The first two cases of transcatheter mitral valve repair with ARTO system in Asia
Kai-da Ren, Zhao-xia Pu, Lei Yu, Feng Gao, Li-han Wang, Stella Ng, Ju-bo Jiang, Hua-jun Li, Yong Xu, Wei He,Min Yan, Xian-bao Liu, Jian-an Wang
Cardiovascular Department, the Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310009, China
KEY WORDS: Mitral regurgitation; Mitral valve repair; ARTO system
INTRODUCTION
Epidemiological investigations reveal that moderateto-severe mitral regurgitation (MR) is present in about 74% of in-patients and 45% of outpatients with systolic heart failure (HF), and the mortality is higher in functional mitral regurgitation (FMR) patients than in non-FMR patients.[1]Surgical repair of FMR is feasible and has been shown to improve functional status.[2,3]However,patients with mitral valve disease may be asymptomatic or have mild symptoms at their early stages, which result in that many patients with advanced age are ineligible for surgeries once severe symptoms occur.[4]
Previous research[5]has already shown that the increase in the septal-lateral dimension is the primary change in the mitral annulus in FMR. So, the ARTO system (MVRx Inc., Belmont, California) is designed to shorten the septal-lateral dimension to treat FMR for patients who cannot tolerate surgeries.[6]This system includes a suture that connects interatrial-septal and coronary sinus anchors. This suture is tensioned to shorten the anteroposterior (AP) diameter of the mitral annulus, thereby improving mitral leaf let coaptation and reducing FMR. MAVERIC (Mitral Valve Repair Clinical Trial) validates the safety and efficacy of the ARTO system for FMR in patients with symptomatic HF.[7]As a well-recognized cardiovascular intervention center,we can perform transcatheter aortic valve replacement(TAVR) utilizing the VenusA-Plus valve.[8]Herein, we describe the first two successful cases of mitral valve repairs using th e ARTO system in Asia.
METHODS
Patients
Patient 1 was a 70-year-old man with a history of dyspnea, who was admitted to the hospital for HF exacerbation. NYHA functional class of this patient was grade IV, due to reduced ejection fraction and concomitant severe MR. Despite optimal medical therapy during the previous 3 months, the patient was still experiencing two episodes of HF exacerbation,requiring hospitalization and use of intravenous diuretics.Moreover, because of his poor heart function, he had an implantable cardioverter-defibrillator (ICD) implanted one month ago. Echocardiography (TTE, 2D/3DTEE)confirmed moderate left ventricular dysfunction (LVIDd 7.45 cm; EF 34.6%) with severe functional MR (EROA 0.49 cm2; MRvol 49 mL).
Patient 2 was a 63-year-old woman, who was admitted to the hospital for progressively worsening dyspnea for 2 years. She had a pacemaker implantation 2 years ago because of type III atrioventricular block, type II diabetes, and NYHA of grade IV. Echocardiography(TTE, 2D/3DTEE) now confirmed moderate left ventricular dysfunction (LVIDd 5.76 cm; EF 42.9%) with severe functional MR (EROA 0.57 cm2; MRvol 75 mL).
Procedures
After discussions with cardiovascular services,percutaneous interventions with the ARTO system were planned for these two patients. Procedures were performed under general anaesthesia in a hybrid catheterization lab with the capability of cardiopulmonary bypass. Two magnetic catheters were used, one was placed in the coronary sinus (CS)through the right internal jugular vein while the other was placed in the left atrium (LA) through the right femoral vein. The two MagneCaths were manipulated and linked magnetically. Then, a small puncturing wire was advanced from the CS into the LA MagneCath and externalized to create a continuous loop wire from the right internal jugular vein to the right femoral vein. A 3-cm CS anchor (T-Bar, MVRx Inc.) was then placed in the coronary sinus and connected to an atrial septal anchor by a suture of adjustable length. The MR of the patient was reduced from severe to moderate assessed by transoesophageal echocardiography (TEE), and postshortening of the AP diameter of the mitral annulus was achieved by adjusting the length of the suture. The suture was then “l(fā)ocked” and cut, allowing removal of the delivery system via the femoral vein and jugular vein.
RESULTS
The procedures were completed in these two patients without any complications. Moreover, the postoperative courses were uneventful for both patients, with no requirements of blood transfusion,pacemaker insertion, stroke, prolonged ventilation, or reoperation. In these two patients, the AP diameters were immediately shortened, and the MR grades were reduced from severe to moderate after the procedures.The NYHA functional classs were improved to grade II for both patients during the hospitalization. Then,after several days of hospital stay, these two patients were discharged without evident dyspnea or chest tightness. The 30-day and 3-month TTE revealed a moderate to severe MR in both patients. At the 3-month follow-up visits, the NYHA functional classes were grade II for the first patient and grade III/IV for the second patient. The result of the first patient is shown in Figure 1.
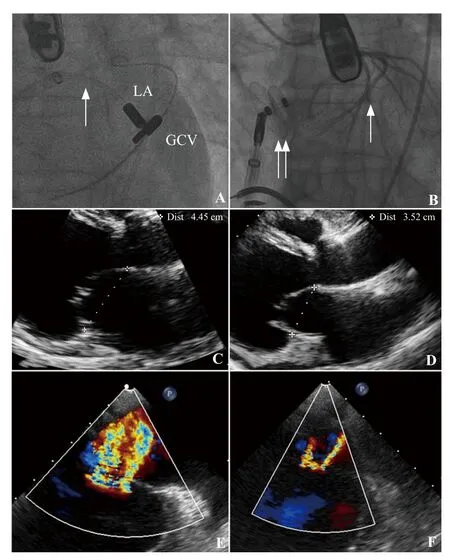
Figure 1. The result of the first patient. A: left atrium (LA) and great cardiac vein (GCV) MagneCaths magnetically linked with a crossing wire passing from the GCV into the LA MagneCath (arrow); B: the final angiographic appearance of the ARTO system after tensioning and suture lock; the GCV anchor (T-Bar) was indicated by the single arrow and the septal anchor by the double arrow; C: baseline T transoesophageal echocardiography (TEE) showing the anteroposterior(AP) diameter was 4.45 cm; D: post-procedure TEE showing the AP diameter was 3.52 cm; E: baseline TEE color Doppler showing severe FMR; F: post-procedure TEE color Doppler showing moderate MR.
DISCUSSION
FMR can arise from left ventricular enlargement with previous myocardial infarction and papillary muscle displacement.[9-11]With increasing age, cardiac remodelling, which is caused by volume overload, may lead to pulmonary hypertension, atrial fibrillation, and HF. Hence, the long-term survival rate of severe MR patients decreases by 6.3% every year.[4]Usually the risk is too high for some patients with severe MR to undergo surgery. The ARTO system provides a suitable solution for these patients.
The ARTO system is safe, effective, and reproducible, as demonstrated in animal studies and clinical settings.[12,13]In a recent study, 11 patients received the ARTO system, and there were no procedural adverse events.[7]In this study, effective regurgitant orifice area and regurgitant volumes decreased significantly. Also, the NYHA functional class was improved for most of the patients. Only two adverse events happened at 30-day follow-ups: one pericardial effusion requiring surgical drainage and one device dislodgement, which presented with no initial symptoms in the patients.
In this report, we presented the first two successful cases of ARTO procedure in Asia. The results showed an immediate reduction in MR with no adverse events.There were no conduction disturbances, stroke, bleeding,or other complications seen in these two patients.However, the improvement of MR grade is not as significant as we expected, which may be due to the complexity of the procedure. More experiences with the system are needed to achieve a better outcome.Furthermore, it is difficult for the T-bar to be located just across the atrial septal anchor, which cannot ideally shorten the septal-lateral distance. Moreover, the improvement of NYHA functional class may be partly due to the medical therapies in the hospital. During the follow-up, these two patients still had moderate to severe MR and limited heart function improvement, especially for the second patient. There are paramount needs in advanced medical managements and familiarity with the ARTO system itself.
We also performed this procedure on another severe FMR patient, which was not successful due to coronary sinus stenosis, and the catheter could not get to the distal segment of the coronary sinus. The patient was discharged from hospital in a stable condition after 6 days of conservative therapy. This reminds us of the importance of establishing a strict protocol of inclusion criteria.
CONCLUSION
In this study, we report the first two successful cases using ARTO procedures in Asia. The clinical results may be even more significantly improved with a careful selection of patients and overcoming the learning curve of the technique.
Funding:This study was supported by Advanced Technique Research of Valvular Heart Disease Treatment Project (2015C03028);Role of TPP1 in anti-senescence and functional optimization of aged mesenchymal stem cells (81570233); Role of FAIM in survival and functional improvement for aged mesenchymal stem cells (81770253); Zhejiang Clinical Research Center for Cardiovascular and Cerebrovascular Disease (2018E50002).
Ethical approval:This study protocol was approved by the Ethical Committee of the Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China.
Conflicts of interest:The authors declare that they have no competing interests. The funders had no role in the design,conduct, analysis, or interpretation of data or in writing the manuscript.
Contributors:JAW, XBL, ZXP, LY, FG, YX, WH, and MY performed the procedure. KDR, JBJ, LHW, and HJL evaluated the patients for ARTO system. XBL, KDR and SN wrote the manuscript. JAW revised and edited the manuscript. All authors read and approved the f inal manuscript.
REFERENCESS
1 Robbins JD, Maniar PB, Cotts W, Parker MA, Bonow RO,Gheorghiade M. Prevalence and severity of mitral regurgitation in chronic systolic heart failure. Am J Cardiol. 2003;91(3):360-2.
2 Bolling SF, Pagani FD, Deeb GM, Bach DS. Intermediate-term outcome of mitral reconstruction in cardiomyopathy. J Thorac Cardiovasc Surg. 1998;115(2):381-8.
3 Hausmann H, Siniawski R. Mitral valve reconstruction and replacement for ischemic mitral insufficiency: seven years'follow up. J Heart Valve Dis. 1999;8(5):536-42.
4 Enriquez-Sarano M. Timing of mitral valve surgery. Heart.2002;87(1):79-85.
5 Timek TA, Dagum P, Lai DT, Liang D, Daughters GT, Ingels NB Jr, et al. Pathogenesis of mitral regurgitation in tachycardiainduced cardiomyopathy. Circulation. 2001;104(suppl 1):I-47-I-53.
6 Palacios IF, Condado JA, Brandi S, Rodriguez V, Bosch F,Silva G, et al. Safety and feasibility of acute percutaneous septal sinus shortening: First-in-human experience. Cathet Cardiovasc Intervent. 2007;69(4):513-8.
7 Rogers JH, Thomas M, Morice MC, Narbute I, Zabunova M.Treatment of heart failure with associated functional mitral regurgitation using the ARTO system: initial results of the firstin-human MAVERIC Trial (Mitral Valve Repair Clinical Trial).JACC Cardiovasc Interv. 2015;8(8):1095-104.
8 Liu XB, He YX, Liu CH, Wang LH, Gao F, Yu L, et al. First-inman implantation of the retrievable and repositionable VenusAPlus valve. World J Emerg Med. 2018;9(1):64-6.
9 Sabbah HN, Rosman H, Kono T, Alam M, Khaja F, Goldstein S. On the mechanism of functional mitral regurgitation. Am J Cardiol. 1993;72(14):1074-6.
10 Otsuji Y, Handschumacher MD, Schwammenthal E, Jiang L,Song JK, Guerrero JL, et al. Insights from three-dimensional echocardiography into the mechanism of functional mitral regurgitation. Circulation. 1997;96(6):1999-2008.
11 Kono T, Sabbah HN, Rosman H, Alam M, Jafri S, Goldstein S.Left ventricular shape is the primary determinant of functional mitral regurgitation in heart failure. J Am Coll Cardiol.1992;20(7):1594-8.
12 Rogers JH, Macoviak JA, Rahdert DA, Takeda PA, Palacios IF, Low RI. Percutaneous septal sinus shortening: a novel procedure for the treatment of functional mitral regurgitation.Circulation. 2006;113(19):2329-34. Epub 2006 May 8.
13 T ibayan FA, Rodriguez F, Langer F, Zasio MK, Bailey L,Liang D, et al. Does septal-lateral annular cinching work for chronic ischemic mitral regurgitation? J Thorac Cardiovasc Surg. 2004;127(3):654-63.
 World journal of emergency medicine2020年1期
World journal of emergency medicine2020年1期
- World journal of emergency medicine的其它文章
- Surgical closure of large splenorenal shunt may accelerate recovery from hepato-pulmonary syndrome in liver transplant patients
- Investigations for the assessment of adult patients presenting to the emergency department with supraventricular tachycardia
- Epidemiological characteristics and disease spectrum of emergency patients in two cities in China: Hong Kong and Shenzhen
- Role of penehyclidine in acute organophosphorus pesticide poisoning
- Admission delay is associated with worse surgical outcomes for elderly hip fracture patients: A retrospective observational study
- A pulmonary source of infection in patients with sepsis-associated acute kidney injury leads to a worse outcome and poor recovery of kidney function
