Traditional Chinese medicine poisoning in the emergency departments in Hong Kong: Trend, clinical presentation and predictors for poor outcome
Rex Pui Kin Lam, Eric Ho Yin Lau, Wai Lam Yip, Joe Kai Shing Leung, Matthew Sik Hon Tsui
1 Emergency Medicine Unit, Li Ka Shing Faculty of Medicine, the University of Hong Kong, Hong Kong, China
2 Accident and Emergency Department, Queen Mary Hospital, Hong Kong, China
3 Accident and Emergency Department, Pamela Youde Nethersole Eastern Hospital, Hong Kong, China
4 School of Public Health, Li Ka Shing Faculty of Medicine, the University of Hong Kong, Hong Kong, China
Dear editor,
Traditional Chinese medici ne (TCM) is popular in many countries, especially in the Chinese population.[1,2]In Hong Kong, it has been estimated that around 15% of the population consumed Chinese medicine products/herbs in the preceding month. Common reasons for consumption include regulating bodily functions, curing disease, and building up health.[3]In a survey conducted in a local emergency department (ED), 1.4% of ED patients reported TCM use within one week of attendance; among them, 7.6%exhibited TCM-related toxicity.[4]A population-based survey in Hong Kong revealed that 2.3% of over-the-counter TCM users reported at least one TCM-related adverse effect in the previous year, especially in those with a lower education level and less access to reliable information.[5]
While most TCM-related toxicities are mild,[4]the medical literature is not lacking in reports of severe adverse reactions after the consumption of certain Chinese herbs,such asAconitum[6]and theDaturaspecies.[7]According to the 2017 Annual Report published by the Hong Kong Poison Information Center, Chinese herbal medicine (CHM)and proprietary Chinese medicine (PCM) ranked number 5 and 15 in the most common poisons to which individuals are exposed, respectively.[8]In Hong Kong, TCM poisoning accounts for 0.2% of all acute adult medical admissions[9]and aconitine poisoning is the most common cause of TCMrelated hospital admission.[10]
In spite of a lack of training in TCM, emergency physicians are often called upon to manage patients with acute toxicity related to TCM use in the ED. A lack of knowledge about TCM may lead to delayed recognition,misdiagnosis, and inappropriate management. While offering complete TCM training to all emergency physicians is not feasible or necessary, they may benefit from training that specifically targets TCM products/herbs with a higher propensity for serious adverse effects. Proper risk assessment of individual TCM products/herbs requires an understanding of the overall toxic profile of all TCM poisonings encountered in ED settings.
Thus far, most literature about TCM poisoning has either focused on individual products/herbs/ingredients[6]or on a particular toxidrome caused by TCM.[7]For this reason,a knowledge gap exists in regard to the overall trend and patterns of TCM toxicities in the ED. This information has a significant implication for the future training of emergency physicians since it highlights TCM ingredients with the highest risk and the greatest need for focused training.
Thus, we conducted a retrospective study in two EDs in Hong Kong to characterize the trend, clinical presentations,and health resource utilization of TCM poisoning, and to further identify predictors of a poor outcome.
METHODS
Study design and setting
We studied consecutive patients who presented to the Accident and Emergency Department (A&E) at Queen Mary Hospital (QMH) and Pamela Youde Nethersole Eastern Hospital (PYNEH) for TCM-related toxicity over an 11-year period between 1 January 2006 and 31 December 2016. We referenced the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE)guidelines when reporting this study.[11]
The two study centers are major A&Es on Hong Kong Island, with an annual ED attendance of approximately 130,000 and 150,000, respectively. Each center has its own ED toxicology team, and each team is comprised of a group of emergency medicine specialists with post-graduate training in clinical toxicology. Patients with acute poisoning presenting to these two centers are either managed directly by the respective ED toxicology teams, or indirectly through internal consultation. Both centers run their own emergency medicine wards, which enables extended care to be provided to poisoned patients. Both are recognized training centers of clinical toxicology with regular monthly audits of poisoning management. When it is necessary, clinicians can consult the Hong Kong Poison Information Center for management advice. They can also send patient serum and urine specimens, herbal remnants, left-over herbs or other specimens to the Toxicology Reference Laboratory of the Hospital Authority (HA) for chemical analysis.
In QMH, data from all poisoned patients presenting to A&E have been prospectively collected and entered into an electronic clinical toxicology database by a designated nurse since 2005. Thus, it is possible to retrospectively identify eligible cases in QMH by reviewing the database.In PYNEH, diagnostic codes using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) by emergency physicians are mandatory for all A&E consultations. We searched the Clinical Data Analysis and Reporting System (CDARS) of HA (an electronic repository that stored diagnostic codes and electronic information of all A&E consultations) for potentially eligible cases using a broad set of diagnostic codes which emergency physicians may use in recording TCM poisoning in the ED (Table 1).
Selection of subjects
We recruited patients with a diagnosis of TCM-related poisoning within the study period. We excluded patients with:(1) exposure to a product not fulf illing the def inition of TCM in Hong Kong (see below); (2) missing information about the TCM ingredients; (3) exposure to a normal dose with no clinical effects; (4) clinical symptoms not explained by the TCM consumed; (5) allergic reaction to TCM product/herbs;and (6) adverse reactions due to drug interaction with Western medicine, which was not the focus of our study.
Def initions
Chinese herbs are widely used as food ingredients,health supplements, and medicine. Indeed, several plant species are used not only in TCM, but also in traditional or proprietary remedies in other Asian countries. As such, there is a need to clearly def ine TCM to minimize misclassif ication of exposure.
We referenced the Chinese Medicine Ordinance (Cap.549) in Hong Kong, which provided clear definitions for local regulation of TCM use. In this study, we def ined TCM as: (1) any materials of herbal, animal, or mineral origin prescribed by a registered Chinese medicine practitioner or a listed Chinese medicine practitioner; or (2) any materials of herbal, animal, or mineral origin self-prescribed or purchased over-the-counter that were customarily used by the Chinese and registered in Hong Kong. We also included TCM that was listed in the Pharmacopoeia of the People’s Republic of China.[12]
We further classified TCM into CHM and PCM,according to the Chinese Medicine Ordinance (Cap. 549).In this study, CHM refers to the Chinese herbal medicines specified in Schedule 1 and Schedule 2 of the Ordinance(https://www.elegislation.gov.hk/hk/cap549) and PCM refers to any proprietary product composed solely of any CHM or any materials of herbal, animal or mineral origin customarily used by the Chinese that is formulated in a finished dose form (such as pills or medicinal oils) and is delivered with a curative or health claim.[13]
We further defined acute toxicity as the adverse effects of a substance resulting either from a single exposure or from multiple exposures in less than 24 hours and the adverse effects should occur within 14 days of TCM consumption.[14]
Outcome
A poor outcome was defined as a composite of death,ICU admission, electrical therapy, antiarrhythmic agents,inotropic support, intubation and mechanical ventilation,renal replacement therapy, or extracorporeal membrane oxygenation (ECMO) during the index hospitalization.
Data collection
Medical records of all eligible cases were reviewed,and data were extracted by an investigator trained in clinical toxicology. Demographic data, TCM product/herbs used,clinical presentation, reasons of exposure, laboratory findings (including analytical findings in the Toxicology Reference Laboratory), consultation records from Hong Kong Poison Information Center, health resource utilization,and clinical outcomes were recorded using a standardized data collection form. We evaluated the whole clinical course of each case (from ED presentation to ED discharge/hospital discharge/death) and graded the severity of TCM toxicity using the Poison Severity Score (PSS) as: 0=none, 1=minor,2=moderate, 3=severe, and 4=fatal poisoning, based on the most severe clinical features (including both subjective symptoms and objective signs). The PSS has been validated for a wide variety of poisoning.[15]
Data analysis
We calculated the ED incidence of TCM-related visits per 100,000 attendances over the study period and evaluated the trend using Poisson regression with the logarithm of total ED attendance as the offset term. We then characterized the clinical presentations and health resource utilization of TCM toxicity using descriptive statistics. Missing values were not inputted. We excluded cases with missing information on the herbal ingredients from data analysis, since their eligibility for inclusion could not be ascertained.
We stratified the data and compared the pattern of clinical toxicities of CHM and PCM exposure. Two patients consumed both CHM and TCM in our study. Therefore,we performed a sensitivity analysis by excluding them in the comparison to determine whether the f indings remained robust. We studied the differences in proportions between groups using the Pearson’s Chi-square test (or the Fisher’s exact test where appropriate). We compared the mean values of the variables of interest across different groups using the Student’st-test. For variables that did not follow a normal distribution, we calculated the median and interquartile range(IQR) and used the Mann-WhitneyUtest for analysis.
We then performed univariate analysis to identify factors associated with a poor outcome. Factors that were significantly associated with a poor outcome (P<0.05)in univariate analysis were entered into a multivariable backward logistic regression model to control for the confounding factors and to identify independent predictors.The SPSS for Window version 25.0 was used for data analysis. A two-tailedP-value <0.05 was considered statistically signif icant.
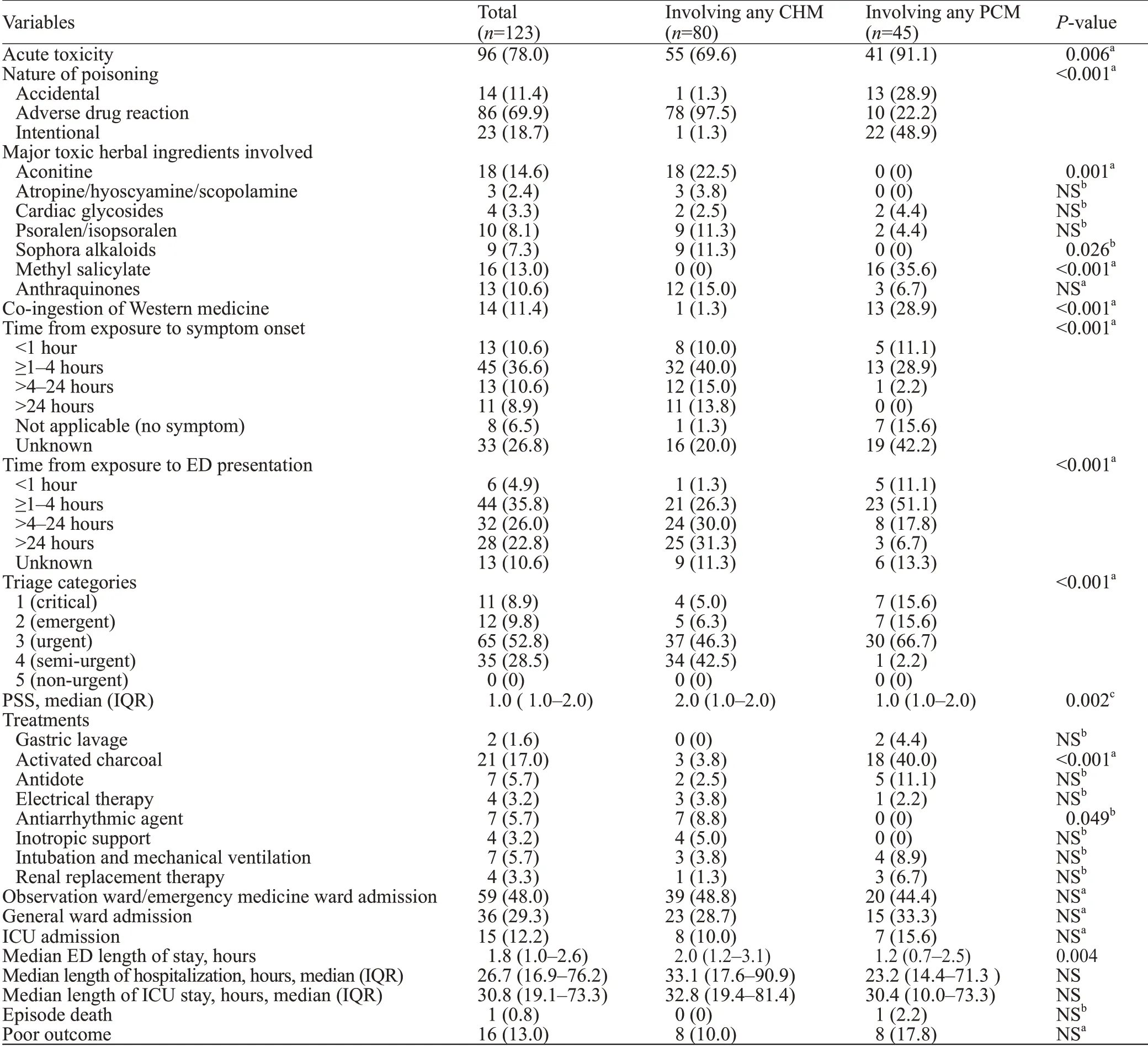
Table 1. Clinical presentations of TCM-related toxicities and comparison of patients with any CHM or PCM exposure, n (%)
RESULTS
We identified 314 episodes (152 in QMH and 162 in PYNEH) and reviewed 280 episodes after removal of duplicates. We excluded 157 episodes based on the predefined criteria. Among the 123 episodes included, 78 involved CHM, 43 involved PCM, and 2 involved both(Figure 1). The mean annual incidences of TCM, CHM,and PCM poisoning were 4.19, 2.65, and 1.47 per 100,000 ED attendances, respectively. Over the study period, the incidence of CHM toxicities increased signif icantly, though the rise was modest (odds ratio [OR] 1.09,P=0.027, 95%confidence interval [CI] 1.01-1.18), while PCM toxicities(OR0.96,P=0.399, 95%CI0.88-1.05) and the overall trend remained static (OR1.05,P=0.178, 95%CI0.98-1.12).
The 123 studied episodes involved 122 patients (one patient presented with aconite poisoning twice over six months). Two clusters of poisoning were identified: one cluster involved three members of a family who suffered from neurotoxicity after consumption ofCassytha f iliformispicked from the wild that was contaminated byGelsemium elegans; the other involved seven members of a family who suffered gastrointestinal toxicity, two of whom suffered from liver derangement after consuming the root ofSauropus spatulifolius(Longliye).
The mean age of the patients was 49.4 years (range 1-95 years), and the female-to-male ratio was 1.8:1 (78 women and 44 men). Adverse reaction to TCM accounted for more than half of the studied episodes, and exposure was confirmed with laboratory analysis of patient/herbal specimen in 44 episodes (35.8%). Overall, the median PSS was 1.0 (IQR 1.0-2.0). The patterns of consumption, clinical presentations, severity of toxicities, treatments, and outcomes are summarized in Table 1.
The clinical presentations of CHM and PCM toxicities differed significantly in many aspects (Table 1). While the majority of CHM toxicities were adverse drug reactions,almost half of PCM poisonings were intentional. Toxic herbal ingredients, such as aconitine and Sophora alkaloids,were only seen in CHM poisoning. Salicylate poisoning was only seen in patients who ingested PCM that contained methyl salicylate. Patients with PCM toxicities tended to present earlier after exposure, have co-ingestion of Western medications, receive more urgent triage ranking and activated charcoal treatment. On the other hand, patients with CHM toxicities had a higher median PSS, a longer ED stay, and a higher chance of being given antiarrhythmic agents.
The toxic profiles of the seven toxic herbs, including their median PSS, organ system where the most symptomatology occurred, common clinical presentations(in descending order of frequency), and interventions given,are presented in Table 2.
Cardiac toxicities were the most severe in patients exposed to aconitine alkaloids and cardiac glycosides. The majority of patients with aconite poisoning (16/18) developed more than one arrhythmia during their clinical course, among whom only one had a history of heart disease. In our cohort,exposure to aconitine alkaloids accounted for the majority of those who received electric therapy. Administration of antiarrhythmic agents and inotrope was related to aconite poisoning. One patient with aconite poisoning developed cardiac arrest longer than one hour and survived after prolonged resuscitation without the use of ECMO.
Neurological toxicities were the most severe in patients who had been exposed to atropine/hyoscyamine/scopolamine, Sophora alkaloids, and methyl salicylate. Five patients with methyl salicylate poisoning complained of dizziness, while four experienced a decrease in sensorium,warranting intubation, and mechanical ventilation. Metabolic acidosis occurred in two patients, and three were given haemodialysis. One patient with advanced malignancies,who deliberately drank medicine oil that contained methyl salicylate, died.
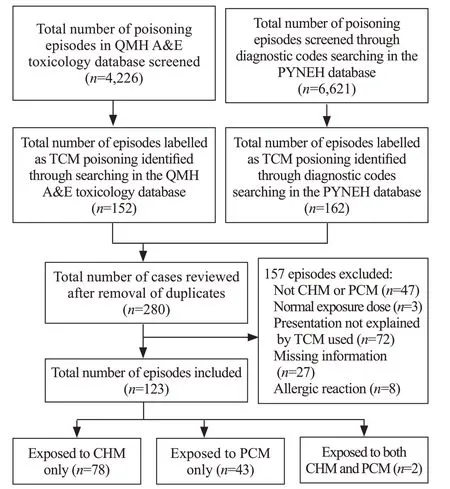
Figure 1. Flow diagram of subject recruitment. QMH: Queen Mary Hospital; PYNEH: Pamela Youde Nethersole Eastern Hospital; TCM:traditional Chinese medicine; CHM: Chinese herbal medicine; PCM:proprietary Chinese medicine.
Exposure to psoralen/isopsoralen (Fructus Psoraleae[Buguzhi]), anthraquinones (Polygoni multif lori[Heshouwu]andRhizoma rhei[Dahuang]), and a number of other herbs,includingFolium artemisiae argyi(Aiye),Fructus xanthii(Cang’erzi),Radix bupleuri(Chaihu),Radix scutellariae(Huangqin),Rhizoma dioscoreae bulbiferae(Huangyaozi),Rhizoma pinella(Banxia),Sauropus spatulifolius(Longliye) was associated with elevated liver transaminases and deranged liver function, but none required liver transplantation.
Univariate analysis revealed that a higher triage category(category 1 or 2), exposure to aconitine, exposure to methyl salicylate, earlier ED presentation after exposure, a lower triage Glasgow Coma Scale and a lower triage systolic blood pressure were signif icantly associated with a poor outcome.When all six factors were entered into the multivariable backward logistic regression model, only high triage category (OR7.33, 95%CI1.32-40.61,P=0.023), exposure to aconitine (OR27.42, 95%CI2.55-295.31,P=0.006),and exposure to methyl salicylate (OR24.17, 95%CI2.09-279.69,P=0.011) remained independent predictors of a poor outcome (Table 3).
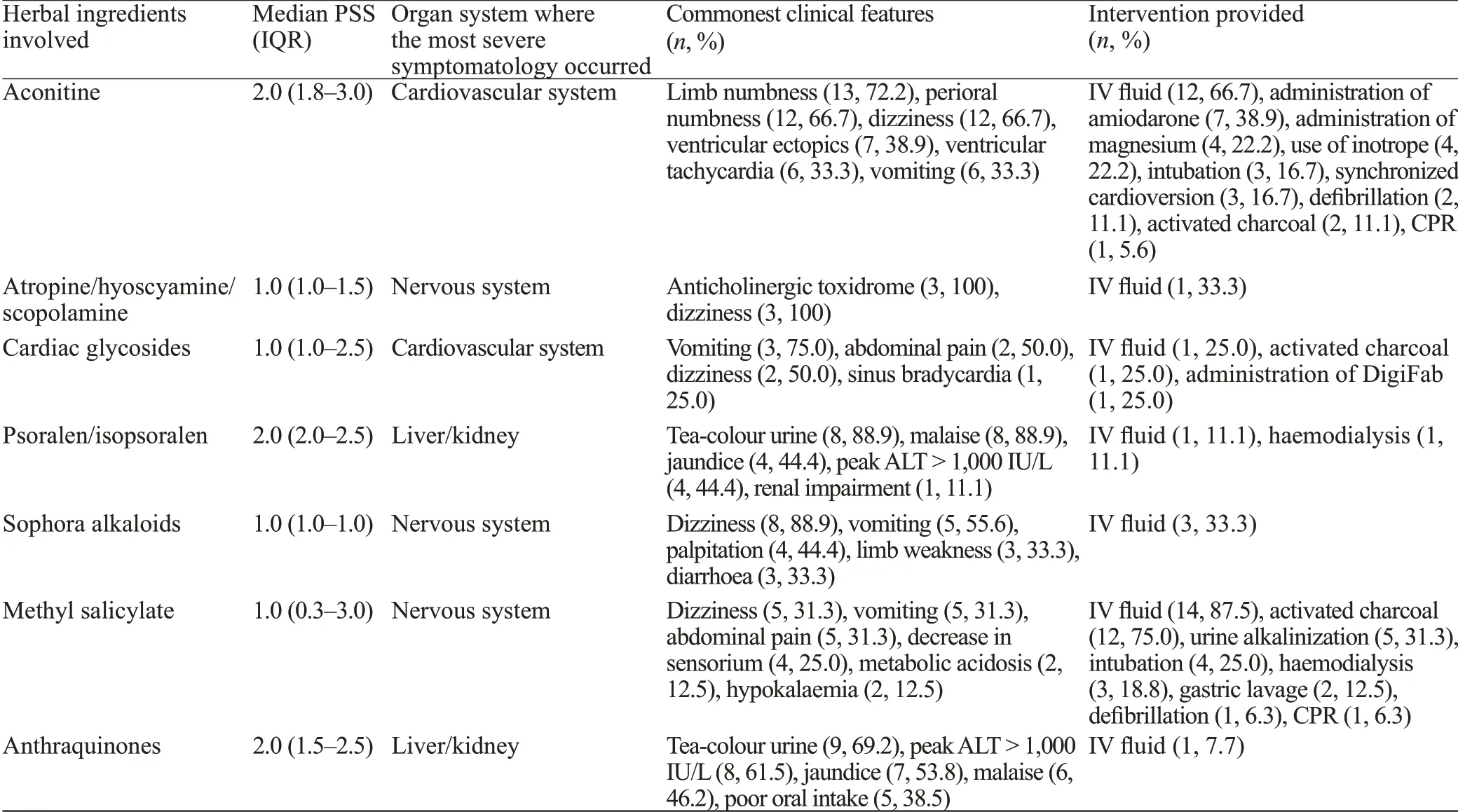
Table 2. The Poison Severity Score (PSS) and distribution of most severe symptomatology in different organ systems of ten selected toxic herbal ingredients
DISCUSSION
In this study, we characterized the overall pattern of TCM toxicity presenting to the ED using inclusion and exclusion criteria that were based on regulatory standards,clear definitions of TCM and its various forms, and validated PSS. We believe this approach provides a better understanding of the overall impact of TCM poisoning in the ED and the relative contribution of different toxic herbal ingredients, highlighting key areas of focus for emergency physicians and clinical toxicologists without training in TCM.
In the literature, there is a paucity of published data on the ED incidence of TCM toxicities. Our study found that,in high-volume Asian EDs serving a predominantly Chinese society where TCM use is common, the ED incidence of TCM toxicities has remained low throughout the past decade. Although the trend of CHM toxicities appears to be rising slightly, the overall number of TCM toxicities,as well as that of PCM toxicities, has remained low and static. The reported incidence in the current study was lower compared with a previous local study (102.4 per 100,000 ED attendance),[4]but this can be explained by the different study methodology, use of more stringent recruitment criteria, and the exclusion of allergic reactions in the current study.
Despite the low incidence, our study demonstrated that 13% of TCM poisoning cases in the ED had a poor outcome.The rarity of occurrence has led to a lack of experience in clinicians in recognizing and managing TCM poisoning.When the clinician’s native language is not Chinese,additional problems in interpreting the CHM formula and recognizing the toxic herbal ingredients will appear. Our experience indicates that the ED toxicology team model,with around-the-clock access to poison center consultation and laboratory support, helps accumulate experience in the team. As in other poisonings, the ED toxicology team can also help reduce unnecessary hospital admission and shorten patients’ length of stay without jeopardizing the quality of patient care.[16,17]Our f indings reveal that almost half of TCM poisoning cases can be managed by emergency physicians in the observation ward or emergency short-stay ward with supportive care. Indeed, less than one third of patients require hospital admission.
CHM and PCM toxicities differ in several ways in regard to presentation. The majority of CHM toxicities presented as adverse drug reactions, while almost half of PCM overdoses were intentional. Certain formulation of PCM, often in the form of medicinal oil and oral capsules/tablets, enables ingestion of a large amount in deliberate self-harm. Patients with PCM toxicities are often assigned a higher triage rating and administered activated charcoal,which could be explained by their earlier presentation and a higher rate of co-ingestion of Western medicine. However,emergency physicians should be aware that CHM is no less harmful than PCM. In our study, the median PSS of CHM toxicities was significantly higher than that of PCM poisoning, and the ED length of stay was also longer.
Our study found that a higher triage category (category 1 or 2), exposure to aconitine, and exposure to methyl salicylate are significant predictors of poor outcomes in TCM poisoning. This f inding has two implications. First, the 5-level triage system currently in use in Hong Kong, which is based on the triage nurse’s assessment of the severity of patient’s presenting condition and the stability of vital signs,[18]can identify high-risk TCM-poisoned patients for whom early intensive treatment is necessary. Second, while the management of salicylate poisoning is generally covered in most medical undergraduate curricula, it is necessary to include aconitine poisoning in formal emergency medicine and clinical toxicology training.
Aconitine and related alkaloids are potent cardiotoxins and neurotoxins found in TCM “Chuanwu”(the root tuber ofAconitum carmichaeli), “Caowu”(the root tuber ofAconitum kusnezoffii) and “Fuzi” (the lateral root tuber ofAconitum carmichaeli), which are used to treat rheumatism, arthritis, fractures, bruises, and pains.[6]Aconitine and mesaconitine bind to the receptor site 2 of the voltage-sensitive Na+channel at its open state, causing persistent activation of these channels in excitable tissues. They can trigger life-threatening arrhythmia through delayed after-depolarization and early after-depolarization.[19]Although regulations on prescription and publicity measures have reduced the incidence of aconite poisoning in the last decade,[20]our study shows that aconite poisoning remains a recurring problem in the ED. The combination of cardiovascular,neurological, and gastrointestinal toxicities observed in our study was consistent with that reported in the literature,[21,22]signifying that recognition of the presentation pattern may play a role in the early clinical diagnosis of aconite poisoning. Our observation further indicates that almost all emergency physicians followed the Advanced Cardiac Life Support pathway, including the use of amiodarone, magnesium, lignocaine, and electrical therapy, in managing ventricular dysrhythmias arising from aconite poisoning, although with mixed success. These f indings are consistent with those reported in a systematic review of the management of ventricular dysrhythmia in aconite poisoning.[23]Flecainide, charcoal hemoperfusion, and cardiopulmonary bypass were not used in our case series, and therefore we cannot comment on their effectiveness. Based on our data, we support the use of a time-buying strategy, including supportive treatment and prolonged cardiopulmonary resuscitation (in case of cardiac arrest), to allow the body to excrete the toxic alkaloids.
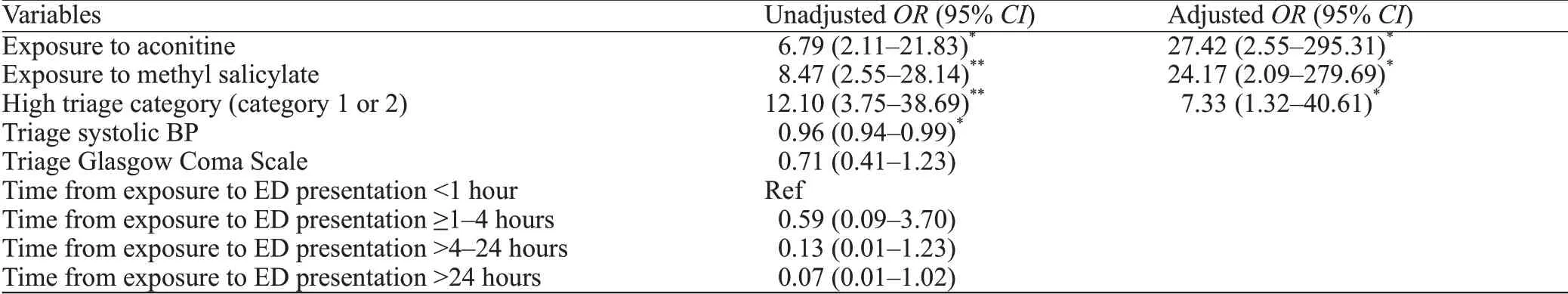
Table 3. Predictors for poor outcomes in TCM poisoning in the ED
Consistent with a previous study on PCM, we found that most PCM toxicities were mild or moderate, except for those that involve methyl salicylate.[24]Methyl salicylate is a major ingredient in numerous over-the-counter PCM in the form of medicinal oil, ointments, lotions or liniments,which are widely used to relieve musculoskeletal aches and pains.[25,26]Accidental or deliberate ingestion of methyl salicylate can result in rapid salicylate poisoning, because of its high concentration in PCM, liquid formulation, and lipid solubility. The latter increases its penetration across the blood-brain barrier and causes central nervous system toxicity. The presence of other toxic ingredients, such as camphor and turpentine, may contribute to neurological toxicities.[27,28]Our study also found that neurological toxicities were a predominant toxic feature after exposure to methyl salicylate: four patients required endotracheal intubation for airway protection. The high occurrence of vomiting (around 1/3 in our study) and decreased sensorium(1/4 in our study) call for proper airway protection when gastrointestinal decontamination is indicated.
Although not associated with a poor outcome, as defined in our study, we found that exposure to certain herbal ingredients was associated with hepatotoxicity.Herb-induced hepatotoxicity has been well reported after consumption of psoralen/isopsoralen (Fructus psoraleae[Buguzhi]), anthraquinones (Polygoni multiflori(Heshouwu) andRhizoma rhei(Dahuang),Folium artemisiae argyi(Aiye),Fructus xanthii(Cang’erzi),Radix bupleuri(Chaihu),Radix scutellariae(Huangqin),Rhizoma dioscoreae bulbiferae(Huangyaozi), andRhizoma pinella(Banxia) in the literature.[29-31]In our study, we also identified two cases of hepatotoxicity induced bySauropus Spatulifolius(Longliye), which was not reported previously within the literature.[32]In general, patients who are exposed to these herbs often exhibit elevated liver transaminase and features of deranged liver function. It is often only after the exclusion of other plausible causes that a diagnosis of herb-induced hepatotoxicity is made. Emergency physicians should actively check for exposure to hepatotoxic herbs when managing patients with unexplained deranged liver function in the ED.
Limitations
There are several limitations to this study. First, its retrospective design might lead to information bias. We sought to minimize the misclassification of cases by screening the whole QMH toxicology database for potential cases and using a broad strategy for the diagnostic code search in PYNEH. Second, the current study relied on clinical diagnoses made by the attending clinicians and critical retrospective chart reviews by the investigators.We did not involve Chinese medicine practitioners when evaluating causality. On the one hand, we might have under-reported the incidence of TCM toxicities in the ED,because of the stringent criteria and definitions used in the case selection, the lack of information in some cases, and the occurrence of misdiagnosis by attending clinicians.On the other hand, we might have over-reported the incidence, because causality was not critically reviewed by a Chinese medicine practitioner. However, we believe that this limitation reflects the real clinical situation, where the timely consultation of a Chinese medicine practitioner is not an option in most EDs. Moreover, stringent case selection criteria and definitions are important to avoid overstating the toxic effects of TCM, especially when not every case has been analytically conf irmed. Third, we were not able to explore the reason behind TCM toxicity in many cases due to incomplete documentation. We could not evaluate the impact of prescription or dispensary error, contamination,impurities, adulteration, and substitution, which are not uncommon in TCM poisoning. Thus, further studies should examine the relative contribution of these factors in instances of TCM poisoning encountered in the ED. Finally, the data of this study were obtained from two EDs in Hong Kong only. The results might not be generalizable to other EDs where the population has a different prevalence and pattern of TCM use.
CONCLUSIONS
Although TCM poisoning is a rare occurrence in the ED, a significant portion of patients develop a poor outcome. Emergency physicians should be aware of the differences between CHM and PCM poisoning and should not underestimate the consequences of an adverse drug reaction to CHM. Training that focuses on managing aconite poisoning and methyl salicylate poisoning should be offered to all emergency physicians practising in regions where TCM use is popular.
ACKNOWLEDGEMENTS
The authors would like to thank Dr. Tony Wing Lai Mak from the Hospital Authority Toxicology Reference Laboratory, as well as Dr. Man Li Tse and Mr. Tin Yat Chow from the Hong Kong Poison Information Center for reviewing the laboratory and poison center consultation records to help in the creation of this manuscript.
Funding:This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-prof it sectors.
Ethical approval:The study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (UW 16-1003) and the Research Ethics Committee of the Hospital Authority Hong Kong East Cluster(HKEC-2016-112).
Conflicts of interests:The authors have no conflicts of interest to declare.
Contributors:RPKL conceived and designed the study and developed the method. JKSL and MSHT provided study supervision.RPKL and WLY retrieved medical records, performed chart review,and collected data. RPKL and EHYL analyzed and interpreted the data. RPKL, WLY, JKSL and MSHT reviewed the literature.RPKL drafted the article. All authors contributed substantially to its revision and provided f inal approval. PRKL took the responsibility for the paper as a whole.
 World journal of emergency medicine2021年2期
World journal of emergency medicine2021年2期
- World journal of emergency medicine的其它文章
- World Journal of Emergency Medicine
- Overlapping public health crises during the coronavirus disease pandemic
- Comparison of intraosseous access and central venous catheterization in Chinese adult emergency patients: A prospective, multicenter, and randomized study
- Empyema associated with vegetable foreign body aspiration
- A red herring: An unusual case of pneumothorax
- A case of a successful post-transcatheter aortic valve replacement His bundle pacing
