Research progress of acupuncture treatment on postpartum depression in recent ten years
Lin-Yan Li;Xiao-Ying Zhang
1Department of Traditional Chinese Medicine, Wujing Community Health Center, Affiliated to Shanghai University of Traditional Chinese Medicine,Shanghai 200241,China.
Abstract In recent years, postpartum depression has gained increasing attention around the world due to its high prevalence and severe health consequences.Meanwhile, a considerable number of postpartum depression patients seek help from alternative therapies especially acupuncture, despite the limited evidence available in terms of the effectiveness of acupuncture on postpartum depression.This article summarizes the Chinese and English randomized controlled trials available on acupuncture treatment for postpartum depression over the past ten years and provides a detailed review.10 randomized controlled trials were identified in this review.The treatment regimens described in these studies included acupuncture mono-therapy, electro-acupuncture mono-therapy, or acupuncture combined with other therapies; and the treatment duration ranged from one month to three months.The Hamilton Depression Scale, Edinburgh Postpartum Depression Scale, and estradiol levels in serum were commonly used to assess the efficacy of acupuncture on postpartum depression.The published data suggests that acupuncture,including manual and electrical stimulation, can significantly reduce Hamilton Depression scores and Edinburgh Postpartum Depression scores,and can increase serum estradiol levels compared with different controls.Furthermore, fewer adverse effects were reported following acupuncture treatment than in the control treatment group.Conversely, there have also been some studies reporting inconsistent results in the effectiveness of acupuncture on postpartum depression.Therefore, acupuncture appears to be a potentially effective and safe therapy for postpartum depression,but its outcomes require validation by more rigorously designed studies.
Keywords:Acupuncture,Postpartum depression,Treatment,Chinese herbal medicine,Mechanism
Background
Postpartum depression (PPD), or postnatal depression,is a depressive disorder that occurs within 4 weeks after childbirth.It is characterized by lack of interest or pleasure, low mood, fatigue, changes in appetite or weight, sleep disturbances, feelings of worthlessness,and suicidal ideation and behaviors [1].Based on a meta-analysis involving 291 studies from 56 countries,the global incidence of PPD has been estimated to be approximately 17.7% [2].The estimated prevalence of PPD in developing countries has reached 20% [3], and is significantly higher than in developed countries such as the United States(11%-20%)[4].The prevalence of PPD in China ranges from 11.38%to 15.01%based on various screening scales, assessment methods, and ethnic backgrounds reported in different studies [5, 6].PPD is the most common complication of delivery [7]and contributes to significant adverse effects on postpartum mothers, such as reduced short-term memory [8] and partner violence [9].Furthermore,infants and children of PPD mothers have a much higher risk of cognitive and language impairments as well as behavioral problems [10, 11].Even worse,PPD is a leading contributor to self-harm, maternal suicide,and infanticide[12].
Despite the high prevalence and potentially harmful outcomes, a considerable proportion of PPD patients remain undiagnosed and untreated[13].Therefore,it is essential to develop efficacious treatment strategies.Pharmacotherapy (e.g., tricyclic antidepressants and selective serotonin reuptake inhibitors), psychotherapy(e.g., cognitive-behavioral therapy and interpersonal psychotherapy), and physiotherapy (e.g., repetitive transcranial magnetic stimulation and light therapy)are three primary interventions for PPD [14-17].Antidepressants are currently the most used treatment for depression.However, most PPD patients are hesitant to undergo pharmacotherapy due to side effects on mothers and breastfeeding infants [18].Psychotherapy and physiotherapy are not readily accessible or affordable for most individuals even though they are relatively safe [19].Therefore,exploring effective and safe treatment options for PPD is urgently needed.Meanwhile, there are increasingly more individuals seeking help from complementary and alternative treatment strategies such as acupuncture[20].
As a key component of traditional Chinese medicine(TCM),acupuncture has been used for over 2000 years.Depression is described as a collection of depressive symptoms that are characterized by the obstruction ofqi(a vital life force)circulation in TCM [21].The first documentation of the acupuncture treatment on depression was recorded in an ancient book of Chinese medicine titledThe Yellow Emperor’s Classic of Internal Medicine(about 300 B.C.),which was collected and compiled by several unknown authors over a long period [22].The acupuncture points specifically used in the treatment of depression were first recorded inA-B Classic of Acupuncture &Moxibustion(256 C.E.-260 C.E.), which is the first monograph of acupuncture and moxibustion compiled by the Chinese physician named Huangfu Mi (215 C.E.-282 C.E.) during the Western Jin dynasty [23].Recent studies have also demonstrated the efficacy of acupuncture on depression.Acupuncture is recommended as an adjuvant therapy for mild to moderate depression in the guidelines for the prevention and treatment of depressive disorders in China in 2015 [24] and the Canadian guideline of depression management in adults in 2016 [25].TheClinical Practice Guidelinesissued by the American college of physicians also demonstrates that single use of acupuncture therapy has a significant effect on depression[26].
Given the limited evidence available on the acupuncture treatment on PPD and the unsatisfactory efficacy of other therapies, research regarding acupuncture therapy on PPD remains of potential value.This article seeks to assess the clinical efficacy and safety of acupuncture therapy on PPD and provide guidance for health professionals and patients.
Methods
Search strategy
The literature published was searched in multiple electronic databases, including PubMed, Google Scholar, China National Knowledge Infrastructure, the Wangfang database, and the Chinese Science and Technology Periodical Database.In addition,reference lists of included studies were also searched.Search terms included: acupuncture, electro-acupuncture,psychotherapy, traditional Chinese medicine, or TCM and postpartum depression or PPD, postnatal depression.After filtering for articles in English and Chinese with human participants published from January 1, 2010 to December 31, 2020, 257 full text studies (26 English articles and 231 Chinese articles)were identified.
Inclusion criteria
Studies were included as follows: participants met the criteria for the diagnosis of postpartum depression;All types of acupuncture were included: manual acupuncture, electro-acupuncture, auricular acupuncture, or acupuncture combined with other therapies (antidepressant, psychotherapy or TCM);acupuncture used in the treatment group, while the control group received a placebo or drugs,psychological therapy or herb; study design was limited to randomized controlled trial.
Exclusion criteria
Uncontrolled studies, observational studies and case studies were excluded; literature were excluded if the data was unclear.
Search result
10 studies were included in this review after excluding 247 studies that did not meet the inclusion criteria.The summary of 10 included studies were presented in Table 1.
Result
Possible underlying mechanisms of acupuncture treatment on PPD
The etiology of PPD remains elusive and refers to a combination of socio-demographic, psychological, and biological risk factors [27].Likewise, the precise mechanisms of underlying effects of acupuncture on PPD are not well understood.From the perspective of modern medicine, acupuncture appears to have antidepressant effects by controlling the quantity of monoamine neurotransmitters, improving sex hormone levels, enhancing the expression of neurotrophic factors, suppressing cytokines, and decreasing inflammatory reactions [28-29].Most acupuncture mechanism studies involve animal models and focus on the regulation of a specific system such as the neuroendocrine system, central nervous system, and immune system.Few studies have addressed the interaction between systems, and the targets of acupuncture in multi-system regulation[30].
As an integral part of TCM, acupuncture involves needling acupoints of the body to restore the balance ofqiand cure disease [31].Based on the TCM theory,PPD refers to a disturbance to the spirit and the disharmony of theQimechanism of the five viscera,and can regulate emotional distress and relieve postpartum symptoms from many aspects, such as by soothing the liver, balancing yin and yang, adjusting the five viscera,and reconcilingqiand blood[32].
The clinical efficacy of acupuncture treatment on PPD
Acupuncture is one of the most popular complementary and alternative therapies in the world.According to the WHO Traditional Medicine Strategy 2014-2023, 103 countries have approved acupuncture therapy and 18 countries provide health insurance coverage [33].Acupuncture is widely used in the treatment of depression.A cross-sectional study conducted by Wang et al.in 2018 mentioned that depression ranked second among all acupuncture indications, and acupuncture has been a popular alternative for mental health treatment in the United States [34].Edinburgh Postpartum Depression Scale(EPDS) and the Hamilton Depression Scale (HAMD)are two commonly used screening and efficacy assessment tools used in PPD-related studies [35].At present, clinical research on PPD treatment with acupuncture mainly use acupuncture or electro-acupuncture as monotherapy or in combination with other therapies as the treatment group.The first-line antidepressants—selective serotonin reuptake inhibitors including citalopram, fluoxetine, paroxetine and sertraline,are commonly used as the control group[36].
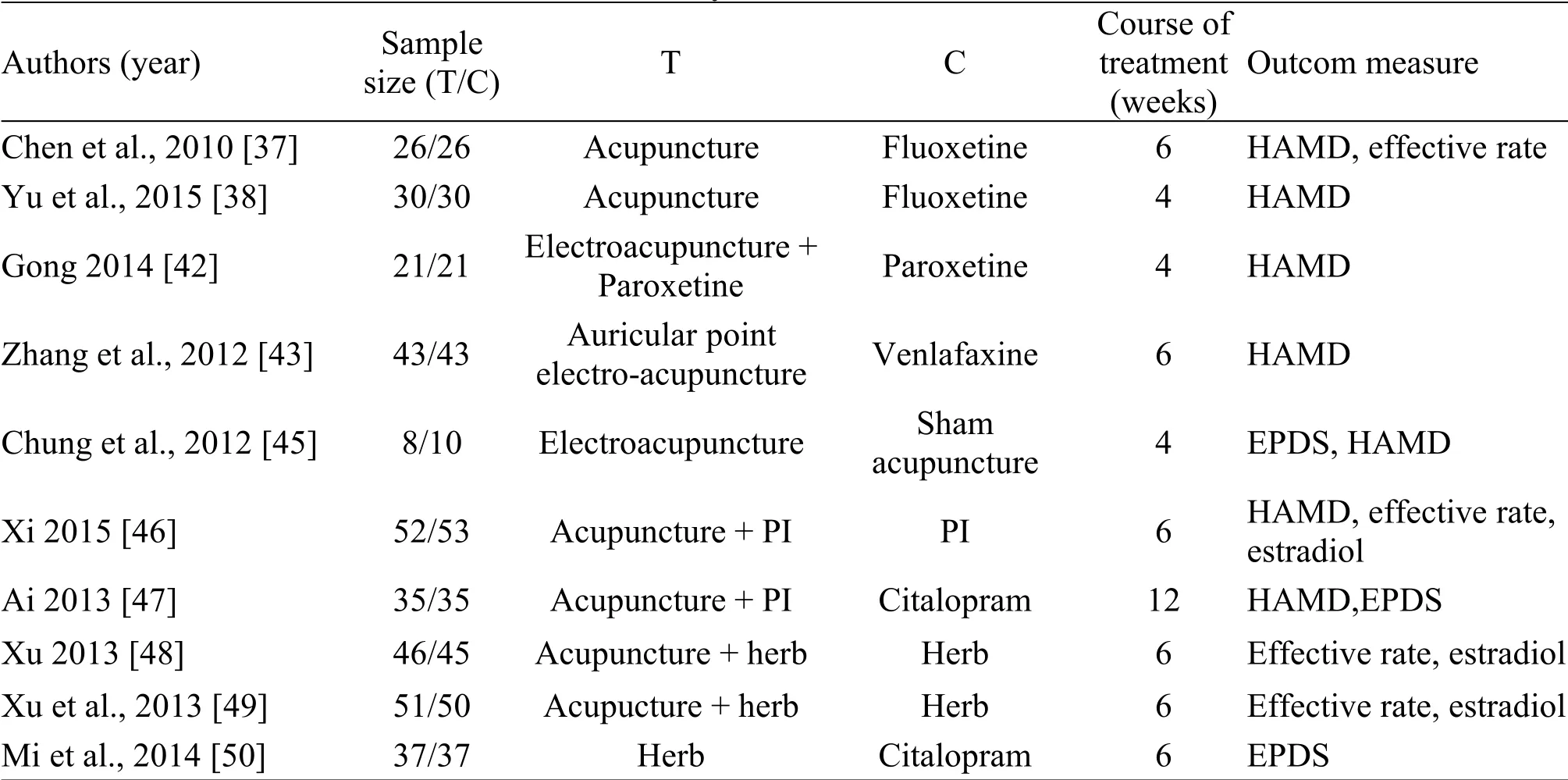
Table 1 Summary of included clinical studies
Manual acupuncture as monotherapy for PPD
Manual acupuncture is the traditional form of acupuncture in which needles are inserted at recognized acupoints and are manually stimulated.Several clinical trials have been carried out comparing acupuncture monotherapy with antidepressants to assess the effectiveness of acupuncture on PPD.A study conducted by Chen et al.recruited a total of 52 postpartum women and randomly divided them into the observation group treated with acupuncture and the control group that received fluoxetine; there were 26 women in each group.The acupoints included Baihui(DU20), Sishencong (EX-HN1), Neiguan (PC6), Hegu(LI4), Taichong (LR3), Sanyinjiao (SP6), and Zusanli(ST36).The treatment lasted for 30 min each time and was repeated for six weeks.The HAMD was assessed at 2, 4, 6 weeks after the treatment to assess efficacy.The findings revealed that both acupuncture and fluoxetine resulted in a reduction in HAMD scores and there was no statistically significant between group differences in HAMD scores at three different time points.In terms of adverse events,the fluoxetine group reported 4 cases of nausea, 2 cases of dizziness, and 4 cases of loss of appetite in the control group, while there were no reported adverse effects in the observation group.The results indicated that manual acupuncture as monotherapy was effective and highly safe for PPD [37].Similarly, Yu et al.randomly assigned 60 PPD patients to the treatment group and the control group, with 30 cases each.The treatment group received 13 ghost acupoints for four weeks,while the control group received fluoxetine for four weeks.Thirteen ghost points were developed by Chinese acupuncturist and herbalist Sun Simiao (581 C.E.-618 C.E.) to treat mental disease [38].The effectiveness of acupuncture was measured by the HAMD score at baseline and after four weeks of treatment.The findings showed that both the 13 ghost acupoints and fluoxetine treatment could significantly reduce the HAMD scores and there was no significant between-group difference.Additionally, no adverse events were reported in this trial[39].
Electro-acupuncture as monotherapy for PPD
Electro-acupuncture is the preferred form of acupuncture needling at recognized acupoints and is stimulated by a device generating electric pulses,which is more reliable and adjustable than manual acupuncture due to its ability to objectively and quantifiably establish the stimulation frequency and intensity [40].A previous study also found that electro-acupuncture had similar antidepressant effects to fluoxetine regarding restoring normal concentration of glial cell line-derived neurotrophic factor in the serum of patients with depression[41].
Two randomized control trials (RCTs) have investigated the effectiveness of electro-acupuncture on PPD.Gong et al.recruited 42 PPD patients and randomized them to the observation group (paroxetine combined with electro-acupuncture) and the control group (paroxetine) with 21 cases each.HAMD was assessed at 5 different time points (1, 2, 4, 6, and 8 weeks after treatment) to analyze the clinical efficacy.The results showed that in the observation group, the HAMD score declined significantly compared with the control group in the first and second weeks (P<0.01),indicating that electro-acupuncture was effective in treating PPD [42].Another RCT carried out by Zhang et al.in 2012 investigated the effectiveness of auricular-acupuncture on PPD.A group of 125 PPD patients were randomly assigned to three groups,including the auricular point electro-acupuncture group(43 cases), the auricular-acupuncture group (39 cases),and the venlafaxine group (43 cases, drug group).The auricular points included endocrine, liver, heart,sympathetic, and ear Shenmen.The treatment lasted six weeks, and the HAMD score was used at baseline and at the endpoint to evaluate efficacy.The outcome results showed that that auricular point electro-acupuncture group (95.3%) was superior to the auricular-acupuncture group (82.0%) and the drug treatment group (81.4%) in lowering the HAMD scores, and no adverse event was mentioned in this trial[43].
Electro-acupuncture versus sham-acupuncture
In recent years, sham acupuncture has been utilized as the placebo group in acupuncture treatment studies.A previous study showed that the credibility of sham-acupuncture was high [44].In 2012, a randomized, double-blind, placebo-controlled trial was conducted by Chung et al.in Hong Kong, and 20 participants with six months mild PPD were randomized for treatment either by electro-acupuncture or non-invasive sham-acupuncture.Subjects in the electro-acupuncture group were needled at cranial and body acupoints, while the non-invasive sham acupuncture group were treated at the same acupoints using placebo needles with the blunt needle not fixed inside the copper handle.Acupoints included Baihui(DU20), Sanyinjiao (SP6), Sishencong (EX-HN1),Yintang (EX-HN3), Taichong (LR3), Neiguan (PC6).The EPDS and the 17-item Hamilton Depression Rating Scale(HDRS17)was adopted to assess efficacy,while adverse events were assessed using open-ended questions.Treatment was given twice a week for 4 consecutive weeks.The results showed that there was a significantly greater reduction in HDRS17 scores from baseline compared with the 4-week post-treatment evaluation in both groups, while there were no significant between-group difference in the EPDS and HDRS17 scores.Both groups reported similar adverse events including needle site pain, headache, dizziness,but there were no between-group differences.The results suggested that both electro-acupuncture and non-invasive sham acupuncture contributed to alleviate the depressive symptoms.However, further studies with larger sample sizes are needed to confirm this finding owning to the small sample size and high attrition rate in this study[45].
Acupuncture combined with psychological intervention
Varieties of researchers have focused their attention on the effectiveness of acupuncture combined with psychotherapy.In 2015, Xi and Wang recruited 158 subjects with PPD and assigned 52 cases to the acupuncture group, 53 cases to the psychological intervention group,and 53 cases to the treatment group(acupuncture plus psychological intervention).Seven acupoints were used in this study, including Baihui(DU20), Sishencong (EX-HN1), Neiguan (PC6), Hegu(LI4), Taichong (LR3), Sanyinjiao (SP6), and Zusanli(ST36).Treatments consisted of 30-min sessions,which were repeated for 6 weeks.HAMD,5-hydroxytryptamineand estradiol were used at six weeks post-treatment to assess the efficacy.The results indicated that the treatment group (acupuncture plus psychological intervention) was significantly superior in reducing the HAMD scores and in increasing 5-hydroxytryptamine, estradiol levels when compared to the psychological intervention and the acupuncture groups.Further, there was no significant difference between these two latter interventions (P> 0.05),suggesting that both acupuncture and psychological intervention are effective in treating PPD, while combining acupuncture and psychotherapy could further enhance the effectiveness of each intervention alone and result in a more powerful therapeutic effect.Furthermore, the combination of acupuncture with psychotherapy was effective in improving the PPD by regulating the levels of 5-hydroxytryptamineandestradiol[46].
In another RCT, 70 subjects with PPD were equally divided into treatment and control groups.The treatment group was given acupuncture plus psychological intervention, while the control group was treated with the antidepressant citalopram.The acupoints included Baihui (DU20), Guanyuan (RN4),Shenmen (HT7), Ganshu (BL18), Xinshu (BL15), and Sanyinjiao (SP6).The intervention sessions lasted 30 min and were repeated for 3 months.HAMD and EPDS scores were evaluated at baseline and at the endpoint.Acupuncture combined with the psychological intervention (88.6%) resulted in significantly lower HAMD and EPDS scores than citalopram treatment (82.9%), and there was a significant between-group difference.In addition, 40%cases in the control group reported side effects including nausea, vomit, dizziness, and heart palpitations, while no adverse events were reported in the treatment group[47].
Acupuncture combined with Chinese herbal medicine
Investigations regarding the combination of acupuncture with Chinese herbal medicine have also been preferred by many scholars.In a randomized,controlled and blind study in 2013, 180 subjects were assigned to the following interventions: Xiaoyaosan(group A), acupuncture plus moxibustion (group B),Xiaoyaosan plus acupuncture and moxibustion (group C), or to a placebo (group D).The acupoints included Qimen (LA14), Taichong (LR3), Fenglong (ST40),Pishu (BL20), Neiguan (PC6), Zusanli (ST36), and Tiantu(RN22).EPDS was used at baseline and at 1,2,4, and 6 weeks after the treatment to evaluate the clinical efficacy.Serum estradiol and progesterone levels were measured at baseline and endpoint.The EPDS score in group C was significantly lower than in the other groups.Furthermore, the serum levels of estradiol and progesterone in groups A, B, and C were significantly higher than that in group D (placebo group) [48].These findings were similar to another RCT conducted by Xu et al., which involved 201 PPD patients presenting with symptoms of kidney-deficiency and liver-depression that adopted the same methodology and assessment tools[49].
In another study involving 74 PPD patients with spleen deficiency and liver depression, the treatment group with 37 subjects received acupuncture and TCM decoctions to strengthen the spleen and regulate the liver,while the control group comprising 37 cases was given the antidepressant citalopram.The acupoints included Fenglong (ST40), Zusanli (ST36), Tianshu(ST25),Qimen(LA14),Taichong(LR3),Pishu(BL20),Neiguan (PC6), and Tiantu (RN22).EPDS was assessed before and after the treatment to measure efficacy.The interventions lasted for 20 min and were repeated every day for six weeks.The EPDS scores in the treatment group were significantly lower than those of the control group[50].
Non-clinical studies of acupuncture treatment on PPD
A previous systematic review and meta-analysis evaluated the effectiveness of acupuncture on PPD,but the results remain controversial.The meta-analysis conducted by Li et al.in 2018 involved 9 RCTs with a total of 653 subjects and suggested that acupuncture was safe and effective for patients with PPD [51].Similarly, in 2017, Wang et al.gathered 14 articles of clinical RCTs evaluating acupuncture for the treatment of PPD and concluded that acupuncture was an effective treatment for PPD, although more well designed RCTs were needed to verify their conclusion[52].Animal experiments have also indicated that acupuncture may have potential antidepressant effects[53].In contrast, another meta-analysis involving eight RCTs reported that acupuncture could significantly reduce HAMD scores in postpartum women, but no additional benefits from acupuncture treatment were observed when compared to conventional treatments,indicating that the effectiveness of acupuncture in PPD differed when compared to different controls[54].
Implications for future research
This literature review suggests that acupuncture appears to be a potentially effective and safe therapy for PPD, but this intervention requires further verification by more rigorously designed studies.The published research currently has limited evidence for or against the use of acupuncture for treating depression and related mood disorders.
Limitations of this study
While the published data may suggest that acupuncture shows a tendency towards being an effective and safe treatment option for PPD, there are still some limitations in the acupuncture studies reported to date.First, most of the clinical trials in the area of acupuncture treatment for PPD had small sample sizes,and some studies were biased and adopted poor methodology, and thus provided low-quality evidence.Second, most studies concluded that acupuncture effectively and safely improved PPD, but were unable to provide details on the underlying mechanisms involved.Third, the majority of the published studies on acupuncture treatment for PPD originated in China,which may result in a publication bias.Future acupuncture trials need to integrate evidence-based medicine methodology with traditional therapies,utilize larger study samples with acupuncture interventions, and include high-quality RCTs.Many published studies of acupuncture have not been translated into English, and this may limit the understanding of the procedures and findings.Acupuncture research is particularly challenging to carry out, owing to a lack of adequate placebo interventions, which limits the quality of the available evidence.
Conclusion
In conclusion, the findings showed that acupuncture appeared to be effective at treating PPD in terms of certain outcomes, but the resulting evidence is insufficient and its effectiveness needs to be further verified in more well-designed studies, especially in terms of randomization and blinding.Our findings are similar to those of three recent meta-analyses.Considering the severe consequences of PPD and the potential value of acupuncture interventions,acupuncture deserves greater attention from health policymakers and is worthy of clinical promotion.Further rigorous research on the role of acupuncture in the treatment of PPD, will likely lead to the adoption of acupuncture as an important therapy for PPD and improvement of patient management, and will ultimately provide additional benefits to patients.
- TMR Non-Drug Therapy的其它文章
- A series of studies on acupuncture treatment of knee osteoarthritis by Chinese scholars
- Acupuncture-based treatments on cervical spondylosis of vertebral artery type
- Comparison of horse and cow milk on sleep disorders in children with attention deficit hyperactivity disorder: a double-blind randomized clinical trial study
- Evaluation of blended internet and face-to-face continuous medical education for cupping providers in Saudi Arabia
- Association between drinking behavior and sleep duration in Chinese adults:findings from the China Health and Nutrition Survey

