Induced pluripotent stem cell technology for spinal cord injury: a promising alternative therapy
Yu Li, Ping-Ping Shen, Bin Wang
Abstract Spinal cord injury has long been a prominent challenge in the trauma repair process.Spinal cord injury is a research hotspot by virtue of its difficulty to treat and its escalating morbidity. Furthermore, spinal cord injury has a long period of disease progression and leads to complications that exert a lot of mental and economic pressure on patients.There are currently a large number of therapeutic strategies for treating spinal cord injury,which range from pharmacological and surgical methods to cell therapy and rehabilitation training. All of these strategies have positive effects in the course of spinal cord injury treatment. This review mainly discusses the problems regarding stem cell therapy for spinal cord injury, including the characteristics and action modes of all relevant cell types.Induced pluripotent stem cells, which represent a special kind of stem cell population,have gained impetus in cell therapy development because of a range of advantages.Induced pluripotent stem cells can be developed into the precursor cells of each neural cell type at the site of spinal cord injury, and have great potential for application in spinal cord injury therapy.
Key Words: axon regeneration; cell therapy; functional recovery; induced pluripotent stem cell; mesenchymal stem cell; neural cells; neural precursor cell; neural stem cell;remyelination; spinal cord injury; stem cells
Introduction
Spinal cord injury (SCI) causes severe damage because the nerves inside the lesion area are severed, meaning that signals cannot pass to the brain or spinal center, resulting in motor impairments. Worldwide, there are currently more than 27 million people living with chronic motor dysfunction following SCI; 90% are the result of traumatic injury and just 10% are the result of secondary injuries from other diseases (Bradbury and Burnside, 2019). Traumatic SCI can be classified as cervical vertebrae injury, thoracic vertebrae injury, or lumbar vertebrae injury. Of these, cervical vertebrae injuries have a death rate that is two times higher than the other two types,likely because high cervical SCIs occur near the respiratory and heart center of the medulla oblongata (Selvarajah et al., 2014). SCIs have three main causes: accidents, falling,and trauma caused by large objects. In the past, accidents were viewed as the most common cause, but a recent report concluded that falling is at the top of the list of factors that cause SCI (Selvarajah et al., 2014). SCI results in enormous damage to both families and societies. For example, in the USA, each patient with SCI costs between 1.1 and 4.6 million dollars over their lifetime (Ahuja et al., 2017). In addition,other pressures, such as the inability to stand, and urinary or fecal incontinence, are a cause of pain for these patients.All of these challenges can ultimately become physical and psychological problems for patients themselves, as well as for the entire country.
The process of SCI includes several stages: physical contusion,primary injury, secondary injury, and eventually chronic SCI with the maturity of glial scars (Tran et al., 2018). The primary injury begins with an inability to move the body autonomously. With the loss of connections between the injured spinal cord and the higher central nervous system(CNS), blood vessels below the injured plane dilate, and blood pressure drops. Because of the low blood pressure and ischemia, many cells begin to die via necrosis and apoptosis.A series of reactions, involving free radical and excitotoxic neuron generation, iron imbalance, and cell membrane lipid peroxidation, occur in the lesion microenvironment within several hours of the injury, and are accompanied by larger scale expansion of the lesion area. The secondary injury of SCI is thus primed as a more serious stage than the first one. Oligodendrocytes are a type of cell that are located in neuronal tissue, lying side by side between nerve fibers to wrap axons, form insulating myelin sheath structures, and assist the efficient transmission of bioelectrical signals. A decrease in oligodendrocytes and oligodendrocyte precursor cells (OPCs) continues for 3 weeks after SCI, and leads to the complete demyelination of neurons around lesion sites(Paschon et al., 2019). Another phenomenon that occurs in SCI is the secretion by microglia of injury signals, including DNA, RNA, and proteins, which are known as molecular patterns associated with post-traumatic injury (Paschon et al.,2019). This secretion results in the attraction of hypertrophic astrocytes, activated by the inflammatory environment, to the lesion boundary (Bradbury and Burnside, 2019). Over time,an astroglial scar slowly forms under a strong extracellular matrix chondroitin sulfate proteoglycan (CSPG) promoter. If this process progresses, it eventually forms a large functionfree cavity, which fails to communicate with the surrounding nerves and results in permanent motor dysfunction (Figure 1).
Currently, SCI remains one of the most challenging complications in the clinic. As well as routine therapeutic strategies, such as pharmacological, surgical, and rehabilitation treatments, cell-based therapies for SCI are also growing rapidly, and progressing from bench to bedside.The number of studies regarding cell therapy for SCI has increased continually from the 1980s, especially in the years after 2000, as observed when we retrieved literature through PubMed using the keywords “spinal cord injury” and“cell therapy” (Figure 2). For decades, the effects of various cell types (including different kinds of stem cells and stem cell-derived oligodendrocytes or neurons) on functional recovery in SCI have been explored. Here, we review the history, progression, limitations, challenges, and perspectives of cell-based therapies in the treatment of SCI, to provide further understanding and references for future cell-based therapeutic alternatives.
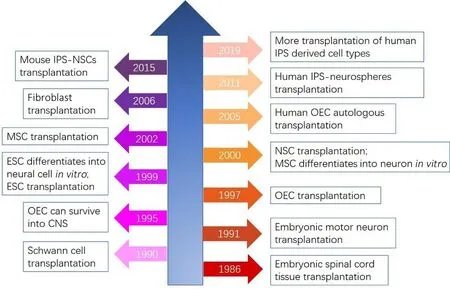
Figure 2|The development process of cell-based SCI therapies.
Search Strategy and Selection Criteria
For the “Cell types involved in SCI” section of this review,a PubMed search for papers published up to 2019 was performed with the following terms: (spinal cord injury [Text Word]) AND (traumatic [Text Word]), which returned 5179 results. For the “Development of cell therapies” section, we searched papers in PubMed using the terms (spinal cord injury[Text Word]) AND (transplantation [Text Word]), and 2510 results were displayed. We then retrieved 62 results using“clinical trial” as the search term selection for the third section of this review, “Clinical trials of cell-based SCI therapies”. For the last section, “IPS technology is a promising alternative treatment for SCI”, we reviewed the 4121 results of a PubMed search for “induced pluripotent stem cell [Title/Abstract]” up to 2019.
Cell Types Involved in SCI
Nerve rebuilding depends on sufficient support and nutrients,which are usually offered by the intracellular matrix and astrocyte-mediated nutrient uptake. The best way to promote motor function recovery requires the regeneration of both dead and damaged nerves and cells. However, neural growth factor deficiencies, myelination inhibitors, the glial scar, and the cystic cavity constitute a barrier to neural tissue selfrepair that cannot be dealt with using traditional methods(Guo et al., 2019). It is therefore believed that the creation of an appropriate environment for cell-based therapies in SCI treatment is essential to induce cell proliferation,axon sprouting, and remyelination. In cell-based therapies,specific cells are transplanted into the lesion sites, but they often struggle to survive in an unfavorable regenerative microenvironment. These exogenous cells must then accommodate themselves in the new environment and participate in the activity of the existing cells (Ahuja et al.,2017). To make transplanted cells work better, a basic step is to understand the concrete function of the cells that are involved in SCI.
Neurons
Neurons are responsible for passing information to any corner of the body by means of electric signals. This process relies on tight junctions between neurons as well as axonal integrity. In SCI, patients are unable to initiate voluntary movement below the transected section. Unfortunately, it is very difficult to repair the nervous system, especially the CNS (Bradbury and Burnside, 2019). Furthermore, nerve regeneration abilities decrease with age. Anderson et al.(2018) concluded that three factors are partially or totally responsible for the failure of neurons to regenerate in adults:neuronal intrinsic growth ability, the supportive matrix, and chemical attraction. Cooperation between these factors is an important contributor to successful neuronal regeneration.Previous studies have reported that neuronal growth requires the proper impetus; the course of neuronal growth only runs smoothly when negative factors are discarded and positive factors are involved. One group recently reported that V2a interneurons can be induced from pluripotent cells (Butts et al., 2019) and are able to alleviate neurogenic disease and function in the CNS. From this, we can conclude that lost neurons are able to be compensated for by neurons derived from endogenous or exogenous cells with stemness traits.Additionally, many other types of neurons need to be further studied for nerve growth in SCI repair. Neurons are vital for signal transmission; thus, ensuring their quantity and quality is very important.
Astrocytes
Astrocytes normally regulate neurotransmitters and neurovascular dynamics, and maintain the consecutive delivery of stable neural signals together with neurons (Gaudet and Fonken, 2018). However, their fate can be diverted toward repairing the wound after traumatic SCI. To respond to severe contusion conditions, both na?ve and active astrocytes quickly proliferate and migrate to the injury environment with the aim of filling the gap, eventually causing an astrocytic scar.This scar is a double-edged sword, making it a hot topic in SCI research. On the one hand, the astrocytic scar limits the amount of toxic factors spreading from the lesion epicenter,thus depressing inflammation expansion and secondary injury; on the other hand, the astrocytic scar shuts out axons and trophic factors, eventually contributing to the failure of damaged neurons to reconnect (Gaudet and Fonken, 2018).Recent reports agree that the advantages of the astrocytic scar are greater than the disadvantages, and suggest that it helps rather than restrains neuronal regrowth (Anderson et al., 2016). The rigid scar is surprisingly thin and is surrounded by a cluster of residual glial cells; these cells are active and can continue with nerve circuit recombination and synapse turnover, depending on their primitive structure and function(O’Shea et al., 2017). What is the role of the glial scar? It has been reported that a kind of extracellular protein deposits on the scar border when astrocytes start to assemble. This protein is CSPG (also known as neuron glial antigen 2; or NG2).CSPG is a nerve growth inhibitor that accumulates on the first day after traumatic SCI and remains there indefinitely (Gaudet and Fonken, 2018). In SCI treatments, it might therefore be useful to target CSPG rather than try to remove the protective glial scar. To do this, we need to understand the mechanisms of CSPG formation and prohibit its initiation (Tran et al.,2018). Interestingly, glial scars may be reversible, because reactive astrocytes in SCI revert to a na?ve state after being transplanted to a healthy spine (Hara et al., 2017). That is, the role of astrocytes is reflected in glial scar formation during the wound healing process. We can therefore conclude that in future research, researchers will move away from trying to remove the glial scar or reactive astrocytes, and instead investigate how to make the scar border more penetrable for surrounding cells or extracellular matrix proteins.
Oligodendrocytes and OPCs
An intact neuron cannot function without the myelination of its axons by oligodendrocytes in the CNS and by Schwann cells in the peripheral nervous system (PNS). In the CNS,each oligodendrocyte produces up to 50 myelin sheaths that wrap axons so that neurons can be separated to promote fast action potential propagation. In contrast, in the PNS,each Schwann cell produces just one myelin sheath (Fu et al., 2019). The existence of the myelin sheath is critical for the fluent execution of function. Olfactory ensheathing cells(OECs) are functionally a mix between oligodendrocytes and Schwann cells; they have myelinating and neurotrophic functions, and play an opposite role to astrocytes by inhibiting glial scar formation. Furthermore, OECs are one of the rare renewable cell types in the CNS, and offer an appropriate environment for axon generation and migration, gradually becoming grafted cells for neural regrowth. Oligodendrocytes are the offspring of OPCs; if the former dies when encountering acute SCI, the latter tends to swiftly proliferate to compensate for the marked loss of oligodendrocytes. It is estimated that oligodendrocyte death continues from 15 minutes to 3 weeks after acute SCI, with a toll of up to 93%compared with 50% of OPCs (Gaudet and Fonken, 2018). In addition, damaged oligodendrocytes release large amounts of myelin growth antagonists, such as Nogo, tenascin, myelinbased glycoprotein, and oligodendrocyte-myelin glycoprotein(Willerth and Sakiyama-Elbert, 2008), which pose another obstacle for nervous system self-repair. At the time of secondary injury, the use of 4,4′-diisothiocyanatostilbene-2,2′-disulfonic acid, a pharmacological blocker of voltagedependent anion-selective channel 1 oligomerization, can decrease the oligodendrocyte death rate and lesion size, and increase neuron density and motor function recovery (Paschon et al., 2019). Many researchers have noted that OPCs that are latent in the glial scar border have a potential correlation with CSPG; these OPCs express CSPG protein on the cell surface and are named OPC-CSPGs. The remyelination ability of OPCs is weakened as a result of CSPG attachment (Tran et al., 2018). In the PNS, Schwann cells, with similar abilities to oligodendrocytes, may be useful in SCI treatment. Although their migration capability is limited and they fail to integrate with host astrocytes when transplanted into the body, these limitations can be resolved by the magnetic modification of Schwann cells (Huang et al., 2017). Thus, oligodendrocytes,OPCs, and Schwann cells maintain spinal myelination at all times and help with remyelination after axonal injury. For cell therapies, all three cell types may be appropriate for grafting.
Microglia
In the nervous system, microglia are a family of cells characterized as macrophages in the immune system.These cells normally patrol the nervous system scanning for infections and lesions, and act as guardians of immunity.After SCI, they can foster nerve rebirth; however, they can also become overactivated, leading to cytotoxicity (Gaudet and Fonken, 2018). Spinal lesions lead to blood-spinal imperfections, macrophages and inflammatory molecules receive signs of the aforementioned extracellular injuryassociated molecular patterns, and a sequence of intricate reactions then arises. However, we cannot overlook these invasive macrophages, because they are key members of the innate immune system. Taking advantage of internal signaling pathways, they can alter microglia and astrocytes, and lead to further alterations of neuroinflammation in traumatic SCI and some neurodegenerative diseases (e.g., Alzheimer’s disease)(Andreasson et al., 2016). In addition, there is a balance between macrophage subtypes that is disrupted by SCI; SCI affects macrophage excitation, spurring a pro-inflammation class switch that potentiates a prolonged inflammation response (Gensel and Zhang, 2015). The immune response is accelerated by morphological and proteomic alterations of microglia under mutual impacts with astrocytes, which also fosters the secretion of inflammatory factors (Paschon et al.,2019). Hence, a cellular network exists in SCI recovery, and each cell type has a unique identity and cannot be replaced by any other. If we want to treat SCI using cell transplantation,we therefore need to understand the interactions among all neural cells, rather than just eliminating or enriching one cell group.
Development of Cell Therapies
We have summarized some animal trials that have tried cell transplantation for SCI therapy (Table 1). Graft candidates have been tested using diverse cell introduction methods, includingin situinjection, intranasal delivery, and cerebrospinal fluid transmission (Satake et al., 2004; Guo et al., 2019), through which implanted cells can survive and transfer to the injured site to execute their functions. In the mouse, rat, dog, pig, and monkey, cell transplantation has been reported to provide a favorable environment for neurogenesis and functional recovery. Current methods used to track progress after cell transplantation include survival time, differentiation ability,expression of neural markers, axon remyelination, neuronal regeneration, and an increase in locomotive Basso-Beattie-Bresnahan scores. In future research, newer and more convincing criteria need to be adopted to provide more precise and reliable information for SCI patients. Next, we summarize the characteristics and action modes of all cell types appropriate for SCI repair.
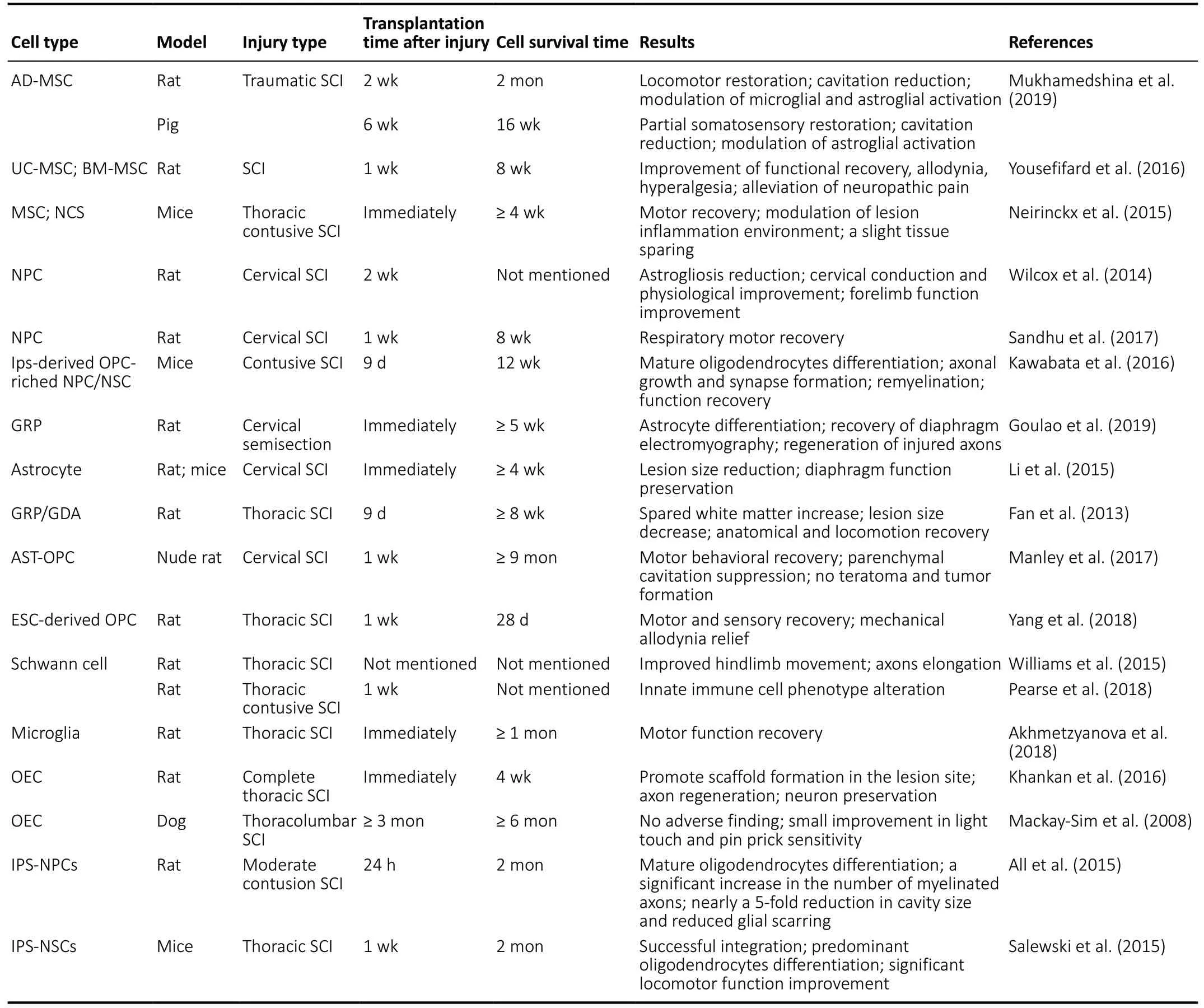
Table 1 |Cell types tested in animal SCI models
Fetal spinal cord tissue
Unlike most cancers, SCI may be not lethal, but it can cause chronic, severe physical disability. At first, routine therapy was the major focus—the idea of transplantation treatment did not appear until scientists became aware of the need to repair the injured nervous system. In 1986, mouse fetal spinal cord tissue was first used as a graft object to transplant into an injured mouse for functional observations (Reier et al.,1986), and a good recovery outcome was achieved. Thus,replacing one damaged tissue with a similar intact counterpart appeared to be a good idea. Subsequently, scientists again implanted embryonic spinal cords into both newborn and adult SCI models. The recovery outcomes indicated that spinal cord transplantation indeed ameliorated lesioninduced functional deficits and decreased the severity of hindquarter lesions (Bregman et al., 1993). However, although the recovery effects of this treatment are clear, it requires fetal spinal cord tissue extraction, which is unfeasible due to ethical considerations and limited source. Nevertheless, based on these ground-breaking transplantation results, cell-based transplantation research began to arise for the treatment of SCI.
Schwann cells and neurons
The ability of Schwann cells to myelinate neurons in the PNS drew attention to their possible use in implantation for SCI repair. Kuhlengel et al. (1990) injected Schwann cells from the PNS into the lesion site of spinal cord models and reported that these surviving Schwann cells packaged neuronal axons and could form basilar membranes. This study demonstrates that Schwann cells can also play an axon ensheathing role in the CNS. Research supporting this conclusion was published the following year by Paino and Bunge (1991). In the same year, embryonic motor neurons were reported to successfully survive and migrate into the host ventral horn to replace depleted neurons (Clowry et al., 1991). These results also indicate that co-transplantation of neurons and Schwann cells afterin vitroculturing may improve the performance of Schwann cells. However, the source of these cells is rather limited, because they are highly differentiated and can only be induced from stem cells. Hence, more stem cells with the ability to form functional cells need to be exploited.
Olfactory ensheathing cells
OECs are currently popular in cell transplantation because of their links with nerve cells. For example, they promote neurite growth without visible graft-related complications (Ahuja et al.,2017). Research relating to SCI treatment using OECs began in 1995, when Doucette recognized that OECs expressed many phenotypic features resembling astrocytes and Schwann cells.In addition, OECs survived to facilitate axonal growth after spinal cord implantation, thus demonstrating the promising therapeutic potential of OECs (Doucette, 1995). In support of this idea, OECs were reported to regenerate the inactive rat tail accompanied by the growth of lesioned axons after being introduced to an acute SCI section (Li et al., 1997).Furthermore, the use of biological tracer technology revealed that OECs with delayed transplantation, at 8 weeks post injury,settled and induced cortical axon regeneration and traveled approximately 10 mm, crossing the transplant bridge (Feron et al., 2005). Therefore, for migration and proliferation,OECs transplanted at both acute and chronic time points can promote neuronal and axonal regrowth. This indicates a relatively large time window for cell implantation, and dispels any misgivings that the acute phase is too transient for cell preparation.
Embryonic stem cells
Embryonic stem cells (ESCs) are popular in the regenerative medicine community for their properties of self-renewal,rapid proliferation, and multi-differentiation. The tendency of OECs to differentiate into nervous system cells was confirmed as early as 1999, with the discovery of oligodendrocyte and astrocyte precursors in OEC medium (Brustle et al.,1999). These precursor cells had successful intercellular communication and could myelinate neurons, which initiated research into ESC transplantation for SCI treatment. The first project appraising the functional recovery promotion of ESCs was performed by McDonald et al. (1999), who reported oligodendrocyte formation at the site of the ESC graft. Nevertheless, ESC grafts will not achieve clinical use until their latent oncogenesis can be completely eliminated.One way to overcome this barrier may be to guide ESCs toward oligodendrocyte or oligosphere formationin vitro,because these pre-differentiated cell types show identical myelin regeneration functions to ESCs when implanted into the lesion site (Liu et al., 2000). Trials in mice indicated that,when implanted at ~10 days after SCI, ESCs could differentiate into astrocytes, oligodendrocytes, and neurons over several weeks, and improved locomotor scores during migration away from the injection site. However, these consequences did not occur if transplantation was delayed up to 10 months after SCI (Keirstead et al., 2005). Therefore, although cell grafts can be performed in both the acute and chronic phases,recovery outcomes remain time-dependent. Furthermore, the appearance of factor-secreting ESCs can markedly improve therapeutic effects. They offer a variety of neural growth and trophic factors, chemokines, and specific proteins to assist the robust growth of neural cells (Chen et al., 2005).Importantly, human-derived ESCs have been demonstrated to be safe (Shroff and Barthakur, 2015), and are effective in the adult SCI rat. For human-derived ESC implantation, the successful differentiation and enhancement of locomotor performance, combined with a lack of toxicity, neurodynia,tumors, or other adverse observations, supports the initiation of phase I complete SCI clinical trials (Manley et al., 2017).Nonetheless, the source of human-derived ESCs is confined to newly formed embryos aborted by pregnant women, and animals must be killed to extract embryos for animal-derived ESCs. These cell acquisition methods have important ethical considerations, meaning that it is difficult for ESCs to be used clinically for human application.
Neural stem and precursor cells
Neural precursor cells (NPCs) and neural stem cells (NSCs)are currently the two cells with the most potential for SCI therapy because they can differentiate into all cell types in the nervous system, including astrocytes, oligodendrocytes,and OPCs. This intrinsic neural lineage differentiation trait makes them potential candidates for CNS cell transplantation.It was commonly believed that NSCs are a cell type that cannot be regenerated and that their number gradually decreases with age in the CNS; this contributed to the traditional idea of exogenous graft targeting for neural regeneration after CNS injury. However, Johansson et al.(1999) reported that endogenous ependymal cells, which were later demonstrated to be NPCs, could foster axon regeneration by self-proliferation and nestin expression.Remarkably, this phenomenon only appears after SCI, and is not present under normal conditions (Namiki and Tator,1999). This discovery resulted in the idea of NSC and NPC transplantation. During implanted NSC differentiationin vivo,these cells mainly become astrocytes (in contrast to rare neurons and oligodendrocytes) after survival, which may be an adverse reaction in the case of axon regeneration (Vroemen et al., 2003). This tendency was able to be reversed by the use of valproic acid, a histone deacetylase inhibitor, so that the differentiation balance was inclined to neurons rather than astrocytes (Zhu et al., 2018). Moreover, other methods can be used in combination to enhance the functional efficiency. For instance, NPCs co-grafted with fibroblasts lead to significantly enhanced functional outcomes, because fibroblasts provide a mesenchymal platform for cystic cavity restoration and NPC adhesion and differentiation (Pfeifer et al., 2004). Moreover,Suzuki et al. (2017) reported that 1 week of chondroitinase ABC administration contributed to marked improvements in grafted NPC survival and differentiation. To rule out the tumorigenesis potential of NSCs and NPCs, they are generally transplanted into immunodeficient animals for long-term observation. In most contused cervical or lumbar animal spinal cords, grafted NSCs/NPCs can survive for 2–8 months or more without tumor detection, and differentiate into three cell lines (astrocytes, oligodendrocytes, and neurons), reduce cell apoptosis, and increase function as measured by the Basso-Beattie-Bresnahan score (Jin et al., 2016; Sankavaram et al., 2019; Zhao et al., 2019). Some human NPCs/NSCs have also been used in rat, pig, and monkey SCI models in preclinical trials. These produced neural-specific markers and improved locomotion, indicating that clinical trials should be conducted (Rosenzweig et al., 2018; Kutikov et al., 2019).The infiltration of numerous inflammatory factors, oxidative products, pro-apoptotic factors, and many other hostile surrounding elements all contribute to acute transplantation being ineffective, while a longer time in the chronic state leads to an amplified cystic cavity and glial scar, so a 9-day delayed operation appears to be the most appropriate (Okano,2002). Before investigating further therapeutic improvements and possible human applications, efforts must be made to elaborate the underlying mechanisms of NSC/NPC activation,sustainability, and subsequent mitosis, migration, and maturation.
Mesenchymal stem cells
Mesenchymal stem cells (MSCs) have a reputation for versatility and have been successful in recent cell research.Moreover, they have exhibited many benefits in clinical application. Their immune modulation properties have been used to alleviate immunological rejection and simultaneously regulate the immune microenvironment, and their multiple lineage potencies have been used to induce many kinds of cells for cancer therapy (Podesta et al., 2019). MSCs have also received much scientific attention for their reported antiinflammation/apoptosis and cytokine-releasing behaviors in the injured spinal cord. In 2000, adult rat-/human-derived MSCs were found to express nestin and tropomyosin receptor kinase A and present neuron-like phenotypes during more than 20 passagesin vitro(Woodbury et al., 2000). This finding indicates that MSCs can break germ layer commitment to develop a neural cell fate. In accordance with this idea,in the same year, researchers transplanted MSCs into the CNS to treat middle cerebral artery occlusion and reported positive results (Chen et al., 2000). Together, these findings suggest that MSCs are promising cell candidates for SCI transplantation therapy. Unlike many other stem cell types,they have extensive sources, such as bone marrow, umbilical cord, and adipose tissue. Moreover, their acquisition methods are also simple and ethical and the culture process is easy.Experiments using rat SCI models have indicated that MSCs can display weak NeuN immunoreactivity at 5 weeks, and can also establish a nerve fiber-permeable bridge across debris, which possibly occurs via a cue from the internal lesion microenvironment (Hofstetter et al., 2002). However,MSCs do not appear to transdifferentiate into true neural cellsin vivo, although they can migrate to the spinal cord and survive for a long time (Castro et al., 2002; Jendelova et al.,2004). In contrast, when MSCs are cultured in medium and cAMP is added, they are easily diverted to become neural cell progenitors (Deng et al., 2001). In brief, the aim for MSC transplantation is not only to induce them to become functional neural cells, but also to take advantage of their role in environment modulation to promote axonal growth, secrete chemokines and growth factors, and suppress the adverse impacts of inflammation (Parr et al., 2007). Furthermore,MSCs are a self-derived and immune rejection-preventable implantation choice. MSCs are also advantageous in that they evade ethical and moral issues, and are able to overcome the difficult cellular access problems of the previously listed stem cell types. They also avoid the lineage limitation problems of terminally differentiated cells. A recent study reported that MSC-derived exosomes can freely penetrate the blood-brain barrier equipped with phosphatase and tensin homolog (PTEN)small interfering RNA (siRNA) to silence PTEN, an intrinsic inhibitor of axonal growth (Guo et al., 2019). MSCs may be able to cure complete SCI, relying on a neurite sprouting phenomenonin vitroand a functional recovery phenomenonin vivo. The proper graft time is also important with regards to the beneficial conditions for implanted cells in the later SCI period—after inflammation, oxidative reactions, and the release of lyases (Hofstetter et al., 2002).
Other cell types
Preclinical trials of cell therapies using astrocytes and microglia are scarce; they are often used as co-grafting objects to protect cells and proteins associated with axon myelination and growth, provide neurotrophic factors and molecules for tissue repair, and modulate the immune environment (Nicaise et al., 2015). Hematopoietic stem cells are a kind of stem cell that differs from the neural lineage. However, in spite of this discrepancy, hematopoietic stem cells can still divert to neural cells and foster functional recovery after being transplanted into SCI mice (Koshizuka et al., 2004). Although research into this method is rare, it is indeed an interesting phenomenon, and further suggests that we need to explore the mechanisms involved in grafted cell behaviors in the injured host. Moreover, fibroblasts as mesenchymal cells can play an indispensable role in SCI treatment if they undergo gene modification. Pizzi and Crowe (2006) reported that matrix metalloproteinase-3-overexpressing fibroblasts might degrade extracellular CSPGs to help with neuron junctions,but this function depends on their co-transplantation with neural cells, because fibroblast-only transplantation is ineffective. Many studies have been conducted using genetically engineered cell options. Genetically altered cells can excrete large quantities of neurotrophic factors, such as neurotrophin 3, nerve growth factor, basic fibroblast growth factor, brain-derived neurotrophic factor, and myelin gene regulator factor, which have benefits for myelination, axon regeneration, and the recovery of locomotor function (Grill et al., 1997; Pizzi and Crowe, 2006). These findings indicate that simultaneous implantation might be a promising option, given that one cell type can supply a growth platform and sufficient nutrients for another cell type (Willerth and Sakiyama-Elbert,2008). Cooperation between two different lineage cells may therefore create good therapeutic outcomes. However,there are a large number of harmful features opposed to normal axon elongation, neuron self-repair, and neural network shaping between implanted cells and local neurons.Therefore, in forthcoming studies, proper cell candidates,antagonists of axonal growth inhibitors, and other related strategies are expected to be discussed. For example, the use of antibodies and gene knockouts are promising means of removing undesired elements.
Clinical Trials of Cell-Based Spinal Cord Injury Therapies
A recent review has summarized recent clinical trials of stem cell-based therapies for SCI patients (Silvestro et al., 2020),and concluded that NSCs and MSCs have been the main focus and have yielded relatively satisfactory results. Here, we have also summarized several clinical trials for each possible cell type that is involved in clinical trials (Table 2). The first instance of treating SCI patients with human ESC implantation,after other therapies had been trialed, was performed in 2016 (Shroff, 2016). Despite the favorable outcomes, reported safety, advantages of rapid proliferation, and convenient genetic manipulation and induction, transforming ESCs for universal clinical application remains a huge ethical and moral challenge. Both autologous and exogenous MSC grafts have been performed in various kinds of human SCI patients, and have been traced for at least 6 months to confirm that there are no transplantation-related adverse effects. The involved female or male human receptors led to different effects on sensitivity, neurogenic bowel/bladder dysfunction, or sexual damage (Vaquero et al., 2016, 2018a, b). However, limited therapeutic consequences were reported in a phase III clinical trial, in which only 2 of the 16 patients had obvious neurological status improvement without any uncomfortable feelings about transplantation (Oh et al., 2016). In contrast,other positive trials were sufficient to suggest the safety,feasibility, and practicability of MSC implantation in the human spinal cord. In 2008, Erik Curtis reported the first instance of spinal cord-derived autologous NSC treatment, in which two of the four patients with T2–12 SCI displayed one to two levels of neurological improvement without any adverse events after 1.5–2.5 years (Curtis et al., 2018). Interestingly,the implanted autologous hematopoietic stem cells and Schwann cells all survived and infused into the injured tissue.Hematopoietic stem cells affect motor evoked potentials or somatosensory evoked potentials, whereas Schwann cells improve slight neuropathic pain or muscle spasticity (Frolov and Bryukhovetskiy, 2012; Anderson et al., 2017). Previous studies have demonstrated that there are no or very few side effects of human cell transplantation, and cell therapy to treat SCI is very feasible. In future clinical trials, further adverse effects and more safety data are expected to be reported.Simultaneously, the development of optimal personalized injections will need to cover cell dosage, delivery methods,injection times, and auxiliary medicine according to each patient’s condition. Thus, understanding the latent restorative mechanisms of diverse cell therapies is of critical significance.
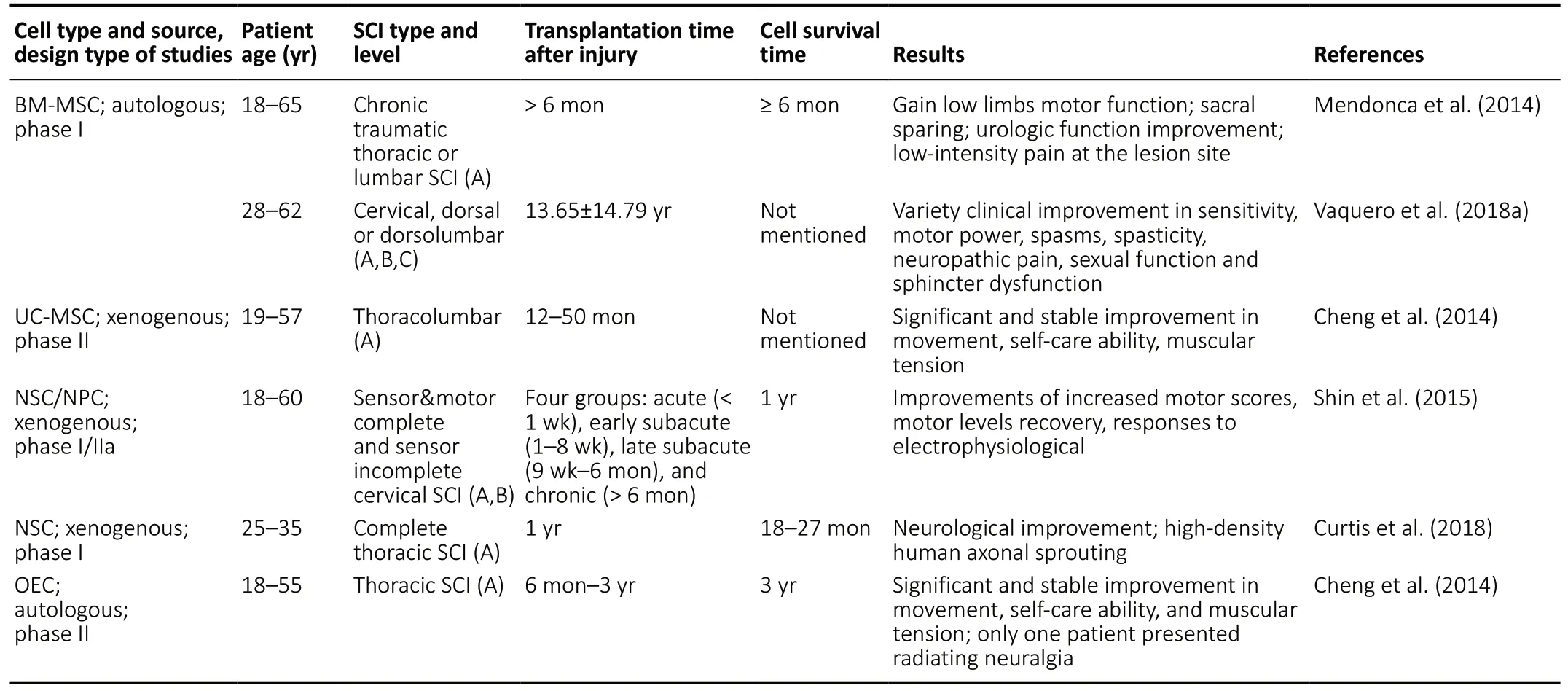
Table 2|Cell types applied in SCI clinic trials
Induced Pluripotent Stem Cell Technology Is a Promising Alternative Treatment for Spinal Cord Injury
Induced pluripotent stem cell (IPS) technology, also called cell reprogramming, came about through the efforts of Shinya Yamanaka in 2006 and John B. Gurdon in 1962 (Gurdon, 1962;Takahashi and Yamanaka, 2006). Both of their contributions suggest that mature cells can be reprogrammed to become pluripotent. As its name implies, IPS technology aims to alter cell fate and is of great historical significance, setting a milestone in both biological and medical fields. With IPS technology, cell therapy gained new hope. The reprogramming system of IPS can be developed using retroviral vectors, Sendai virus, episomal DNA, or chemical reprogramming. Chemical reprogramming has recently captured attention because it boasts a range of the laudable characteristics of chemical molecules: it penetrates well and is immunogenicity-free,adjustable, economical, easy to synthesize and conserve, and reversible (Hou et al., 2013). More importantly, it generates a non-carcinogenic XEN-like (extraembryonic endodermlike) cell state that expands rapidlyin vitrowithout destroying genomic integrity or stability (Li et al., 2017). Regardless of the path that is used for reprogramming, the rationale of cell reprogramming may be 1) the double alteration of gene expression procedures for one somatic cell (Li et al., 2017);and 2) that differentiated cells are in a temporary stable situation that is overturned once homeostasis is destroyed in the case of injury, disorders, or natural aging (Obokata et al., 2014). Until now, IPS has been used to successfully treat SCI, diabetes, sickle cell anemia, Parkinson’s disease, and thrombocytopenia in rodent disease models, and retinal pigment epithelium, leukemia, thrombocytopenia, and transmissible melanoma in human patients. IPS technology is currently evolving and may be used for a human SCI treatment protocol in the near future.
Although pre-existing cell therapies targeting chronic SCI have achieved various positive outcomes, they are unsatisfactory because many questions remain about source restriction,individual incompatibility, short survival times, and failure to integrate into the host nervous system, among others. With the emergence and maturation of IPS technology and its human application, many of these challenges have been overcome.The differentiation potential of IPSs means that they enjoy popularity in the medical field, because they can grow into any kind of functional cells according to patient needs. In parallel,IPSs bypass the ethical controversies associated with ESCs and nuclear transplantation, and avoid immune rejection problems because of their autonomous derivation from each patient’s own somatic cells. By using IPS technology to treat SCI, we may be able to rebuild the self-repair functions of absent cells in the nerve system via homologous cell reprogramming and differentiation. Moreover, the chronic development process of SCI and the long preparation required for IPS treatments are a good match. Autologous IPS-derived cells are able to escape from the host immune system and survive for a long time, meaning that they can play stable roles in the nervous system. The first instance of SCI therapy with human IPSs was performed in a mouse model, in 2011. The grafted hIPSderived neurospheres survived, migrated, communicated with host neurons, and differentiated into astrocytes/oligodendrocytes/neurons for up to 112 days. They also presented outcomes of angiogenesis and neurite growth, and increased myelination and motor function recovery without tumorigenesis (Nori et al., 2011), which suggests the feasibility of applying IPSs to treat human SCI. Thus, to treat a patient with SCI, we can obtain somatic cells from every convenient tissue of the patient, induce them to IPSs via the Oct3/4, Sox2,Klf4, and c-Myc (OSKM) method or chemical reprogramming,and differentiate them into neural-specific cells to participate in spinal cord repair (Figure 3).
There are several limitations of IPSs for clinical application,such as a high risk of tumor germination and a low induction efficiency because of residual somatic cell epigenetic memory(Shi et al., 2017; Keefe and Li, 2020; Mao et al., 2020).Fortunately, the tumor formation limitation can be resolved using γ-secretase inhibitor, quality checks, pre-differentiation,and suicide gene introduction (Fatima et al., 2019; Nagoshi et al., 2019). A recommended solution for the low induction efficiency involves stepping away from current autologous grafts toward allografts, which rely on the formation of a cell bank. A cell bank was accomplished for the first time by Taylor et al. (2012), on the basis of major histocompatibility complex(MHC) matching between the receiver and exogenous stem cells. This idea involves extracting disease-free somatic cells for IPS generation and storing them in a cell bank, without losing stemness, for future direct use. Thus, the establishment of an IPS-derived cell bank underlies an IPS-derived NSC/NPC bank, which is expected to provide possibilities for immediate use and increase success rates of recovery (Okano and Yamanaka, 2014). In this way, we would be able to use IPSs from the same origin in a large number of patients with SCI, thus boosting IPS efficiency. Nevertheless, optimal transplantation times; differences between experimental and clinical stem cells caused by culture conditions, donor standards, and receptor types; and cell action modes should be taken into consideration (Takahashi, 2018).
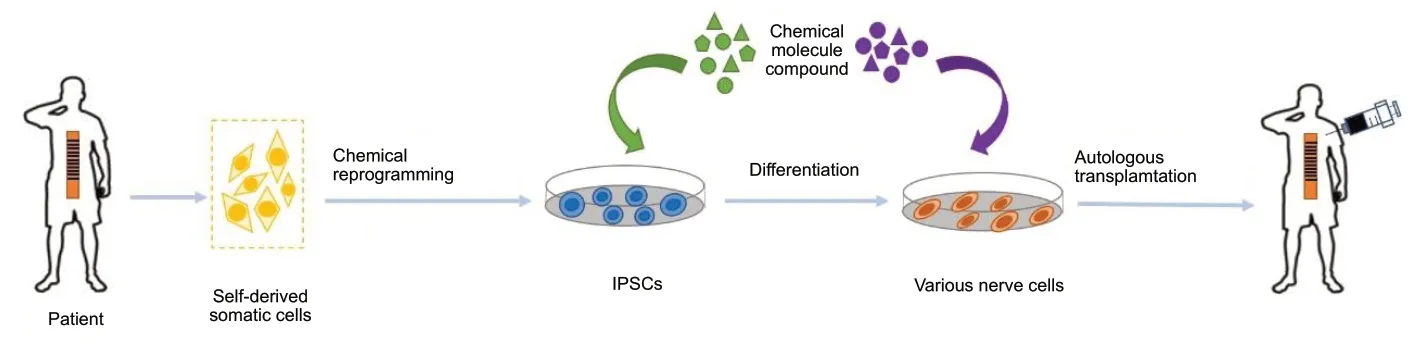
Figure 3|Application of IPS technology for SCI therapy using autologous somatic cells.
Conclusions and Perspectives
SCI is an increasingly intractable problem worldwide.Given that many difficulties remain to be resolved with cell therapies, we believe that IPS technology should be used as an SCI therapy. Based on previous animal results, the further human introduction of IPS, and all phases of clinical tests being passed, the preclinical data needs to be summarized to create a safe and efficient protocol. The use of both biological scaffolds and physical training is likely to improve functional outcomes accompanied by the establishment of innervation networks, and more than 10 times the number of anti-inflammatory cells have been reported in treatment group compared with the control group (Lin et al., 2019).The combined transplantation of easily degradable biological scaffolds and stem cells may enhance the effects of therapies as a result of more appropriate growth environments. In the future, a more comprehensive therapy should be created,because neither traditional therapies nor IPS-derived cell implantation can individually lead to functional recovery.Current medical developments involve selecting the most suitable cell type for transplantation in accordance with each patient’s injury degree and site, and formulating a patientspecific therapeutic schedule. Additionally, patient mindset is of critical importance; if a good treatment effect is desired,frequent psychological counseling is essential. A cure for SCI is expected in the near future using cell therapies and IPS technology.
Author contributions:Literature searching and manuscript writing: YL;manuscript revision: BW and PPS; manuscript guidance: BW. All authors read and approved the final manuscript.
Conflicts of interest:The authors declare that they have no competing interests.
Financial support:This project was supported by the National Key Research and Development Program of China, No. 2017YFA0104304(to BW), 2017YFA0205400 (to PPS), and 2017YFA0506000 (to PPS); the National Natural Science Foundation of China, No. 81571213 (to BW);the Nanjing Medical Science and Technique Development Foundation of China, No. QRX17006 (to BW); the Nanjing Medical Science and Innovation Platform, No. ZDX16005 (to BW) and the Innovation and Entrepreneurship Plan of Jiangsu Province (2019) (to BW).
Copyright license agreement:The Copyright License Agreement has been signed by all authors before publication.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix,tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Open peer reviewer:Melanie G. Urbanchek, University of Michigan, USA.
Additional file:Open peer review report 1.
 中國(guó)神經(jīng)再生研究(英文版)2021年8期
中國(guó)神經(jīng)再生研究(英文版)2021年8期
- 中國(guó)神經(jīng)再生研究(英文版)的其它文章
- Peri-infarct reorganization of an injured corticospinal tract in a patient with cerebral infarction
- Non-invasive electrical stimulation as a potential treatment for retinal degenerative diseases
- TLR2 and TLR4-mediated inflammation in Alzheimer’s disease:self-defense or sabotage?
- Stem cell-derived three-dimensional(organoid) models of Alzheimer’s disease: a precision medicine approach
- Microglia accumulation and activation after subarachnoid hemorrhage
- Histone acetylation and deacetylation in ischemic stroke
