Physicians’ views on the usefulness of practical tools for assessing the driving ability of older drivers: a cross- sectional study
Paul Sebo
ABSTRACT
INTRODUCTION
With increased longevity and improved health of older drivers, the number of older drivers is expected to increase over the next decades.12Although older drivers tend to have more favourable driving habits, for example, in terms of observation of speed limits,13a number of health issues occurring more often in the elderly, such as sensory, motor or cognitive decline, could impair their driving performance.45
National programmes for assessing older drivers’ fitness to drive have been developed in several countries,6although there is no agreement to date on the level of association between the result of these assessments and future driving ability.7-9In Switzerland, at the time of the study, a medical examination was mandatory every 2 years for all drivers over 70 years of age. A revision of the Road Traffic Act that came into force after the end of the study (in January 2019) raised the minimum age for this medical examination to 75. This examination is carried out by general practitioners (GPs), except in Geneva where it is undertaken by the medical assessors of the road traffic office. These assessors are all physicians and most of them are also GPs (of the 69 medical assessors 60 were GPs at the time of the study). The prerequisites for carrying out these examinations vary from canton to canton: in Geneva, medical assessors have to attend a 1 day theoretical training course, whereas in other cantons, GPs only have to identify themselves to the competent cantonal authorities.
Physicians are asked to identify medical conditions that could affect the driving ability of older drivers. At the end of the assessment, they complete a form, which is returned to the road traffic office with a general recommendation (fit to drive, fit to drive with constraints, unfit to drive or furtherevaluation required). About 2% of older drivers are considered medically unfit to drive in Switzerland, mainly due to cognitive (64%) and visual (18%) impairments.10This figure does not include older drivers who are considered unfit after reports from the police, family members or health professionals. In Switzerland, health professionals can report patients they consider unfit to drive to the road traffic office at any time (these patients then undergo a thorough medical assessment and possibly a temporary or permanent licence revocation). However, this is a voluntary procedure; physicians do not have the legal obligation to report unfit- to- drive patients to the competent authority.
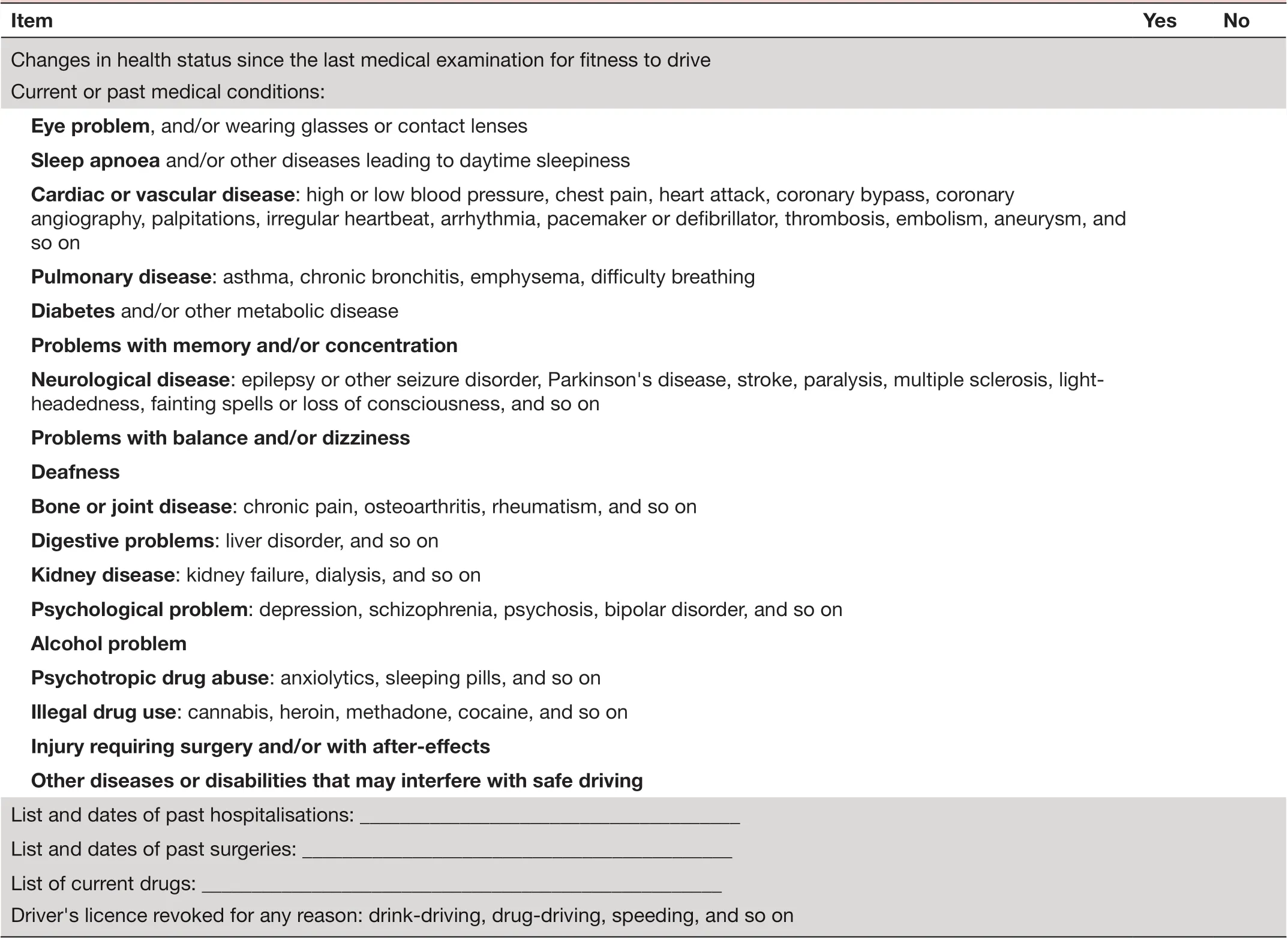
TabIe 1 Older driver preconsultation self- administered questionnaire on health
To simplify their task, physicians can use the information sources provided by the traffic medicine website (medtraffic. ch) and the publications of traffic medicine experts in local medicine journals.11In addition, traffic medicine experts have recently developed a standardised self- administered questionnaire based on Swiss recommendations that can be completed by older drivers before the consultation and used by physicians to guide their assessment (see table 1 for the English version of the older driver preconsultation self- administered questionnaire on health). As part of the development of self- assessment instruments promoting self- regulation, the self- administered questionnaire could also be completed by older drivers at home in order to help raise awareness of their driving skills.
To our knowledge, there are no studies in Switzerland that explored physicians’ views on the usefulness of these practical tools and information sources. Only a few foreign studies addressed this theme. A Canadian study found that a large number of physicians were not aware (24%) and, among those who were aware, did not use (31%) the reference book published by the Canadian Medical Association titledDetermining medical fitness to drive: a guide for physicians.12An American study found that 69% of physicians were not aware of the American Medical Association guidelines regarding medical conditions affecting older drivers.13
In this study, we aimed to explore physicians’ views on the usefulness of two practical tools to guide fitness- to- drive assessments and the use by physicians of the information sources provided by the Swiss traffic medicine website, first overall and then according to physicians’ characteristics. In particular, we aimed to compare responses according to whether participants were medical assessors or GPs. Our hypothesis was that those who were not medical assessors, those who were younger physicians and those with fewer fitness- to- drive assessments (because these physicians are generally less experienced), and female physicians (because they are more likely to follow the recommendations than their male counterparts)14would find these two practical tools more useful and visit the traffic medicine website more often.
METHODS
As planned by the study team, this cross- sectional study was nested within a practice review carried out in 2017, designed to describe the fitness- to- drive assessment practices of physicians in the French- speaking part of Switzerland.11The manuscript follows the Strengthening the Reporting of Observational Studies in Epidemiology guidelines for reporting observational studies.
Survey site, survey population and data collection
We randomly selected 500 GPs practising in the cantons of Vaud, Jura and Neuchatel (sample fraction: 500/1075; probability weight: 2.15), hereinafter referred as ‘regular practice GPs’. We also selected all medical assessors of the road traffic office in Geneva (n=69; probability weight: 1). All medical assessors and selected regular practice GPs were asked to complete a paper questionnaire withsociodemographic items(gender, age, practice location, number of half days worked per week) and questions aboutfitness-to-drive assessments(estimated mean number of assessments per week and content of their assessments). In addition, physicians were asked to rate theperceived usefulness of a standardised questionnairecompleted by older drivers before the consultation anda reference guidesummarising the Swiss recommendations on the fitness- to- drive assessment of older drivers, on a 5- point Likert scale ranging from ‘not useful’ (0) to ‘very useful’ (4). Finally, they were asked to rate thefrequency of use of the information sources provided by the traffic medicine website ( medtraffic. ch),on a 5- point Likert scale ranging from ‘never used’ (0) to ‘a(chǎn)lways used’ (4).
For the part of the questionnaire dealing with the content of fitness- to- drive assessments, physicians were asked to report the procedures they performed during the assessments (see box 1: medical fitness to drive/driving history patient questionnaire), scoring them on a 5- point Likert scale ranging from ‘never performed’ (0) to ‘a(chǎn)lways performed’ (4). These items were selected by consensus within the research team, which included three traffic medicine specialists and three academic GPs. The questionnaire was pretested with five GPs practising in Geneva.
Confidentiality and ethical approval
All collected data remained confidential. We presumed tacit consent if the physicians sent back the questionnaire. According to Swiss law, this study did not require ethical review, because we did not collect personal health- related data.
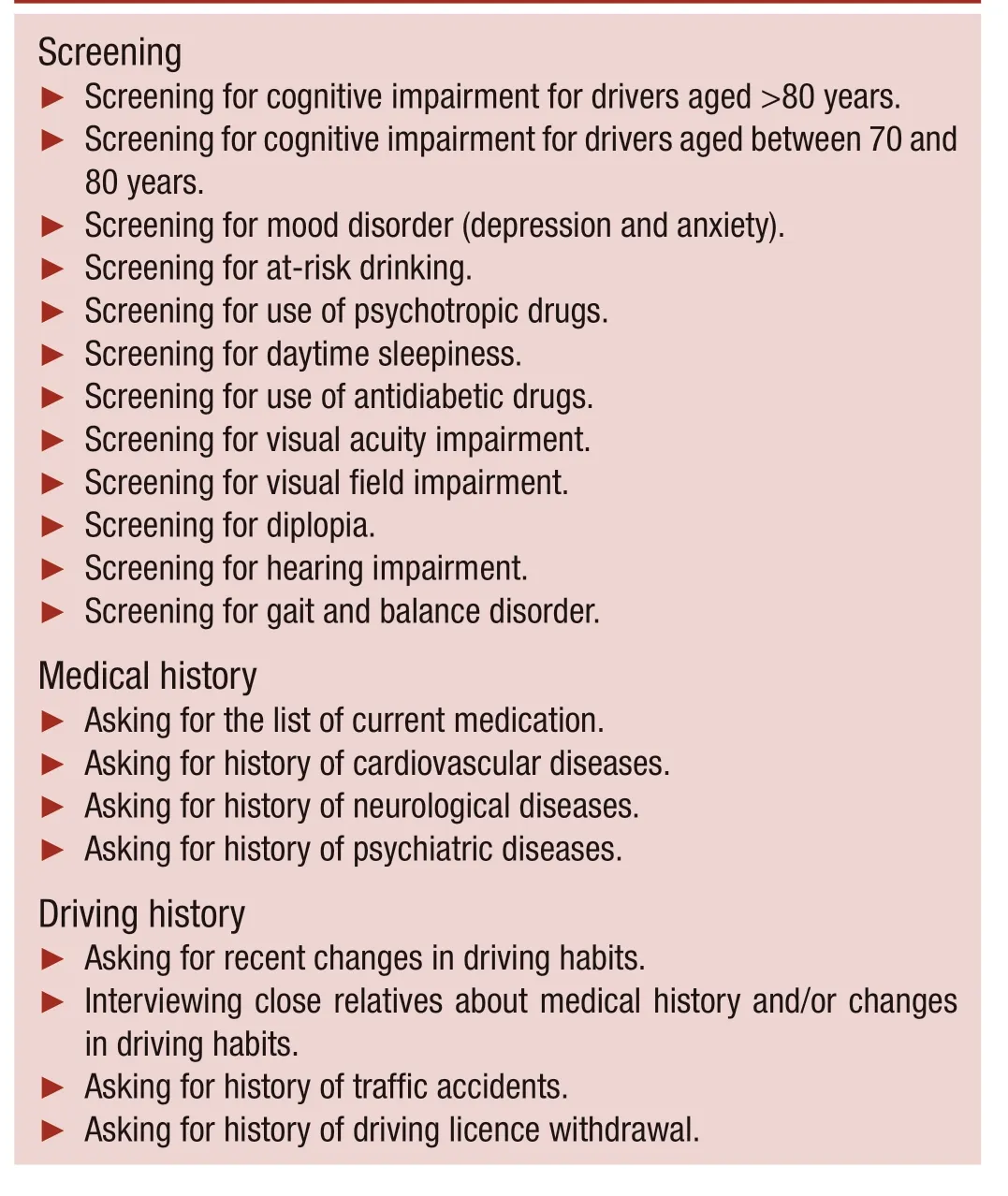
Box 1 Medical fitness to drive/driving history patient questionnaire
Statistical analyses and sample size
We described physicians’ characteristics (sociodemographic characteristics and those related to fitness- to- drive assessments), using frequency tables for categorical variables, and medians and IQR for numerical data (not normally distributed). We compared these characteristics between medical assessors and regular practice GPs using design- basedFtests (corrected weighted Pearson χ2tests) for categorical variables and Wilcoxon rank- sum tests for numerical data.
We computed the proportion of physicians who judged that these assessment tools would be very useful (4/4) or somewhat useful (3/4), and the proportion of physicians who always (4/4) or often (3/4) use these information sources, and we compared the responses between physicians’ subgroups using design- basedFtests. For these tests, we dichotomised the number of fitness- to- drive assessments into ≤2 and >2 per week and the number of procedures often or always performed into <15 and ≥15. The cut- off points were set at 2 and 15, respectively, as they were the medians of the distribution. We used survey data analyses because we had to take into account the stratified random sampling.
Finally, we carried out weighted logistic regressions for all variables showing statistically significant differences between the subgroups, to assess whether the observed differences could be due to sociodemographic factors.
The required sample size was computed for the practice review.11For the current study, we wanted a 95% CIwidth of about 0.15 (15%) around the estimate. Given the formula for the estimation of a proportion (n=1.962× proportion × (1- proportion) / precision2), the minimal sample size required for the study was 171 (proportion used in the formula=0.5). The sample size estimated for the practice review met these requirements.
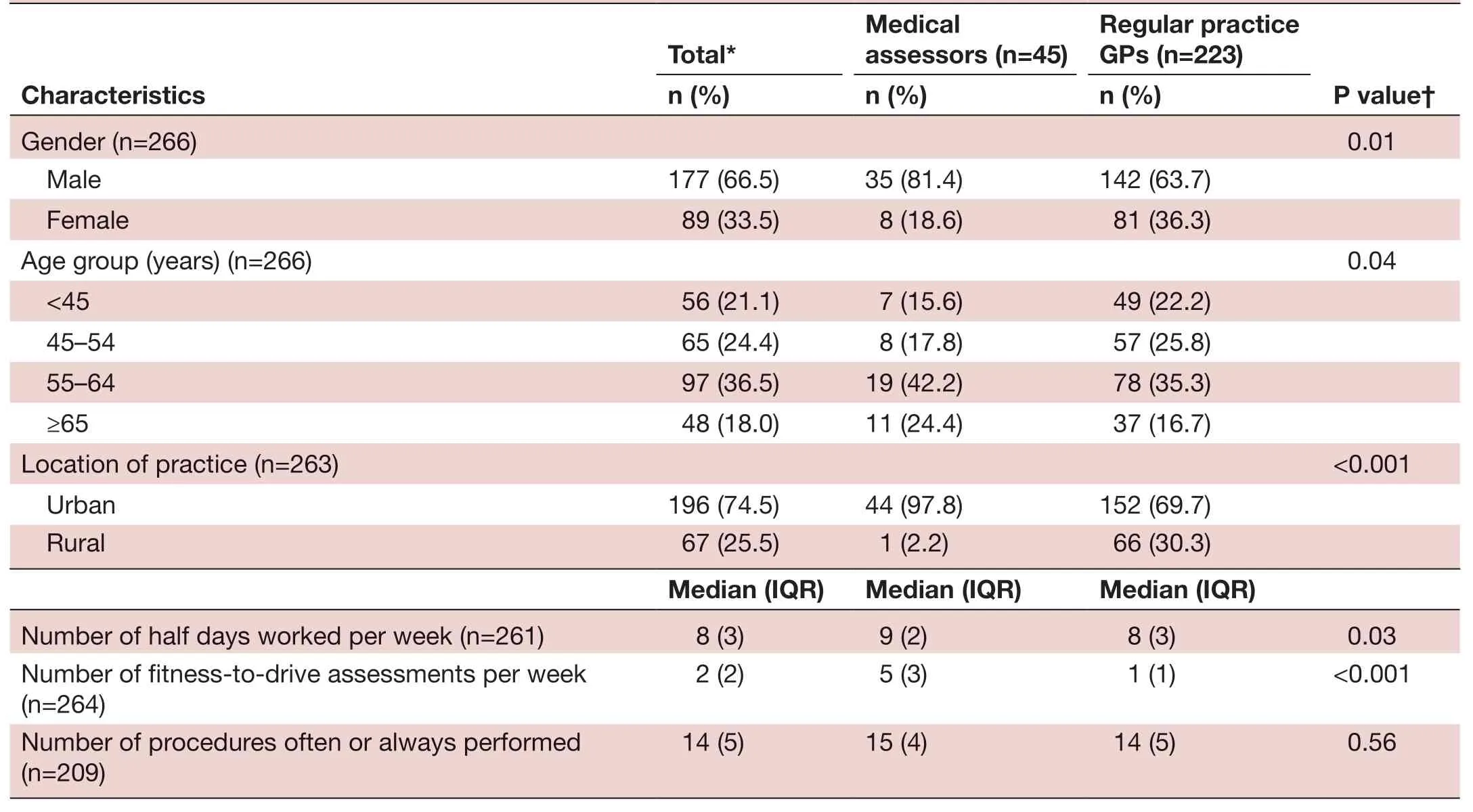
TabIe 2 Physicians’ characteristics, overall, and stratified into two groups according to whether they are medical assessors of the road traffic office or regular practice GPs (n=268)
Statistical significance was set at a two- sided p value ≤0.05. All statistical analyses were carried out with STATA V.12.0 (College Station, USA).
RESULTS
Study population
Two hundred and sixty- eight physicians (47%) agreed to participate in the study (medical assessors: 45, regular practice GPs: 223). Table 2 presents their main characteristics. The majority of participants were male (67%) and practising in urban areas (75%); they were rather experienced physicians (more than half of them were older than 55 years). The median number of assessments carried out was 2 per week, 14% of physicians performing less than one assessment, 36% one assessment, 21% two assessments and 29% more than two assessments per week. Finally, the median number of procedures physicians often or always performed was 14. Compared with regular practice GPs, those practising as medical assessors were more often male, slightly older and practising more often in urban areas. In addition, the median number of assessments per week was five times higher for medical assessors than for regular practice GPs (median: 5 vs 1). Our sample of physicians (medical assessors excluded) appear to be representative of all physicians practising in Switzerland in terms of age (median age: 54 years in Switzerland vs 57 years in our study), but slightly less in terms of gender distribution (men: 59% in Switzerland vs 64% in our study).15
Perceived usefulness of the preconsultation patient questionnaire
Overall, three- quarters of physicians judged that the preconsultation patient questionnaire would be very (43%) or somewhat useful (32%) to guide their assessments (table 3). There were no statistically significant differences between physicians’ subgroups, although older physicians tended to consider the questionnaire less useful.
Perceived usefulness of the reference guide
The majority of physicians also judged that the reference guide would be very (62%) or somewhat useful (27%). As shown in table 3, in univariate analysis, medical specialty and age were statistically significantly associated with the perceived usefulness of the guide, with medical assessors and older physicians finding the reference guide less useful (both p values 0.03). In multivariable analysis, these associations were not statistically significant.
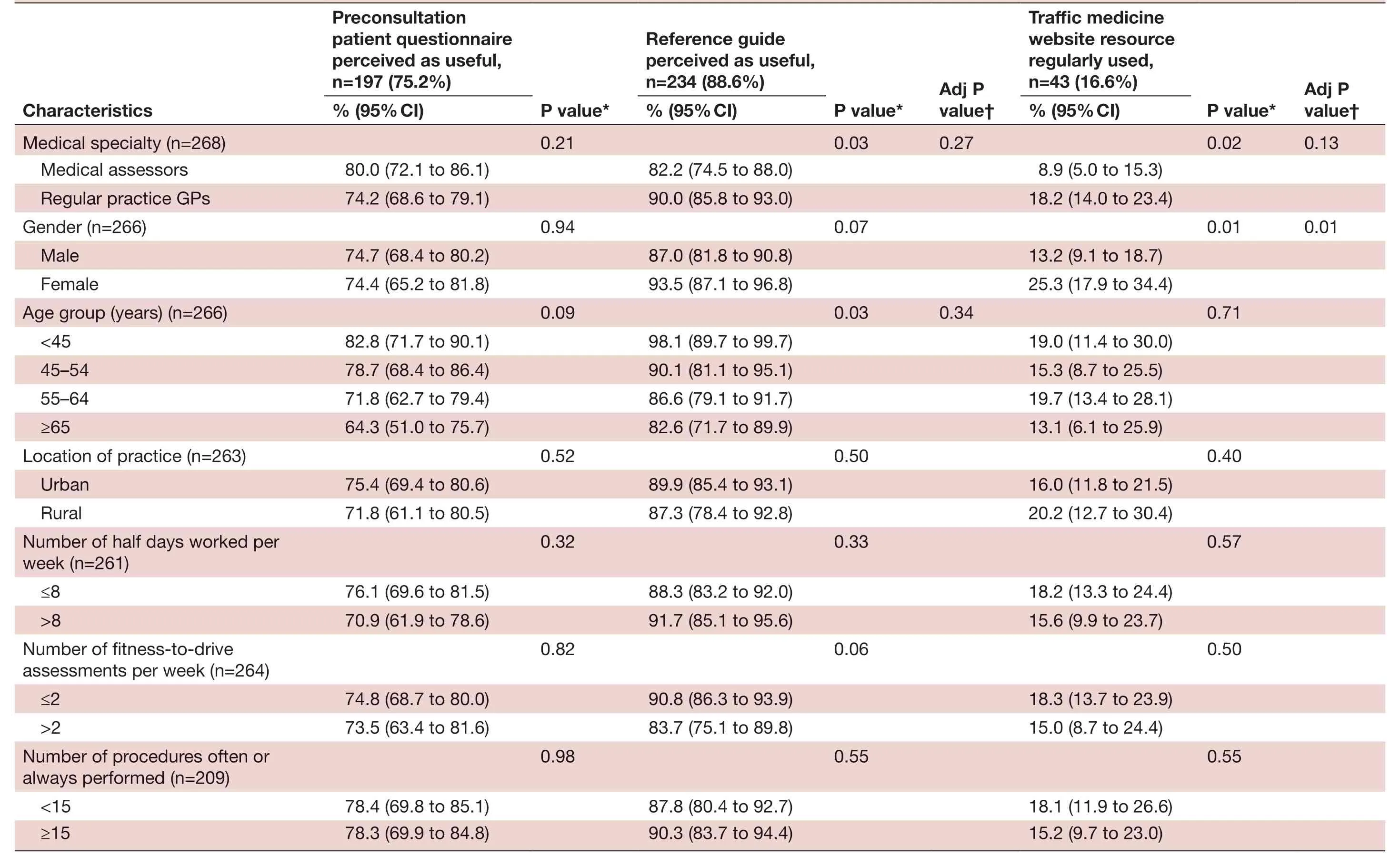
TabIe 3 Perceived usefulness for physicians of a standardised questionnaire completed by the drivers (preconsultation patient questionnaire) and a reference guide to help physicians during the fitness- to- drive assessment, as well as frequency of use of the information sources provided by the traffic medicine website, stratified by physicians’ characteristics (n=268)
Use of the information sources provided by the traffic medicine website
Overall, only a minority of physicians (17%) regularly used these information sources (table 3). Almost one- third of physicians (31%) have never used them (data not shown in the table). In univariate analysis, medical specialty (regular practice GPs) and gender (female) were statistically significantly associated with regular use of the website resource. The association with gender (but not with medical specialty) was statistically significant in multivariable analysis, with female physicians being more likely to use these information sources than their male counterparts (adjusted OR 2.9 (95% CI 1.3 to 6.1), p=0.01).
DISCUSSION
Main finding
We found that the median number of fitness- to- drive assessments carried out by our sample of physicians was 2 per week. We also found that the majority of physicians considered that a self- administered questionnaire completed by older drivers before the consultation and a reference guide summarising the Swiss recommendations on the fitness- to- drive assessment of older drivers would be very/somewhat useful. However, less than one- fifth of them always/often used the information sources provided by the traffic medicine website. Finally, there were no statistically significant associations between the medical specialty (medical assessors or GPs) and the perceived usefulness of the preconsultation patient questionnaire and reference guide and the frequency of use of the traffic medicine website.
Comparison with the existing literature
The finding that the preconsultation patient questionnaire and the reference guide were considered useful could be explained in two ways. First, physicians may feel that they are not sufficiently trained and/or do not have the required competences to carry out the fitness- to- drive assessments. These two practical tools could help to reassure them, and, as such, they could be used as a model to guide these assessments. This assertion would be in line with previous research; for example, a survey carried out in Canada (n=460 GPs) showed that nearly half of GPs did not feel comfortable in assessing older drivers and the majority of GPs (89%) were interested in receiving more training in this area.12Another study carried out in Sweden and Finland (n=1682 GPs) showed that only 21% of Finnish and 18% of Swedish GPs felt that their training in traffic medicine was sufficient for assessing the driving fitness of older drivers.16Second, the preconsultation patient questionnaire could offer time- saving benefits for physicians, in that it could be completed at home or in the waiting room, and, as such, the collection by physicians of relevant medical information during the medical visit could be carried out more quickly.
We also found that younger physicians were generally more likely to consider both of these practical tools useful, although the association with age was not statistically significant in multivariable analysis. This finding could be explained by the fact that younger physicians are less experienced physicians and are generally more in need of tools to improve their skills in this area. For example, several authors have shown that younger physicians tend to have higher adherence to guidelines than their older, more experienced counterparts.17-19In England, a study showed that a 10- year increase in age was associated with halving odds of using elective surgical referral guidelines.19
Interestingly, the proportion of physicians in our study who found the instruments useful was not dependent on their medical specialty (medical assessors or regular practice GPs), nor did the results vary with the number of assessments performed per week or with the level of adherence to Swiss guidelines (estimated by the number of recommended procedures performed by physicians during the fitness- to- drive assessments: ≥15 vs <15 procedures). Note that an in- depth discussion on this topic (level of adherence to Swiss guidelines) can be found in the practice review.11
Surprisingly, although the majority of physicians found these instruments useful, less than one- fifth of physicians regularly used the information sources provided by the Swiss traffic medicine website. They were however gender effects with female physicians using the traffic medicine website resource a little more than their male counterparts: 25% vs 13% for male physicians. In addition, almost one- third of physicians have never used them, perhaps because they were unfamiliar with them. This would be in line with two American studies showing that physicians were not aware of existing fitness- to- drive assessment guidelines.1213These findings suggest that physicians assessing the fitness to drive of older patients should be more aware of available sources of information, particularly male physicians. Regular training of physicians, which is currently not the case in our country, would be an ideal opportunity to assess their knowledge and provide them with the necessary information on available medical resources. It should be noted, however, that the information available to physicians to help them assess older drivers, in particular the Swiss recommendations, is not evidence- based but only expert opinions.
Perspectives
The implementation of a preconsultation patient questionnaire, ideally in both paper and online formats, would be in line with the general trend towards the development and promotion of self- assessment instruments that favour self- regulation and support the transition to driving cessation.2021Thus, the preconsultation patient questionnaire could be regularly completed by older drivers at home and provide an opportunity for feedback and increased awareness of their fitness to drive, for example, by asking them to self- report health concerns.2021However, patients’ perceptions of driving ability and actual driving ability may differ significantly, and many older drivers with medical conditions do not appropriately self- regulate their driving (especially those with dementia).22For this reason, evidence- based assessments of fitness to drive can assist physicians in determining the driving ability of patients who are medically impaired.
Limitations
First, only physicians practising in Western Switzerland were included in the study; these physicians are not necessarily representative of all physicians practising in Switzerland. Second, the study data were based on the answers to a self- administered questionnaire and therefore are subject to self- report bias. Third, we did not record any data on physicians who declined to participate in the study. Finally, this study assessed the perceived usefulness of practical tools (preconsultation patient questionnaire and reference guide) and the use of the traffic medicine website. It would also have been useful to examine whether these resources actually have an effect on how physicians assess older drivers, their knowledge and their confidence in fitness- to- drive assessments.
CONCLUSIONS
Many physicians in this study found the preconsultation patient questionnaire and reference guide useful to guide them for assessing the driving ability of older drivers, but only a minority regularly used the information sources provided by the traffic medicine website. Future studies should explore the reasons why many physicians do not use available sources of information. In addition, further research is needed to find out what older drivers and drivers’ associations think about the use of these practical tools.
Correction noticeThis article has been corrected since it was published Online First. A typo has been fixed in the abstract.
AcknowledgementsPS would like to warmly thank all the doctors who participated in the study, Amir Moussa, our research assistant, and Dagmar Haller, Philippe Huber, Yolanda Mueller and Leonardo Silvestri for their support and assistance throughout the study.
ContributorsPS was involved in the conception, data analysis and data interpretation. PS drafted the first version of the manuscript. PS can be contacted for access to the data set underlying the current analysis.
FundingThis project was supported by institutional funding from the Faculty of Medicine, University of Geneva.
DisclaimerThe funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interestsNone declared.
Patient consent for publicationNot required.
Provenance and peer reviewNot commissioned; externally peer reviewed.
Data availability statementData are available upon request.
Open accessThis is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY- NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non- commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non- commercial. See: http:// creativecommons. org/ licenses/ by- nc/ 4. 0/.
ORCID iD
Paul Sebo http:// orcid. org/ 0000- 0001- 7616- 0017
 Family Medicine and Community Health2020年3期
Family Medicine and Community Health2020年3期
- Family Medicine and Community Health的其它文章
- The day the residents left: lessons learnt from COVID-19 for ambulatory clinics
- Enhancing your scholarship as a family medicine junior faculty member
- Associations between concussion and risk of diagnosis of psychological and neurological disorders: a retrospective population- based cohort study
- GP prescribing in Northern Ireland by deprivation index: retrospective analysis
- Postgraduate education among family and community physicians in Brazil: the Trajetórias MFC project
- Telemedicine, the current COVID-19 pandemic and the future: a narrative review and perspectives moving forward in the USA
