Multimodality imaging in COVID-19 patients: A key role from diagnosis to prognosis
Antonello D'Andrea, Juri Radmilovic, Andreina Carbone, Alberto Forni, Ercole Tagliamonte, Lucia Riegler,Biagio Liccardo, Fabio Crescibene, Cesare Sirignano, Giovanna Esposito, Eduardo Bossone
Abstract
Key Words: COVID-19; Interstitial pneumonia; Pulmonary computed tomography;Echocardiography; Lung ultrasound; Thromboembolism
INTRODUCTION
On December 31, 2019, the World Health Organization was alerted by the Public Health Commission of the Province of Hubei, China regarding some cases of severe pneumonia, of unknown etiology, characterized by symptoms such as fever, malaise,dry cough, dyspnea and respiratory failure, which occurred in the urban area of Wuhan. A new coronavirus, severe acute respiratory syndrome coronavirus 2, was identified as responsible for the lung infection and is now called coronavirus disease 2019 (COVID-19). Since then, as we well know, there has been an exponential growth of contagions, which initially involved neighboring countries, such as Japan and South Korea, and then affected extra-continental countries, with the first documented cases in Europe, United States and Africa between January and February 2020. On January 30, 2020, the World Health Organization declared the epidemic a global emergency.The epidemic exploded in Italy on February 21, 2020, while the pandemic was declared on March 10, 2020. Currently, the main sources of infection are people themselves infected with severe acute respiratory syndrome coronavirus 2. Even asymptomatic carriers can become a source of diffusion. Transmission takes place by aerosol via “droplets”, but even if direct and indirect transmissions are less important,they must be taken into account. An early diagnosis of the virus carriers is one of the key points to contain the spread, the morbidity and the mortality of the pandemic. The definitive diagnosis takes place through specific tests, while the exact role of imaging in the care pathway of the patient with suspected or confirmed COVID infection is still to be defined.
The subject of this review is to underline precisely the role of imaging in the evaluation of these patients.
CLINICAL MANIFESTATIONS
According to current epidemiological investigations, the incubation lasts from 1 to 14 d, usually from 3 to 7 d. The clinical manifestations are very heterogeneous, and the main ones are fever, dry cough and asthenia. In a minority of patients, nasal obstruction, rhinorrhea, pharyngodynia, myalgia and diarrhea are present. Common neurological symptoms include anosmia and dysgeusia and mental confusion in marked hypoxemia. Dyspnea and/or hypoxemia occur in patients with a severe form of the disease often 1 wk after the onset of the disease, while rapid progression to acute respiratory distress syndrome (ARDS), septic shock, metabolic acidosis, coagulation deficiency and finally multiple organ failure are possible in critically/very serious patients. Some children and infants may instead present an atypical clinical profile,which consists of gastrointestinal symptoms, such as vomiting, diarrhea, drowsiness or hypersomnia and tachypnea.
Of interest, as underlined by numerous position papers of national and international scientific societies, coronavirus infection can have implications in the cardiological field for the following reasons: Patients with COVID-19 infection can develop cardiac complications, although not very frequent; cardiovascular diseases continue to be predominant in the general population and the same patients who present with an acute coronary syndrome can at the same time be infected or carriers of COVID-19. Reverse transcription-polymerase chain reaction and/or next generation sequencing can detect the presence of viral nucleic acids in oro-pharyngeal swabs, sputum and other samples from the lower respiratory tract, blood and stool.The samples of choice for greater accuracy of the test are those from the lower respiratory tract (sputum or bronchoaveolar lavage). Once the sample is collected, it should be analyzed as soon as possible. It represents the gold standard for diagnosis;but, being burdened by numerous false negatives in the initial stages of the disease, it must be repeated in suspicious cases at 72 h to confirm the absence of disease.
IMAGING TECHNIQUES
In a context of non-specific symptoms and extremely variable clinical pictures, such as severity and progression, the contribution of integrated imaging can be crucial not only for the diagnosis of pneumonia but also for therapy monitoring and obtaining prognostic information.
Currently, the optimal imaging strategy is still uncertain. The discriminating parameter to hospitalize or send home a patient with suspected COVID-19 is the presence of respiratory failure, linked to the pulmonary infection that may be in progress (respiratory failure, even subclinical, given the progressively rapid worsening of the pathology). The functional data can be easily obtained by performing a blood gas analysis (a simple, rapid procedure that does not require patient access to hospital routes with the risk of further infections) or by a 6-min walking test, while the anatomical/morphological data- are linked to the execution of imaging tests(procedures that require the patient's access within the hospital and exposure to the virus of other personnel and other environments) (Table 1).
Radiological imaging
Interstitial pneumonia is the main clinical manifestation of COVID-19. Pulmonary interstice is defined as a particular entity located between the alveolus and capillaries and is investigated mainly with radiological techniques. Interstitial pneumonia is characterized by the presence of edema and inflammatory cell infiltrate in the interstitial spaces (alveolar walls), more than in the alveolar cavities. It is only in the more advanced stages of the disease do they begin to fill the alveolar spaces, first in part [“ground glass” (GG)] and then total (consolidation). COVID-19 interstitial pneumonia does not have a specific manifestation, and we cannot define a patient as positive based only on the imaging picture. Pneumonia is in fact composed of a series of characteristics comparable with many other pneumonia or interstitial manifestations.
Standard chest radiographic examination (X-ray) is characterized by low sensitivity in identifying the earliest lung changes of COVID-19, which is characterized by GG opacities. Therefore, it is not the most suitable radiological examination, except for the initial diagnosis of exclusion of other bacterial alveolar pneumonia. However, it is necessary to consider that, in many of the community-acquired lung infections, the changes become manifest on chest Xray within a time interval usually 12 h from the beginning of the symptomatology;and, therefore, the examination can be negative if done too early.
In the more advanced stages of the infection, the chest X-ray examination shows bilateral multifocal alveolar opacities, which tend to confluence up to the complete opacification of the lung, with possible small associated pleural effusion(Figures 1 and 2).
In the early stages of the morbid process, chest computed tomography (CT) and particularly high resolution CT (HRCT) have a high diagnostic sensitivity. COVID-19 pneumonia, however, shows a varied and nonspecific HRCT patterns, similar to other lung infections, such as influenza A (H1N1),cytomegalovirus, other coronavirus (severe acute respiratory syndrome, Middle East respiratory syndrome), streptococcus and pneumonia from atypical germs (chlamydia,mycoplasma).
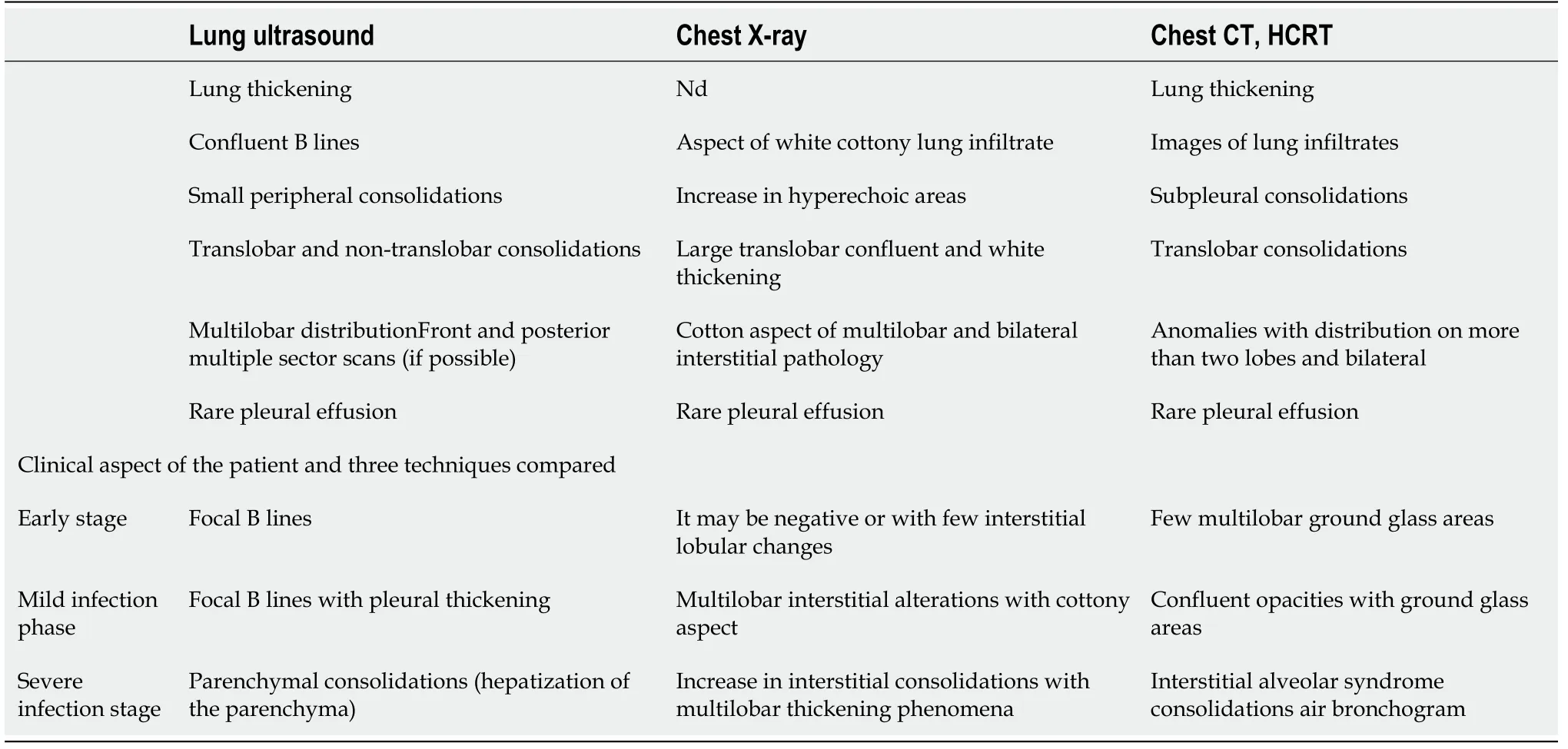
Table 1 Comparison of the three imaging methods in patient with coronavirus disease 2019 pneumonia
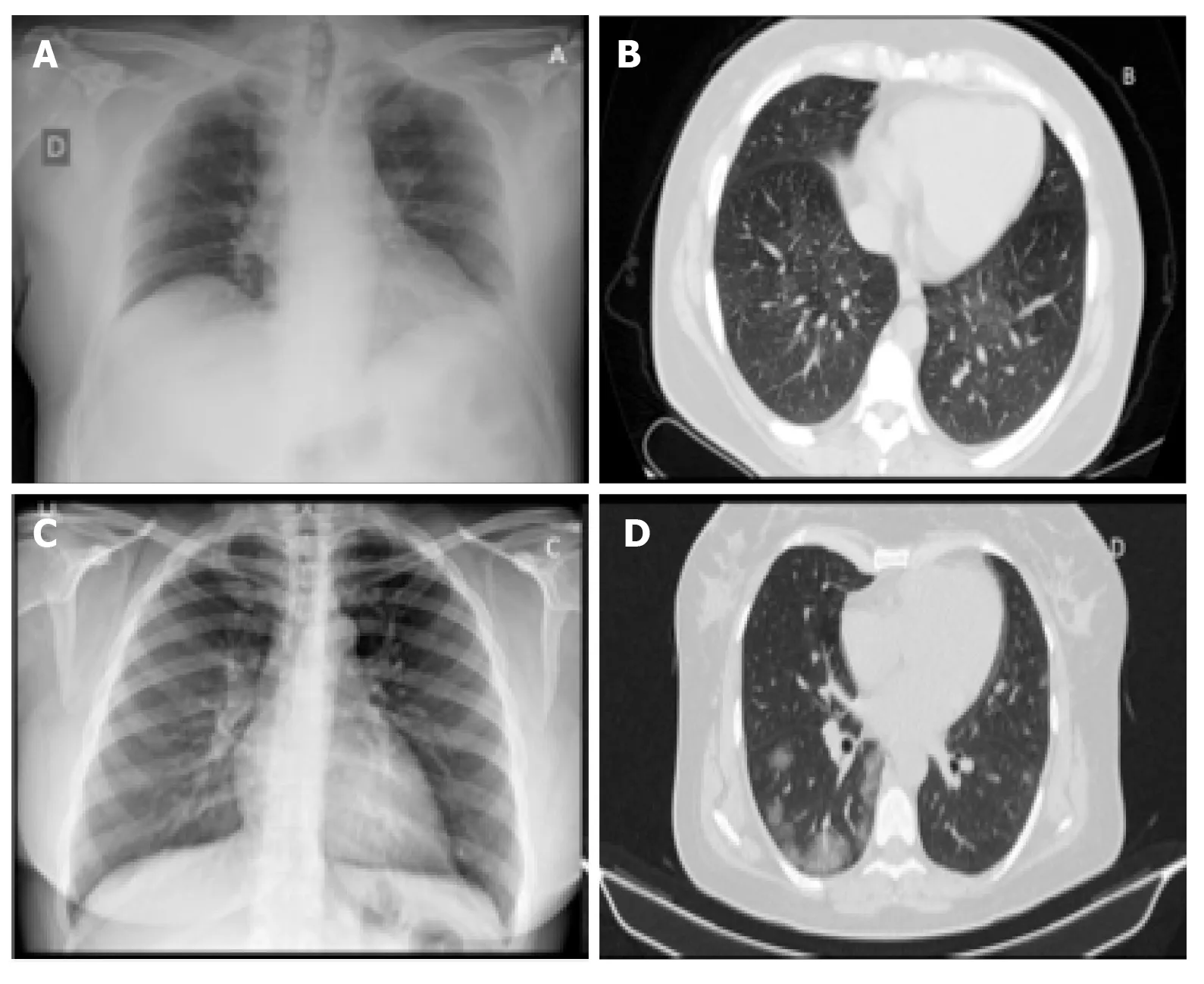
Figure 1 Standard chest X-ray and pulmonary computed tomography in a patient during early–stage and during the first week of coronavirus disease 2019 pneumonia. A, B: Presymptomatic phase: Few areas of hyperdensity with ground glass on computed tomography, mainly in the lower and posterior fields; C, D: First week of symptoms: Bilateral ground glass opacities more confluent on computed tomography.
HRCT is performed with a high resolution method (gold standard of interstitial disease), which allows to have a slice thickness between 0.625 mm and 1.25 mm,capable of showing the conditions of the interstitium or the hexagon formed by the secondary lobule.
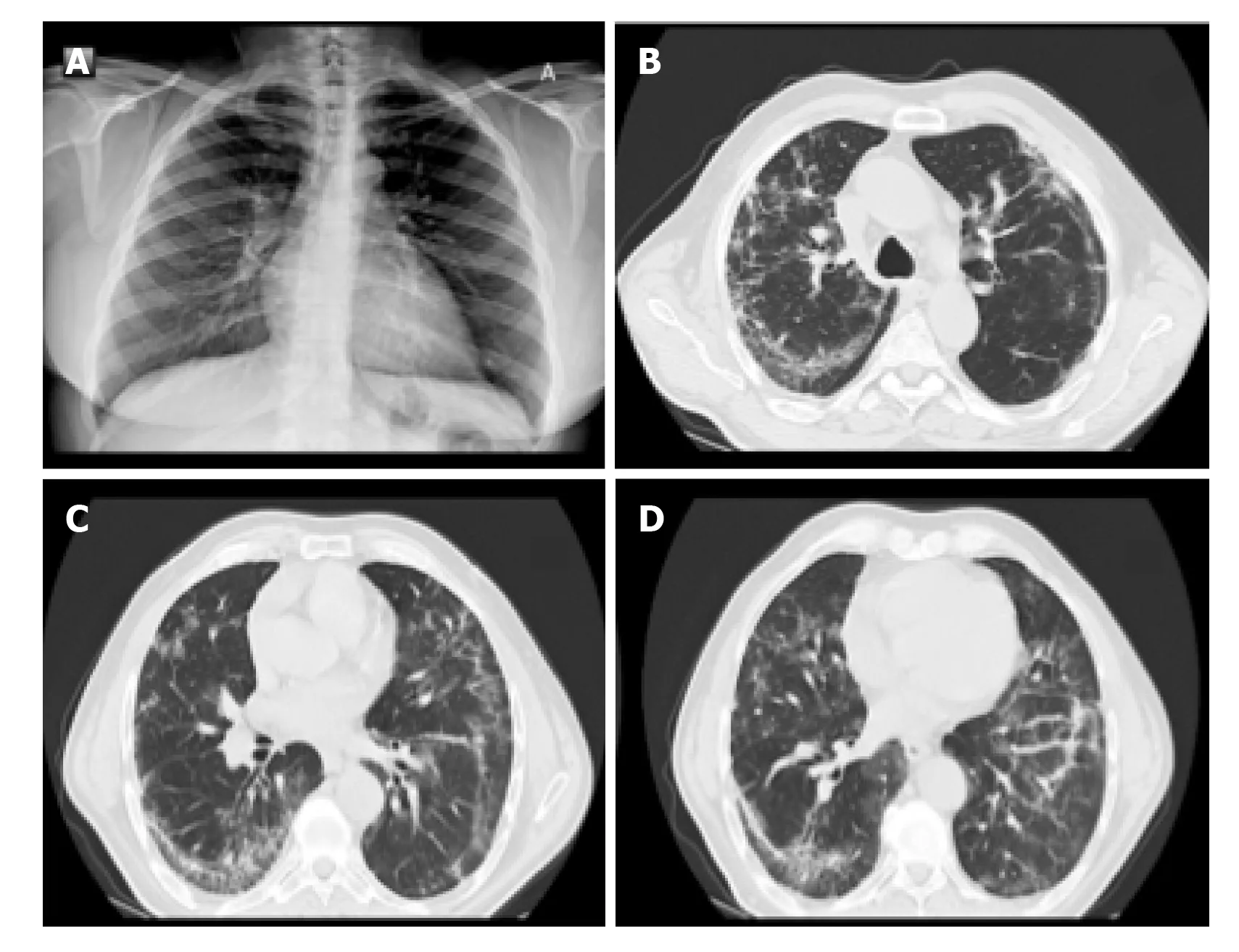
Figure 2 Standard chest X-ray and pulmonary computed tomography in a patient during the second week of severe coronavirus disease 2019 pneumonia.
The most common findings in HRCT were the multifocal bilateral GG areas,associated with consolidation areas with patchy distribution, mainly peripheral/subpleural, and with greater involvement of the posterior regions and lower lobes. As recently documented in a joint document of various scientific societies (Italian Society for Radiological Medicine, Italian Society for Ultrasound in Medicine and Biology and FISM), the "pure" focal or multifocal GG pattern and the"crazy paving" pattern were also observed in COVID-19 pneumonia, characterized by the presence of GG areas superimposed on smooth thickening of the interlobular and intralobular interstitium. Less commonly described are the presence of exclusive consolidations, the "reversed halo sign" (focal area of GG delimited by a more or less complete peripheral ring of consolidation) and cavitations, calcifications,lymphadenopathies and pleural effusion.
In addition to the early stages of diagnosis, HRCT is useful in assessing the course and severity of the disease; and, therefore, in guiding the patient's clinical management. While in the initial stages there are bilateral peripheral GG opacities, in more advanced phases of the disease, the segments involved increase in number, so that the GG extends and involves an increasing percentage of the parenchyma, passing from peripheral to more and more centralized. Furthermore, the areas previously GG increase in density, up to the final parenchymal consolidation. The evolution is characteristic of this specific pathology, since coronavirus is able to determine a primary viral pneumonia. In fact, while the other viral pneumonias consolidate when a bacterial infection overlaps, in COVID-19 infection, the same pathogen involves the most peripheral branches of the bronchial tree and so determines a parenchymal consolidation without bacterial superinfection (primary viral pneumonia).
The progression of the disease correlates with the increase in the number, size and density of the GG areas in HRCT examinations, with the appearance of widespread and bilateral parenchymal consolidations with air bronchogram in the context. CT,therefore, does not have a defined role in the initial phase, and perhaps not even in the final stages of the morbid process, but rather in the intermediate phase of the patient's diagnostic path to understand how necessary it is to be aggressive, fast and therapeutically impacting. Even the American College of Radiology states that CT should not be used for screening or as a first radiological line but only in hospitalized,symptomatic patients or in subjects with specific clinical indications(Figures 1-3).
Hence, CT shows an incremental power only when it can have an effective impact on the management and on the background therapy. For example, if we want to evaluate if and how much the pulmonary thickenings have increased to decide eventually to anticipate intubation, then CT is appropriate. If, on the other hand, we simply want to acknowledge that the patient is getting worse, but the therapy is already maximized, it does not make sense to perform the CT, as it is important to avoid unnecessary infectious risks in transporting the patient to the radiology department.
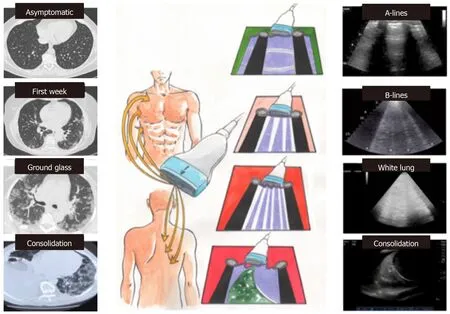
Figure 3 Correlations between bedside lung ultrasound and pulmonary computed tomography during the different phases of coronavirus disease 2019 pneumonia.
Lung ultrasound
Bedside pulmonary echography in a clinical setting such as COVID pneumonia has an undeniable set of benefits, such as improved ease of disinfection, less contact area with patients and the ability to perform the exam without moving the patient on a stretcher,thus reducing the risk of spreading the virus while respecting the appropriate protection measures. The inability to maintain a minimum doctor-patient safety distance makes it one of the tests that puts health professionals at risk.
To increase significantly the sensitivity of the lung ultrasound, a thorough examination is necessary, adopting an antero-posterior window and trying to visualize the lung as much as possible in a 12-segment approach (each lung is divided in three areas by the anterior and posterior axillary lines: Front, lateral and posterior). The high frequency linear probe may be preferable to obtain high resolution images of the pleural line (the first horizontal line encountered in the scan, 1-2 mm thick depending on the probe used) to distinguish between a regular and normal sliding pleural line(“sliding”) with respect to a thickened, irregular or interrupted pleural line or with no sliding (as occurs in pneumothorax).
The key aspects to distinguish in lung scan are: (1) A lines: Normal reverberation artifacts of the ultrasound beam on the pleura/pulmonary air interface; hyperechoic(white) lines horizontal and parallel to each other and to the pleural line, typical of the healthy lung; (2) B lines (“comet tail”): Pathological artifacts typical of the interstitial disease (from pulmonary oedema to interstitial pneumonia); vertical hyperechoic lines perpendicular to the pleural line, which provide from the pleural line itself (not from the skin), direct themselves in depth and mask the A lines, preventing their visualization. The more these lines are numerous, close and coalescent, the worse is the involvement of the interstitium; (3) Pulmonary consolidation: When the degree of pulmonary aeration is reduced and the air in the alveolar spaces is replaced by exudate/inflammatory cells, the ultrasound beam is able to penetrate the parenchyma showing a “consolidation” with an ecostructural pattern similar to that of the liver(hepatization of the lung); and (4) Pleural effusion: Pulmonary ultrasound is certainly the gold standard in the diagnosis of pleural effusion. In this condition, the investigation has a very high sensitivity and specificity and allows to evaluate correctly the volume of the effusion and the echogenicity (transudate vs corpuscular exudate).
Pulmonary ultrasound results in COVID pneumonia seem to correlate very well with the results of chest CT. With the increasing severity of the disease, the following evolution has been observed: (1) Presymptomatic phase: Few areas of hyperdensity with GG at CT, mainly in the lower and posterior fields, related to the echographic B lines alternating with areas with normal A lines (“patchy”); reduced mobility of the diaphragms from the early days; (2) First week of symptoms: bilateral GG opacities more confluent on CT, related to the coalescing B lines that form “patches of white”(“waterfall sign”), and wrinkled pleural line; (3) Second week: Small peripheral subpleural bilateral consolidation on CT and echography, with evolution in “dry lung”and dense and fixed B lines with respect to pleural sliding; and (4) In the most severe form, the volume of the consolidated lung progressively increases, with the absence of color at the color-doppler of the consolidations, and the possible evolution towards ARDS (Figure 3). Within the consolidated lung there are hyperechoic branched consolidations (those that are aerial bronchograms on CT).
Other interesting features are: Peripheral pulmonary anomalies can cause interruption and thickening of the pleural line; areas of normal lung (with an A line pattern) can be observed at the beginning of the disease or during recovery; small pleural effusions may be observed, while larger pleural effusions are uncommon.
The chest echography is highly indicated for the daily evaluation of the lung picture and the monitoring of therapy. In a prognostic sense we can distinguish two fundamental frameworks: Pattern 1: Beginning interstitial disease with B lines spread also to the anterior fields, usually in the “positive end-expiratory pressure (PEEP)responders”; Pattern 2: Ventilated front areas (A lines), thickened posterior areas(“white lung”), responsive to the pronation.
Transthoracic echocardiography
The echocardiogram in this clinical context can be useful in selected cases in detecting regional or global anomalies of the contractility of the left ventricle and in documenting the possible acute overload of the right ventricle, in case of ARDS,especially in the presence of hemodynamic instability. It should be noted that acute myocardial damage (significant increase in troponin or ischemic electrocardiograph abnormalities) was found to be, in two recent analyses with a total of more than 600 patients with established COVID infection, significantly associated with the fatal outcome, while the prognosis of patients with underlying chronic heart disease but without acute myocardial damage was relatively favorable. Inflammation can be a potential determinant mechanism for myocardial injury, and an aggressive therapeutic approach can be considered for patients at high risk of myocardial injury.
The National Society for Hospital Cardiologists like other societies, such as the Italian Society of Cardiology and Italian Society of Cardiovascular Imaging, given the importance of the health phenomenon, has recently disclosed documents aimed at highlighting the importance of a correct procedure and execution of cardiology consultancy and echocardiography, especially in pandemic COVID-19 pneumonia.All cardiological scientific societies believe it is important to ensure the execution of urgent and non-deferrable exams in the patient with hemodynamic instability,maintaining the possibility for the cardiologist to be able to refuse the execution of tests not considered appropriate in his own judgement and favoring the different and possible forms of remote electrocardiograph and imaging consultations, thus limiting access to infected areas.
Even the American Society of Echocardiography recently underlined how it is necessary in COVID-19 infections to select the indications for the echocardiogram,limiting it to urgent patients, to be carried out with personal protective equipment(PPE) and the necessary hygiene rules. In particular, a single echocardiograph should be identified, preferably portable and of reduced dimensions to facilitate sanitation, when possible using probe covers, and the examination should be carried out by a single operator, of sufficient experience (not in training), with a scan that is a good compromise between adequacy and speed of execution (limited ultrasound sections; bimodal responses with high clinical impact; image registration and subsequent “off line” review). Particular attention is then placed on the execution of a possible transesophageal echocardiogram, the procedure itself “generating aerosol”and therefore putting those at greater infectious risk, to be limited in non-urgent indications and to be carried out with complete PPE (e.g., mask at least N95 according to American classification or FFP2 according to the European classification). The need to ensure the training of health personnel on the correct methodologies for wearing and above all removing PPE is also underlined (Figures 4 and 5).
At present, there are no echocardiographic studies conducted specifically in COVID-19 patients. However, the role of the echocardiogram in monitoring biventricular function and septic shock is well known. In the past 10 years, most studies on acute myocardial dysfunction during sepsis have been conducted in patients admitted to intensive care and subjected to mechanical ventilation, using transesophageal echocardiography. From these studies it emerged that about 30%-40% of septic patients develop reduction of the ejection fraction of the left ventricle(LV), impaired LV diastolic function and possible impairment of the function of the right sections, which is currently less characterized but present above all during ARDS. Another aspect that should be underlined is the definite hemodynamic effect of ventilation on ventricular performance. Positive end-expiratory pressure,increasing lung volumes, can cause an increase in pulmonary vascular resistance(PVR) due to the compression of alveolar and extra-alveolar capillaries, with consequent increase in afterload and right ventricle (RV) volume, shift of the interventricular septum to the left and consequent reduction of compliance and filling of LV. However, since the increase in PVR is countered by the elimination of hypoxiainduced vasoconstriction, the net increase in PVR becomes relevant only for high PEEP values. The increase in intrathoracic pressure also determinates an increase in the resistance of the intrathoracic veins, a mechanism that reduces the gradient and venous return for RV, especially in conditions of true hypovolemia (anemia,dehydration, etc. in a healthy heart) or relative hypovolemia (severe RV dysfunction).This phenomenon, however, is counterbalanced by the increase in abdominal pressure due to the lowering of the diaphragm with the effect of “squeezing” on the liver and the spleen. Therefore, in clinical practice, the potential negative hemodynamic effects of PEEP (hypotension secondary to reduced preload and increased RV afterload) are mainly confined to patients highly dependent on preload and can be partially balanced by carrying out a preventive volemic filling.
COMPARISON BETWEEN METHODS
The sensitivity of chest X-ray in reported COVID-19 cases was 59%, compared to 86%for lung CT, especially in detecting subtle opacities. The real sensitivity of pulmonary ultrasound in this context is not clearly defined. It will depend on several factors (in particular the severity of the disease, the presence of obesity or high acoustic impedance of the chest, the completeness of the scan and the experience of the operator). A complete lung ultrasound examination should exhibit an intermediate sensitivity between CT scan and chest radiography. There is no established data yet,but it is reasonable to extrapolate the experiences in other types of pneumonia.Specificity is certainly low. An irregular B-line or consolidation pattern can be observed in any pneumonia or interstitial lung disease. Therefore, a clinical correlation is absolutely necessary (e.g., evaluation of previous chest imaging studies to evaluate if chronic abnormalities are present). Also, it should be note that hospitalized supine patients may have B-lines and consolidation in a posterior and inferior distribution due to atelectasis. Hence, pulmonary echography can have the greatest sensitivity and specificity among outpatient or first aid patients (Table 1).
However, the serial control of the individual patient could be very useful in the context of respiratory intensive care. The evolution of a focal “white lung” in a “dry lung” with widespread sub-pleural consolidations is an indication of an unfavorable evolution of the pathology, with the consequent need for more aggressive treatment with oral-tracheal intubation rather than non-invasive ventilation. Pulmonary echography also allows checking for the presence of pneumothorax (absence of pleural sliding), new thickenings from bacterial over-infection and pleural effusion, all obviously without having to move the patient.
CONCLUSION
The integrated clinical, laboratory, radiological and ultrasound approach to the patient’s bed is fundamental in the diagnosis, monitoring and evaluation of the therapy of the patient with severe acute pneumonia due to COVID-19. Thoracic echography is a very important and well developed diagnostic path, especially in Italy, which allows to avoid unnecessary CT scans and, at the same time, highlight and monitor parenchymal damage without moving the patient. CT should not be performed routinely for all patients, because in the first 48 h it can be absolutely negative, and in the late phase the imaging finding may not change the therapeutic approach.
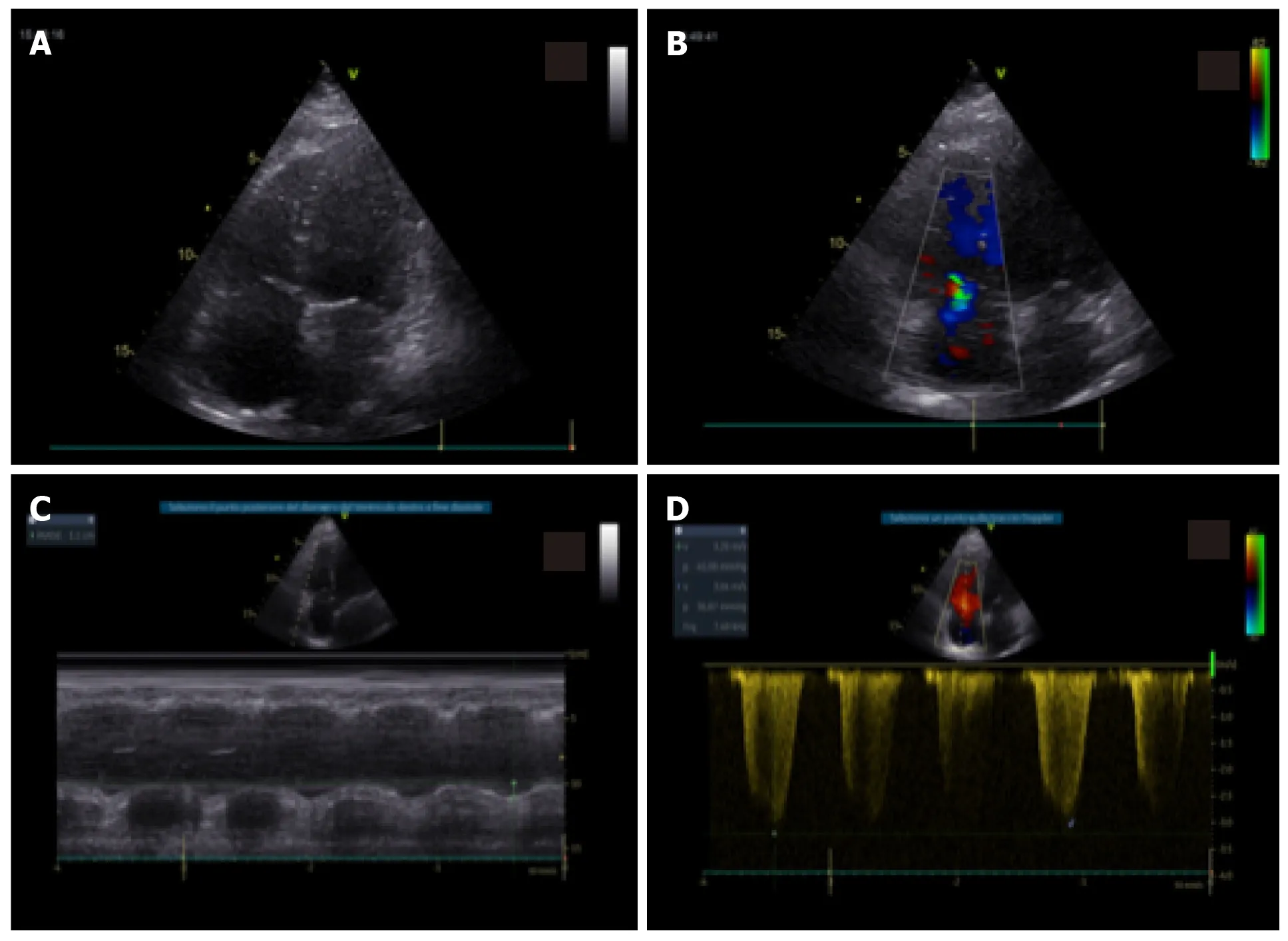
Figure 4 Standard echocardiography in a patient with coronavirus disease 2019 pneumonia and right ventricular impairment. A: In apical four-chamber view, mild right ventricular dilatation; B: Mild tricuspid regurgitation; C: With moderate impairment of right ventricular function with reduced tricuspid annular plane systolic excursion; D: Increase in pulmonary pressures.
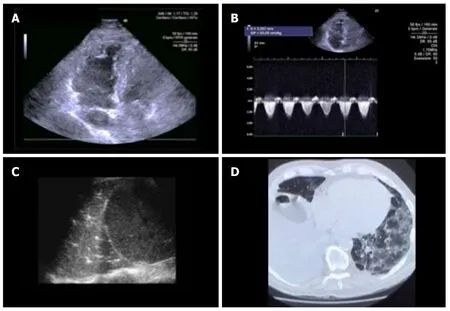
Figure 5 Standard echocardiography, lung ultrasound and pulmonary computed tomography in a patient with coronavirus disease 2019 pneumonia. A: In apical four-chamber view, mild right ventricular dilatation; B: With increase in pulmonary pressures; C: By lung ultrasound; D: Pulmonary computed tomography ground glass with presence of consolidation areas.
 World Journal of Radiology2020年11期
World Journal of Radiology2020年11期
- World Journal of Radiology的其它文章
- Clinical features and radiological manifestations of COVID-19 disease
