Stem cell injection for complex anal fistula in Crohn’s disease: A single-center experience
Oliver Schwandner
Abstract
Key Words: Complex anal fistula; Crohn’s disease; Stem cell therapy; Mesenchymal stem cells; Darvadstrocel; Treatment; Surgery; Outcomes
INTRODUCTION
Both medical and surgical options for complex perianal fistulas associated with Crohn’s disease remain difficult and challenging[1 -5 ]. Despite recent progress in medical treatment including biologicals and actual trends in sphincter-preserving surgical techniques, considerable recurrence rates after definite surgery for Crohn’s anal fistula have been documented[2 ,3 ,5 ]. As an interdisciplinary treatment regimen is the prerequisite for disease control and potential long-term remission of perianal fistulizing Crohn’s disease, therapeutic goals include symptom improvement (e.g.,reduction of secretion, absence of pain), prevention of recurrent perianal abscess requiring further surgery, preservation of continence, improvement of quality of life and, finally, healing of the fistula.
Focusing on surgical procedures for complex anal fistulas, conventional procedures such as advancement flap repair have shown considerable failure rates for Crohn’s fistulas, whereas innovative surgical options such as ligation of the intersphincteric fistula tract (LIFT), biomaterials (e.g., plug) or video-assisted anal fistula treatment seem to have a 50 % healing rate after 12 mo without significant impairment of continence[6 ]. Recently, several reports and randomized studies have demonstrated that stem cell therapy for Crohn’s complex anal fistula has raised the healing rates after 12 mo[2 ,7 ,8 ].
Impressed by the encouraging healing rates reported from the ADMIRE trial[7 ,8 ], it was the aim of this retrospective single-center study to evaluate the current results of stem cell therapy for complex anal fistulas in Crohn’s disease with special focus on indication, patient selection and long-term outcome.
MATERIALS AND METHODS
Clinical setting
Stem cell injection was performed by administration of human, allogenic, expanded adipose-derived mesenchymal stem cells (darvadstrocel) for complex anal fistulas associated with Crohn’s disease in adult patients. For the current study, Alofisel?(5 million cells/mL) was used (Takeda GmbH, Konstanz, Germany). Upon authorization of the European Medicines Agency (initial authorization on December 14 , 2017 ),Alofisel?is indicated in patients with non-active or mildly active Crohn’s disease when fistulas show an inadequate response (failure either due to persistence or recurrence)to at least one conventional, biological or surgical therapy. Darvadstrocel was only administered if the fistulas had conditioning by curettage or seton drainage. All potential candidates for stem cell injection had fully informed consent of the innovative method and underwent a selection process by multidisciplinary evaluation and discussion (gastroenterology and proctology); finally, the center was trained by an educational and hands-on workshop for the use of darvadstrocel in complex fistulas in Crohn’s disease to ensure that only specialist physicians perform the procedure.Moreover, intrainstitutional education was conducted for darvadstrocel administration (e.g., pharmacy, surgical team).
Study population
All patients with complex anorectal fistulas associated with Crohn’s disease who were amenable for definite fistula closure were potential candidates for darvadstrocel administration if at least one conventional or surgical attempt to close the fistula had failed. All patients suffered from complex fistula according to American Gastroenterological Association and Parks classification[9 ,10 ]. All patients had a minimum of one complex fistula, including patients with two complex fistulas in 58 .3 % (7 /12 ).According to Parks classification, 76 % of the fistulas were transsphincteric and 14 %were suprasphincteric. Darvadstrocel was only indicated in patients without active Crohn’s disease, ruled out by ileocolonoscopy, and without the presence of anorectal abscess assessed by clinical examination and/or pelvic magnetic resonance imaging(MRI). Additionally, all patients had interdisciplinary discussion prior to surgical treatment. Specific inclusion and exclusion criteria are outlined in Table 1 .
Study design and outcome evaluation
To evaluate the outcome of patients who underwent local stem cell injection by the application of darvadstrocel, a retrospective analysis of existing routine clinical data was performed. In detail, regular clinical data of patient care and quality control(including patients’ characteristics, type of therapy, outcome evaluation during routine clinical follow-up) were retrospectively analyzed in an anonymized fashion. Patients underwent darvadstrocel administration not for primary study purpose but for quality assurance and patient care. To assess outcome, criteria of healing included that both internal and external openings were closed, no abscess or fluid collection was present and if the patient was free of symptoms (e.g., pain, secretion). Healing was assessed by clinical examination and proctoscopy. Strict criteria and definitions of persistence and recurrence are outlined in Table 2 .
Special consideration for coronavirus disease 2 019 pandemic
Due to the coronavirus disease pandemic in the beginning of 2020 , the coronavirus disease 2019 (COVID-19 ) outbreak had direct implications for patients with perianal fistulizing Crohn’s disease regarding their schedule for definite surgery. As a result of the primary outbreak in March 2020 , no patients had elective surgery for Crohn’s associated complex anal fistulas at our institution between March 2020 and July 2020 according to governmental restrictions (German Ministry of Health). Moreover,according to a second restriction period for elective procedures at our institution starting in November 2020 , potential procedures were postponed to 2021 . Finally, a relevant number of patients with fistulizing perianal Crohn’s disease under immunosuppression and/or maintenance therapy (e.g., biologicals) postponed their surgery to 2021 .
Preoperative assessment
All patients amenable for stem cell injection were seen in the proctological office 2 -4 wk prior to darvadstrocel treatment. Informed consent was given, including for efficacy from the ADMIRE study, innovation of the current technique, and monitoring of side effects or adverse events, surgical technique and follow-up observation. Procto-logical examination included clinical examination and proctorectoscopy to rule out abscess or proctitis in the immediate preoperative phase. No antibiotic treatment was administered; setons were controlled to be correct in place. No routine curettage of fistulas drained by setons was performed in the preoperative period, and no specific change for medical treatment was performed.
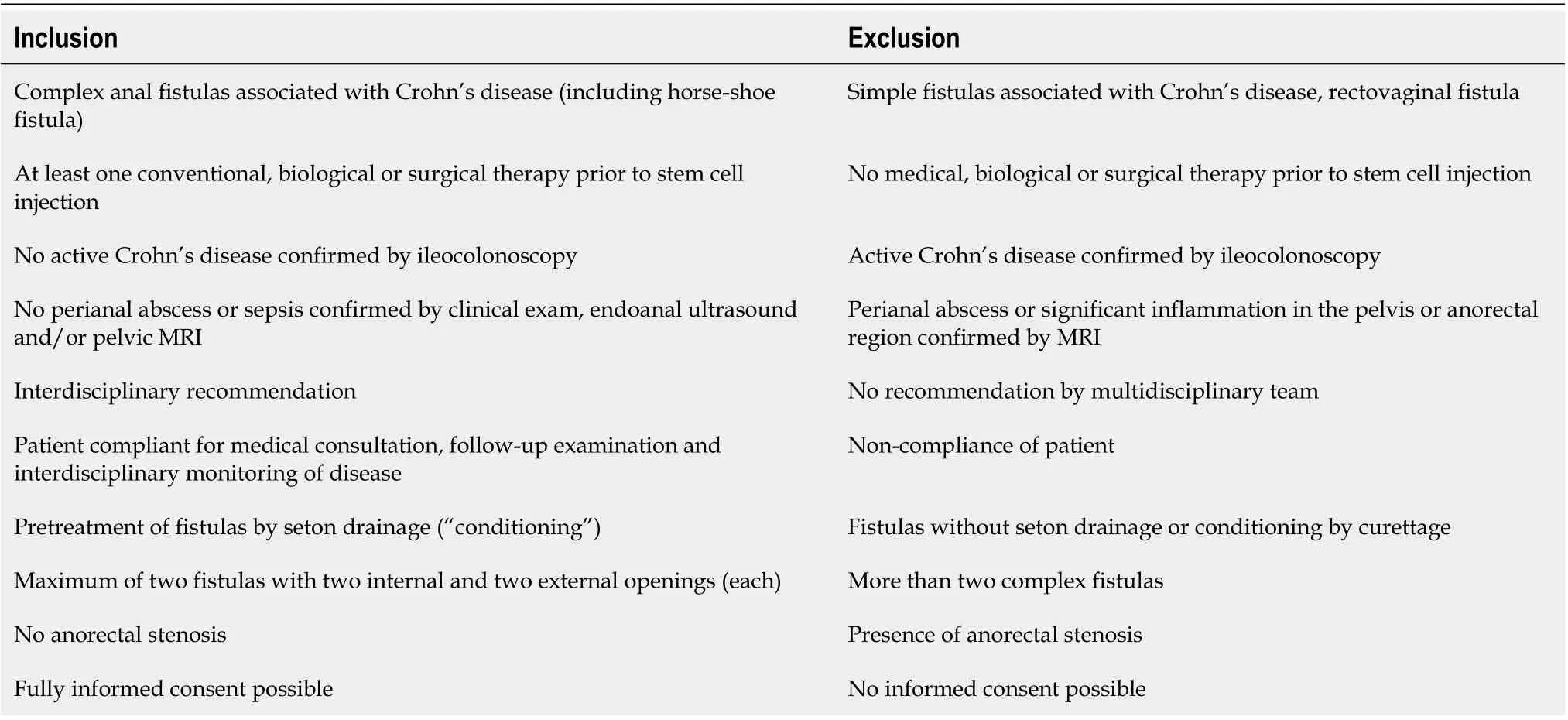
Table 1 Inclusion and exclusion criteria for administration of darvadstrocel
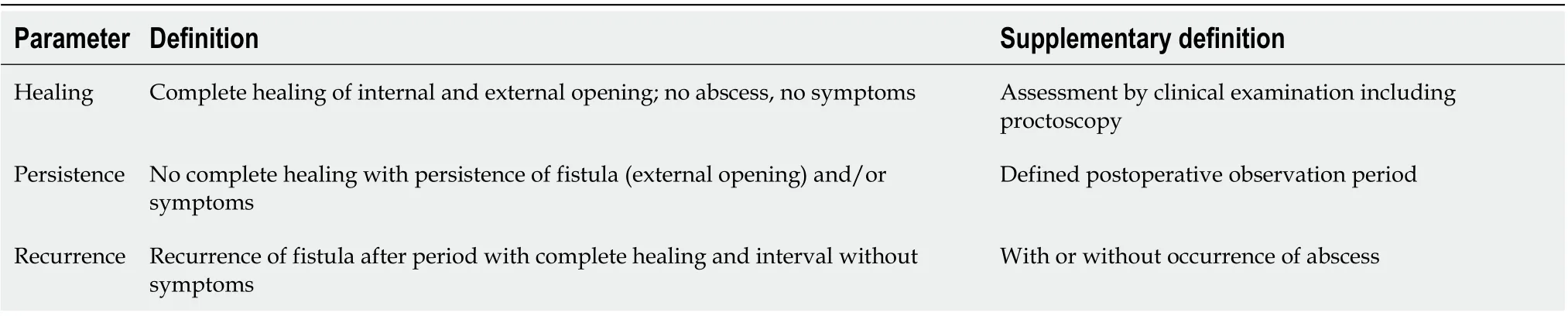
Table 2 Definitions of outcome
Surgical technique
All surgical procedures were performed under general anesthesia. The patient was placed in lithotomy position. A single-shot antibiotic prophylaxis was routinely administered (cefuroxime/metronidazole). Initially, a careful examination under anesthesia was performed to ensure that there was no presence of abscess or proctitis;moreover, assessment of fistula length, anatomy and topography according to Parks classification[10 ] was performed. After removal of setons, a vigorous curettage of the fistula tracts was performed by using a metallic curette. Additionally, injection of a sodium chloride solution (0 .9 %) was administered after curettage. No excision of the fistula tracts were conducted; however, the external openings were sparingly excised.Afterwards, the internal openings were closed by either direct suturing (absorbable suture, Vicryl 3 /0 ; Ethicon EndoSurgery, Norderstedt, Germany) or by mucosal flap(absorbable suture, Vicryl 3 /0 ) if necessary.
After preparing and resuspension of the stem cells and gentle aspiration by using a syringe and injection needles (22 -G), darvastrocel was injected according to the manufacturer's recommendations: Two vials were injected around the internal openings (transanal approach), and the other two vials were injected along the fistula tracts creating small deposits of the cell suspension along the fistulas from external openings (perianal approach). After injection, a soft massage along the fistula region was performed; finally, a sterile bandage was placed around the anal region.
Postoperatively, no specific restrictions related to feeding and mobility were present; after wound control on the first postoperative day, the patient was discharged from hospital. No specific wound management was proposed (only clear water twice a day). Maintenance therapy was given as planned prior to surgery. Neither intravenous nor oral antibiotic therapy was given in the postoperative period.
Follow-up
Regular follow-up examination was performed 2 , 4 and 6 wk after surgery in the proctological office, to obtain clinical data related to quality assurance and patient care. Moreover, follow-up examination was advised at 6 , 12 and 24 mo after stem cell injection. Additionally, gastroenterological monitoring was advised to provide regular monitoring of Crohn’s disease. As clinical follow-up was primarily indicated for routine quality control and was not indicated for study purpose, regular follow-up did not include postoperative MRI as routine examination.
RESULTS
Study population and patient characteristics
Between July 2018 and January 2021 , a total of 12 patients (6 females, 6 males) with a mean age of 42 .5 (range: 26 -61 ) years underwent stem cell therapy for complex anal fistula associated with Crohn’s disease. All patients had medical therapy (infliximab,adalimumab, vedolizumab or azathioprine), and complex fistulas did not respond to either medical or surgical treatment prior to stem cell therapy. Mean duration of Crohn’s disease was 19 .3 years (range: 7 -36 years), and median duration of perianal fistulizing Crohn’s disease was 8 .7 years (range: 1 -16 years). All fistulas had at least one conventional surgical approach to close the fistula (except seton drainage) prior to stem cell therapy; mean number of surgical attempts to close the fistula was 2 .0 (range:1 -4 ). Details on study population and patients’ characteristics are detailed in Table 3 .
Fistula characterization
All patients underwent fistula conditioning by seton drainage for a mean duration of 31 .5 (range: 6 -72 ) wk, and 4 patients had undergone fecal diversion due to severe perianal sepsis. All patients had a minimum of one complex fistula, including patients with two complex fistulas in 58 .3 % (7 /12 ). Two of 12 patients had horse-shoe fistula,and 3 of 12 had one complex fistula. In total, 21 fistula tracts were documented in 12 patients. According to Parks classification, the majority of fistulas were transsphincteric (76 %) or suprasphincteric (14 %).
Surgery
All patients underwent removal of seton, fistula curettage, transanal closure of internal opening by suture (11 /12 ) or mucosal flap (1 /12 ) and stem cell injection. No intraoperative complications or side effects were noted. Postoperative morbidity included 1 patient with fewer (without signs of perianal sepsis) on the second postoperative day.No serious adverse events were documented.
Outcome
Details on efficacy evaluation and outcome are outlined in Table 4 . At a mean followup of 14 .3 mo (range: 3 -30 mo), a healing rate was documented in 66 .7 % (8 /12 ); mean duration to achieve healing was 12 wk (range: 6 -30 wk). Four patients had either fistula persistence (n= 2 , 16 .7 %) or fistula recurrence (n = 2 ; 16 .7 %). Within follow-up,4 patients developed perianal abscess (33 .3 %) and required reoperation. From 4 patients with ileostomy, one stoma reversal was performed 2 years after fistula healing.
Focusing on patients with a minimum follow-up of 12 mo (6 /12 ) or 24 mo (4 /12 ),long-term healing rates were 66 .7 % (4 /6 ) and 50 .0 % (2 /4 ), respectively.
DISCUSSION
Despite significant progress in medical treatment, including biologicals and cell-based therapies, development of sphincter-saving surgical techniques and interdisciplinary co-working, failure rates after definite surgery for perianal fistulizing Crohn’s disease are still high[3 ,11 -13 ]. Moreover, in patients with severe and refractory perianaldisease, the decision to perform fecal diversion or even proctectomy has a tremendous impact on quality of life, particularly in younger patients. Impressed by the preliminary results of limited single-center studies and the encouraging data of the ADMIRE study[7 ,8 ], this was a retrospective single-center study analyzing routine clinical data on the application of allogenic, adipose-derived mesenchymal stem cells(darvadstrocel) for complex perianal fistula associated with Crohn’s disease, providing structured inclusion and exclusion criteria in 12 patients.
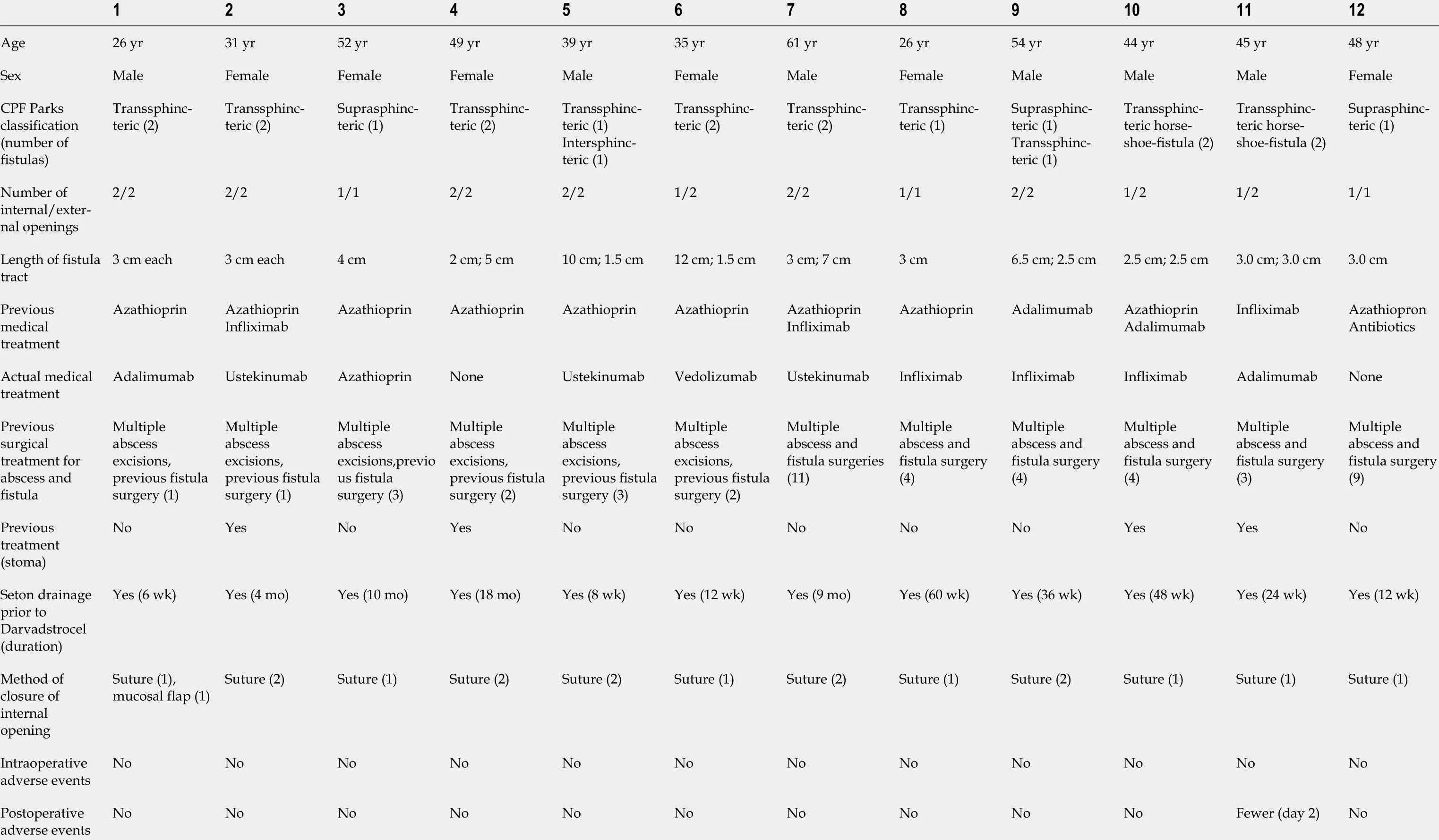
Table 3 Patient population
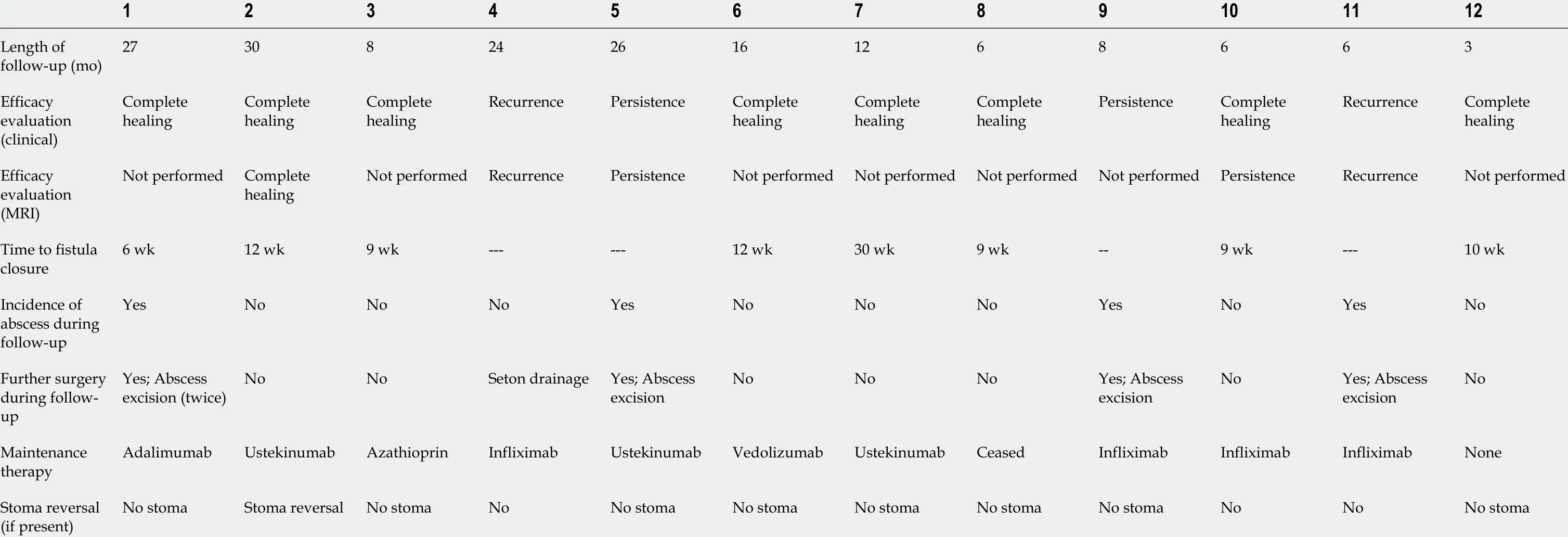
Table 4 Efficacy evaluation and outcomes
In general, the optimal surgical treatment of complex anal fistulas in patients with Crohn’s disease remains challenging. As the majority of patients need surgery for perianal fistulizing Crohn’s disease and a high proportion of patients need further surgery due to abscess and recurrent fistula, the integrity of the anal sphincter is essential for preservation of continence[3 ]. Therefore, the risk of deterioration of continence status increases with the number of surgical procedures and the invasiveness of procedures performed. For complex anal fistulas according to American Gastroenterological Association and Parks classification[9 ,10 ], transrectal flap procedures (advancement or mucosal flap repair) and the LIFT procedure can be considered as effective surgical options in stable disease and absence of proctitis and/or anorectal stenosis with acceptable healing rates[11 -18 ]; however, fecal incontinence and soiling is reported in approximately 10 % of patients after endorectal flap procedures[6 ,11 ,18 ]. Focusing on the LIFT procedure, the risk of incontinence is low, but about half of the patients need additional surgery due to recurrence[14 -16 ].The main “disadvantage” or limitation of both procedures are high complex fistulas with suprasphincteric course or multi-tract fistulas with two internal and external openings (“multiple branching tracts”). In these patients, long-term seton drainage is the favored option; alternatively, proctectomy can be considered. Based on this“surgical dilemma”, the novel therapeutic approach of local stem cell therapy seems to be an alternative for highly selected patients with multi-tract, complex fistulas.
In the meantime, a variety of limited studies demonstrated that local injection of mesenchymal stem cells can induce long-term fistula healing without the risk of incontinence and without serious adverse advents related to the mesenchymal stem cells themselves[19 -22 ]. Following the results of the multicenter, phase III randomized control trial (ADMIRE), the application of allogenic, adipose-derived, mesenchymal stem cells combined with transanal closure of the internal opening and fistula curettage, a 50 % healing rate of stem cell therapy compared with a 34 % success in the placebo group was documented after 24 wk, and healing rates were sustained to 52 wk[7 ,8 ].
Impressed by these results and personally searching for the “best option” in patients with multi-branching or two-tract complex fistula, it was the aim of the current singlecenter experience to evaluate the outcome of local injection of darvadstrocel in a highly selected group of patients. Following the current single-center experience with stem cell therapy, strict inclusion and exclusion criteria were defined. In accordance with the inclusion criteria of the ADMIRE study[7 ,8 ], only patients with complex fistulas associated with Crohn’s disease-in the majority two complex fistula, suprasphincteric fistula and horse-shoe-fistula, without active luminal Crohn’s disease (stable disease under medical treatment) and no evidence of perianal sepsis were included. In contrast, simple fistulas or rectovaginal fistulas were excluded for stem cell therapy.Moreover, in the current study, patients with single-tract intersphincteric or transsphincteric fistulas as well as relatively short single-tract fistulas (fistula length less than 3 cm) were not candidates for stem cell therapy; in these patients,advancement flap repair, mucosal flap repair or LIFT procedure was the preferred option. Within the observation period, a total of 28 patients underwent flap or LIFT procedure for complex fistula associated with Crohn’s disease (data not shown).
All patients had drainage of fistulas by seton for a minimum of 6 wk. In contrast to the ADMIRE study[7 ,8 ], 4 patients who underwent fecal diversion due to perianal sepsis related to complex fistulas years before admission to our center were included in the current study after interdisciplinary discussion, as the only alternative surgical treatment would have been a proctectomy in these patients, and patients refused this option. Finally, all 12 patients had at least one attempt to surgically close the fistula with no success; thus, all fistulas treated with stem cell therapy were recurrent complex fistula.
Focusing on surgical technique and administration of darvadstrocel, no difficulties or intraoperative morbidity were documented. One patient had fewer on the second postoperative day without any signs of perianal sepsis. No serious adverse events in the immediate postoperative course were noted.
After a mean follow-up of 14 .3 mo (range: 3 -30 mo), healing rate was 66 .7 % (8 of 12 patients). Healing was based on strict criteria and was assessed by clinical examination and proctoscopy in the follow-up period. In terms of postoperative MRI (5 /12 patients), 1 female patient with clinical evidence of fistula healing also had radiological healing as documented by MRI, whereas 3 patients had radiological recurrence (2 ) or persistence (1 ). One patient with clinical healing had radiologic persistence of fistula without signs of contrast enhancement. Focusing on patients with a minimum followup of 12 mo (6 /12 ) or 24 mo (4 /12 ), long-term healing rates were 66 .7 % (4 /6 ) and 50 .0 % (2 /4 ), respectively.
The occurrence of perianal abscess during follow-up was relatively frequent in the current collective. Four patients (33 .3 %) developed perianal abscess in the postoperative course, and surgery (abscess excision) was required (1 patient had abscess formation twice). Interestingly, the occurrence of perianal abscess was late (3 ,4 , 7 , 9 and 22 mo after darvadstrocel administration), and abscess localization was near to one former external opening. The incidence of abscess was related to recurrence in 1 patient (supralevatoric abscess with proctosigmoiditis), occurred with exacerbation of systemic disease (subcutaneous abscess with active inflammation of ileocolic region and proctitis), and was associated with fistula persistence in 2 patients. As a consequence of the relatively high incidence of perianal abscess following stem cell therapy in the current series, a more wide or radical excision of the external opening should be recommended in future procedures to prevent perianal abscess. Moreover,patients with the occurrence of abscess could not be defined “in remission”; however,there was no change in medical treatment. Therefore, the differentiation of abscess as a local problem following fistula surgery or as a problem of systemic disease with direct implications for medical treatment should be more in focus between gastroenterologists and surgeons.
Analyzing the further course of patients with long-term healing in terms of medical therapy, 1 patient had ceased maintenance therapy after recommendation of the gastroenterologist. Focusing on patients who had fecal diversion in the past, one female patient underwent stoma reversal 2 years after stem cell injection. In the other 3 patients, follow-up is still too short, as stoma reversal should be advised not prior to a minimum period of 6 mo after definite fistula surgery (1 patient), and the other two patients had recurrence.
Specifically addressing the observation period related to the COVID-19 pandemic,stem cell therapy was not performed within March 2020 and July 2020 and within a second period starting in November 2020 due to general restrictions concerning elective operations in Germany. Based on governmental restrictions and in-hospital limitations (e.g., reduced capacity in the surgical theater) as well as logistic reasons (e.g., transportation of stem cells under specific conditions) patients with stable disease and without signs of active perianal disease were postponed. This was in accordance with other European and United States experiences related to the management of patients with inflammatory bowel disease[23 ,24 ].
The current results clearly demonstrate that an innovative sphincter-sparing surgical approach including fistula curettage, transanal closure of internal openings and local injection of darvadstrocel leads to promising long-term healing rates in patients with no “effective” alternative, such as flap repair or LIFT procedure.However, fundamental limitations of this single-center experience are the small number of patients, the retrospective design, and the absence of a control group.Therefore, the definite role of local application of mesenchymal stem cells has to be discussed within multidisciplinary round tables or consensus conferences to have clear position statements[25 -28 ]. Actually, we are still in the episode of a “l(fā)earning curve” in terms of patient selection, ideal surgical technique, interdisciplinary treatment discussion, role of maintenance therapy and evaluation of outcomes, among others.Therefore, generally accepted indications and pathways of stem cell therapy for complex fistulas in Crohn’s disease cannot be derived; however, the current results should be a plea for further standardization and interdisciplinary consensus.
CONCLUSION
These single-center data demonstrate that local injection of adipose-derived mesenchymal stem cells (darvadstrocel) is safe and effective in patients suffering from perianal fistulizing Crohn’s disease. Providing long-term healing in 66 .7 % of patients,stem cell therapy seems to be an innovative and promising surgical therapy for complex anal fistula associated with Crohn’s disease. However, this single-center experience is limited due to the small number of patients and the retrospective assessment of routine clinical data related to quality control. As a technical consequence of a high incidence of perianal abscess during follow-up, a wide excision of the external opening should be recommended for future procedures. Finally, further interdisciplinary efforts including controlled studies are necessary to evaluate the definite role of stem cell therapy for complex anal fistula in Crohn’s disease.
ARTICLE HIGHLIGHTS
Research motivation
At present, failure rates after surgery for complex anal fistula associated with Crohn’s disease are still high, and surgical options in patients with recurrent and/or multitract fistula are limited.
Research objectives
The primary objective was to assess whether local stem cell injection is associated with acceptable healing rates in a routine clinical setting.
Research methods
Providing strict inclusion and exclusion criteria, 12 patients with complex anal fistulas associated with Crohn’s disease underwent local application of allogenic, adiposederived mesenchymal stem cells (darvadstrocel). Darvadstrocel was only indicated in patients without active Crohn’s disease confirmed by ileocolonoscopy and without presence of anorectal abscess. Study design was retrospective and routine clinical data were analyzed.
Research results
Twelve patients (6 females, 6 males) with complex anal fistula associated with Crohn’s disease underwent fistula curettage, transanal closure of internal openings and local darvadstrocel administration. Fifty-eight percent of patients had two complex fistulas,and seventy-six percent of the fistulas were transsphincteric. After a mean follow-up of 14 .3 mo, a healing rate of 66 .7 % (8 /12 ) was documented. Perianal abscess occurred in 33 .3 % of patients during follow-up.
Research conclusions
This single-center experience demonstrates that local stem cell injection for complex perianal fistulizing disease is safe and provides acceptable healing rates. However,conclusions are limited due to the small number of patients and the retrospective study design.
Research perspectives
Based on the current results, local stem cell injection could be a new “puzzle piece” for effective treatment of complex anal fistulas associated with Crohn’s disease.
 World Journal of Gastroenterology2021年24期
World Journal of Gastroenterology2021年24期
- World Journal of Gastroenterology的其它文章
- COVID-19 and its effects on the digestive system
- Weight loss interventions in living donor liver transplantation as a tool in expanding the donor pool: A systematic review and meta-analysis
- Disorders of the brain-gut interaction and eating disorders
- Altered profiles of fecal bile acids correlate with gut microbiota and inflammatory responses in patients with ulcerative colitis
- Chronic intestinal failure and short bowel syndrome in Crohn’s disease
- Early genetic diagnosis of clarithromycin resistance in Helicobacter pylori
