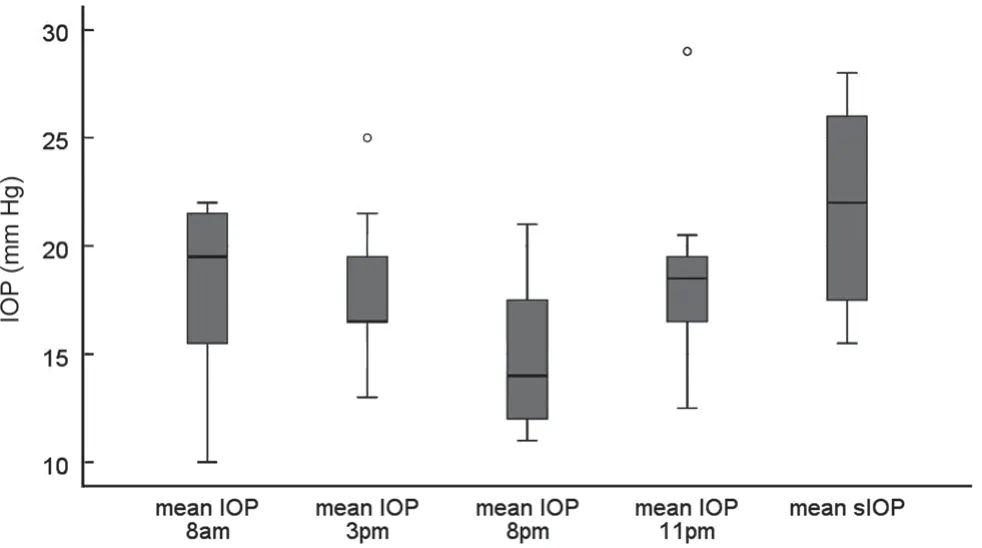
Figure 4 The 24-hour IOP profile of study eyes before surgery (n=11)Boxplot graphs indicate the median, the 25% and 75% IQR. Whiskers span to the 1.5× of the IQR. Outliers are indicated by small circles.
Overall, this study found ab-interno trabeculectomy standalone or combined with cataract surgery to lower mean siIOP by 18% to an average of 14.4 mm Hg ten months after surgery. Topical medication could be reduced equally by 1.5 medications (54%). These results are in line with current literature, showing significant IOP lowering effects of abinterno trabeculectomy both stand-alone and in combination with cataract surgery for up to two years after surgery[18-21].In comparison to other studies we found a comparable postoperative mean siIOP. For example Kaplowitzet al[19]found a mean postoperative IOP of 15 mm Hg twelve months after combined ab-interno trabeculectomy and cataract surgery and Mizoguchiet al[21]showed a mean postoperative IOP of 14 mm Hg at the 2y follow-up after stand-alone ab-interno trabeculectomy. Our findings also support a hypothesis of Polat and Loewen[28], who suggested the outcome IOP after abinterno trabeculectomy to be capped at 15 mm Hg close to the episcleral venous pressure.
Yet, the mean relative reduction was weaker in our study than in previous studies by Mizoguchiet al[21]and Kaplowitzet al[19], who found a reduction of 23% and 27% respectively.This difference can be explained by a lower baseline IOP in our study (the baseline IOP in our study was 17.6 mm Hg compared to 22.3 mm Hg and 26.7 mm Hg), different follow‐up periods and the different measurement times of IOP. In contrast to our study, in which the mean siIOP was calculated as a mean of the IOP values at 8a.m., 3p.m., 8p.m., and 11p.m.,in most studies included in the reviews by Chowet al[18]and Kaplowitzet al[19]only one day time measurement was taken both preoperatively and postoperatively. Also, in these Metaanalyses, topical medication was only reduced by 0.17-1.1 medications in contrast to a reduction by 1.5 medications in our study explaining a smaller relative reduction in IOP[18-19].The primary objective of our retrospective analysis was to study the effect of ab‐interno trabeculectomy on suIOP levels in glaucoma patients. Our study results indicate that this surgical approach allows significant reduction of IOP in supine posture by an average of 2.9 mm Hg. Relative reduction of suIOP levels by ab-interno trabeculectomy was between 12%to 13%.
Additionally, posture-induced IOP increase in supine position changed after surgery to the same extend as the mean IOP in a sitting position. Mean IOP change between sitting and supine body positions was 32% preoperatively and 37% after surgery without statistically significant difference.
Our results on suIOP levels are in line a study of Tojoet al[20],who showed a reduction in IOP fluctuations both during the night and during the day after ab-interno trabeculectomy combined with cataract surgery compared to preoperatively.However, this study only measured IOP fluctuations and not IOP values during night time and in supine position.
In our review of existing literature, we have not found any data on the effect of ab‐interno‐trabeculectomy on suIOP levels. In contrast to this, a significant reduction of the relative increase from sitting to suIOP has been described for conventional trabeculectomy[16]. This divergent effect on IOP patterns could be explained by the anatomic and physiological differences of both surgical approaches. In trab, where significant lowering of suIOP levels can be found, the aqueous humor bypasses all layers of the anatomical drainage pathway. In ab-interno trabeculectomy resulting in reduction of resistance of the trabecular meshwork only, the aqueous humour still drainsviaSchlemm’s canal and the uveoscleral and episcleral veins.Therefore, the IOP is still influenced by the change of venous pressure depending on position of body and head. In our study ab-interno trabeculectomy was combined with cataract surgery in 92% of included cases. Therefore, the effect of ab‐interno trabeculectomy cannot be distinguished from the effect of the cataract surgery itself. Standard cataract surgery is known to incorporate a temporary IOP lowering effect for conventional IOP measurement during daytime[29-30]. In a Meta-analysis the mean IOP reduction for POAG was found to be -2.7 mm Hg for stand-alone cataract surgery[30]. However, available data about the effect of stand‐alone cataract surgery on the suIOP levels is very inhomogeneous[15,31-33]. While some studies found a lowering effect on IOP fluctuations during the night in primary angle-closure glaucoma (PACG)[34]and diurnal fluctuations in pseudoexfoliation glaucoma[33], others found no effect on suIOP by cataract surgery in PΑCG[15]or no effect on IOP fluctuations[32]or the magnitude in posture-induced IOP change of non-glaucoma patients[31]. Based on these findings,the effect of ab-interno trabeculectomy may outweigh the effect of cataract surgery.
Limitations of our study include the retrospective setup of the study, the relatively small sample size, heterogeneous study group and a potential selection bias due to exclusion of incomplete datasets. Four of the 26 patients underwent SLT more than six months prior to the study procedure. As SLT alters the trabecular meshwork, this could have influenced the results. Due to the low number of patients with prior SLT this effect is thought to be of minor importance.
The retrospective nature of the study and limited data availability lead to inclusion of more than one type of glaucoma (i.e.,pseudoexfoliation glaucoma and POAG). This heterogeneity of the study group could reflect a more realistic clinical setting.Most patients included in our study, received the 24-hour IOP profile during the day or the two days before ab‐interno trabeculectomy or cataract surgery of the fellow eye and therefore should not represent a bias towards complicated cases. Our study design required the first eyes receiving abinterno trabeculectomy to be selected as study eyes to allow comparison to the untreated fellow eye. Following standard of clinical care, the eye that is stronger affected by glaucoma is operated first. In our study preoperative MD as well as preoperative siIOP and suIOP were comparable between study and fellow eyes, but there was a significantly worse BCVΑ in study eyes than in fellow eyes, indicating that BCVA might have driven the decision which eye to operate first.
Another potential bias is the different number of topical antiglaucomatous and other medications before and after surgery and between the study and the fellow eyes after surgery. As pre- and postoperative TAM mainly topical betaadrenergic receptor antagonists, alpha2-adrenergic agonists,prostaglandin analogs as well as carbonic anhydrase inhibitors were used in both study and fellow eyes. However, as different studies have shown[12-13], topical anti-glaucomatous therapy has only very limited effect on suIOP. Therefore, this difference in TΑM is thought to have only a minor effect on our study results.In summary, we found a significant IOP lowering effect of ab‐interno trabeculectomy not only during daytime in a sitting position but also in a supine position after three hours of uninterrupted bedrest. The extent of IOP reduction between both body postures–sitting and supine–is however comparable.The relative increase from sitting to suIOP could not be altered by this approach of glaucoma surgery.
ACKNOWLEDGEMENTS
We thank all technical experts of our imaging laboratory and FOR 2240 “(Lymph-) Angiogenesis and Cellular Immunity in Inflammatory Diseases of the Eye” for their support (www.for2240.de).
Conflicts of Interest: Gietzelt C,None;Kiessling D,None;Widder RA,None;Heindl LM,None;Cursiefen C,None;Dietlein TS,None;Enders P,None.
 International Journal of Ophthalmology2021年8期
International Journal of Ophthalmology2021年8期
- International Journal of Ophthalmology的其它文章
- Macular density alterations in myopic choroidal neovascularization and the effect of anti-VEGF on it
- Mid-term results of patterned laser trabeculoplasty for uncontrolled ocular hypertension and primary open angle glaucoma
- Comparison of the SlTA Faster–a new visual field strategy with SlTA Fast strategy
- Evaluating newer generation intraocular lens calculation formulas in manual versus femtosecond laser-assisted cataract surgery
- Conjunctival flap with auricular cartilage grafting: a modified Hughes procedure for large full thickness upper and lower eyelid defect reconstruction
- Improvement of human embryonic stem cell-derived retinal pigment epithelium cell adhesion, maturation, and function through coating with truncated recombinant human vitronectin
