Inhaling muscle spray: A rising trend of abuse
Sohil Pothiawala, Chong King Yong, Rabind Charles
Sohil Pothiawala, Rabind Charles, Department of Emergency Medicine, Woodlands Health Campus, Singapore 768024, Singapore
Chong King Yong, Department of Emergency Medicine, Sengkang General Hospital, Singapore 544886, Singapore
Abstract Ethyl chloride was popular as an inhalant recreational drug in the 1980s. It is easily available in pharmacies as well as sold online as a topical anesthetic spray for pain relief. In recent times, its use is gaining popularity again among the youth as an inhalant drug due to its neuro-stimulatory effects. To avoid the risks associated with use of illegal drugs, and ease of availability of ethyl chloride without restrictions, there is a rising trend to use it as a “substitute” drug of abuse. In this paper, we try to highlight to the critical care and emergency physicians that majority of these cases present with predominant neurological symptoms, with occasional involvement of the cardiovascular system. The diagnosis of ethyl chloride poisoning is primarily clinical and supportive care is the mainstay of treatment, along with subsequent counseling. Ethyl chloride abuse should be considered as a differential diagnosis in young patients presenting with predominant neurological symptoms. Alongside raising public awareness, the manufacturers and retail distributors of these products have an important role to play in reducing the risk of abuse.
Key Words: Ethyl chloride; Abuse; Inhalant; Neurological; Recreational; Counselling
INTRODUCTION
Volatile substance abuse comprises of inhalation of volatile compounds such as glue,paints, sprays and fuels due to their psychoactive effects. Ethyl chloride was popular as an inhalant recreational drug in the 1980s. It is a colorless, flammable hydrocarbon with a strong ether-like odour[1]. It was originally used as a general anesthetic, but its use was subsequently discontinued considering its safety profile, unpleasant recovery phase and availability of newer superior agents[2]. It is used for cryoanalgesia to drain small abscesses and as a solvent and refrigerant in chemical industries. It is easily available in pharmacies as an over- the-counter topical anesthetic spray and also sold online for pain-relief from muscle spasm in athletes and also during tattoo and piercings. It rapidly evaporates due to its boiling point of 12 ℃, and hence produces a cold sensation and feeling of pain relief[3]. In recent times, its use is gaining popularity again among the youth as an inhalant drug to “feel high”.
DISCUSSION
Inhalants comprise of a broad range of volatile substances (Table 1). To avoid the risks associated with use of illegal drugs, and ease of availability of ethyl chloride without restrictions, there is a rising trend to use it as a “substitute” drug of abuse. The risk factors for potential abuse include male gender, low socio-economic status and middle-class youth.
People who “sniff” ethyl chloride inhale it directly from the container. During“huffing”, it is sprayed over the clothes or on a towel, and the evaporating fumes are then inhaled through the nose and the mouth. Chronic abusers use “bagging” as they can inhale higher concentration of the chemical.
The pathophysiology of ethyl chloride neurotoxicity is secondary to its rapid absorption in the blood from the lungs. Also, being lipophilic, it gets concentrated in the brain with subsequent development of a range of central nervous system effects.Acute solvent exposure appears to produce N-methyl-D-aspartate receptor inhibition,as well as it increases α1β1 Gamma aminobutyric acid, α1 glycine and 5-hydroxytryptamine receptor activation[4].
They produce dose-related continuum of effects, ranging from motor excitation at low concentrations to central nervous system depression, seizures, coma and even cardiopulmonary arrest at higher concentrations. They can also sensitize the heart muscles and some people will develop fatal arrhythmias. The exact pharmacokinetics of ethyl chloride in humans is not known, but animal model studies suggest that its metabolism involves oxidation by cytochrome P-450 and NADPH- and O2dependant reaction to produce acetaldehyde. It may also undergo conjugation with glutathioneviaglutathione-S-transferase[1].
Majority of the cases have mild, short-lasting effects. The systemic effects of ethyl chloride are described in Table 2. Acute brief inhalation can result in feeling of drunkenness, euphoria, and hallucinations. Other acute effects include dizziness,confusion, impaired short-term memory, ataxia, lack of muscle coordination and even loss of consciousness[1,3]. Inhaling high dose of ethyl chloride has depressant effect on central nervous system. It is also used for chemsex[5]. Neurological symptoms secondary to chronic abuse result in ataxia, tremors, speech difficulties, decreased reflexes, hallucinations, involuntary eye movement/nystagmus and deranged liver function. It can also affect the cardiovascular system, predisposing the patient to various cardiac arrhythmias, like ventricular ectopy, atrio-ventricular conduction defects, brady-arrhythmias, and occasionally ventricular fibrillation or asystole leading to sudden cardiac death[6]. Data regarding severe toxicity secondary to ethyl chlorideinhalation is rare, and few deaths have been reported till date. A patient developed cardiac arrhythmia along with neurological effects, subsequently leading to respiratory arrest[7].
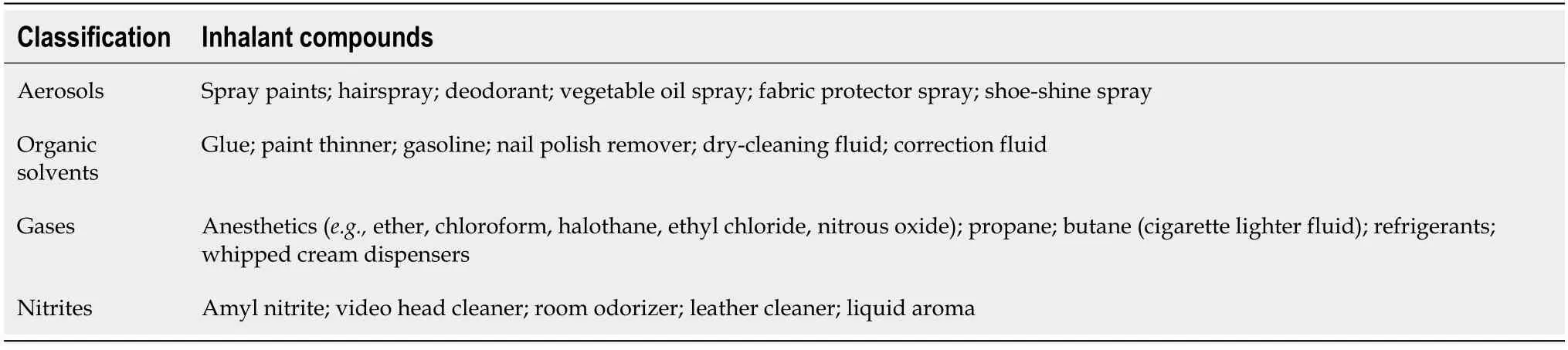
Table 1 List of common volatile substances used as inhalants
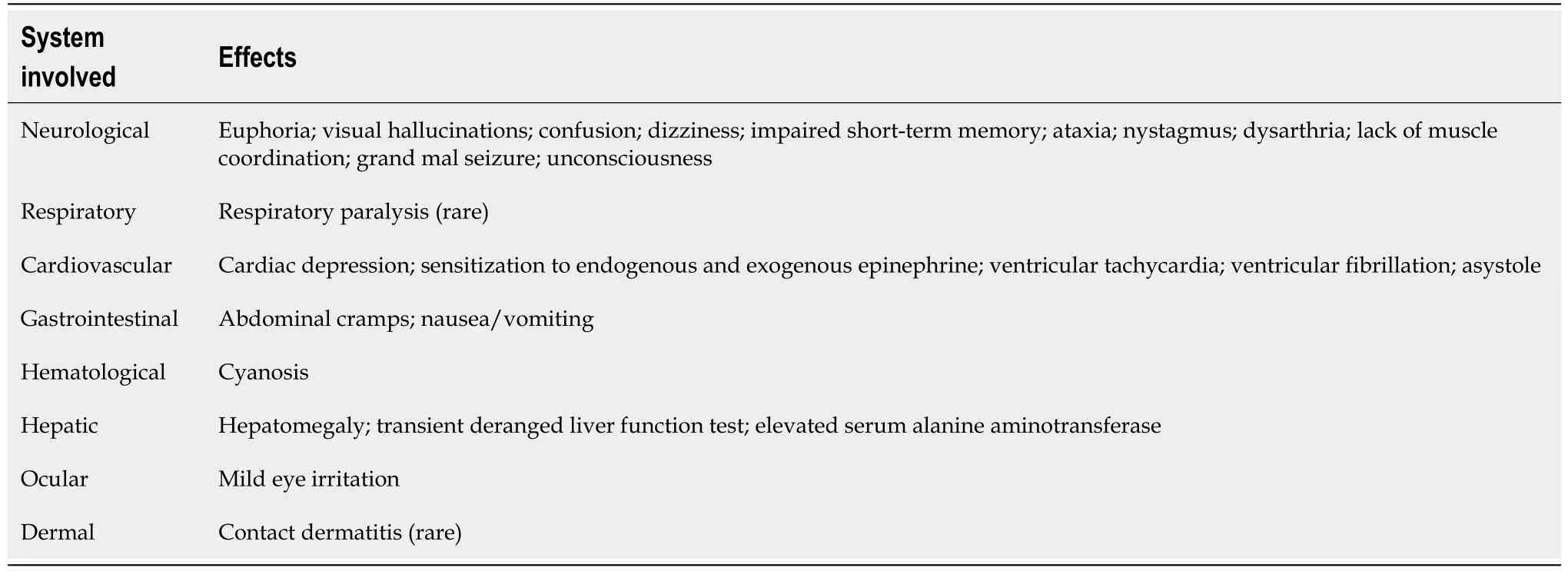
Table 2 Systemic side-effects of ethyl chloride abuse
The diagnosis of ethyl chloride poisoning is primarily clinical, based on history,including a detailed social history, and physical examination. There are no definite investigations to check the level of ethyl chloride in blood or urine. Supportive care is the mainstay of management. The initial management entails removal of the patient from ongoing exposure, which includes removing patient’s clothes as they usually spray it on their own clothes for inhalation. Patients need to be monitored for cardiac arrhythmias and neurological depression. Usually the neurological effects are transient, and resolve quickly. There are no known antidotes or any specific means to enhance elimination. Most neurological symptoms completely resolve in about a week following cessation of its inhalation[8]. Physicians should consider concomitant ingestion of alcohol or other drugs of abuse in patients who do not regain consciousness or recover rapidly in the emergency department[9]. Few patients require supplemental oxygen, and those who are unconscious and/or develop respiratory depression will require advanced airway and ventilatory support. Patients should also be specifically evaluated for traumatic injuries, which otherwise can be overlooked[6].
Once the patient is medically stable, he/she must be referred for counseling and an outpatient psychiatric evaluation, as these patients are typically young, and frequently suffer from underlying social or behavioral problems.
Also, the manufacturers and retail distributors of these products have an important role to play in reducing the risk of abuse. Similar to health hazard labelling on cigarette packets, these aerosol sprays as well as other volatile substances should have a warning logo to raise awareness among the public. Pharmacies as well as online retailers can play their part by allowing purchase of a single ethyl chloride canister.Staff at pharmacies should be trained to identify customers who look suspicious of misusing this product.
CONCLUSION
Propensity for addiction and adverse effects of ethyl chloride are underappreciated due to lack of awareness in public and healthcare professionals. We wish to raise awareness among the physicians regarding its rising trend of abuse as an inhalation agent, due to ease of availability and neuro-stimulatory effects. Ethyl chloride abuse should be considered as a differential diagnosis in young patients presenting with predominant neurological symptoms. Raising public awareness as well as improving vigilance on the sale of these products will help in reducing the burden of abuse.