Clinical observation on heat-sensitive moxibustion plus lactulose for postoperative constipation of mixed hemorrhoid due to spleen deficiency
Dong Fen-fen (董芬芬), Ying Jian (應健)
Yuhuan Hospital of Traditional Chinese Medicine, Zhejiang 317600,China
Abstract
Keywords:MoxibustionTherapy;Heat-sensitiveMoxibustion;MoxaStick Moxibustion;Point,Shenque(CV 8);Hemorrhoids;Constipation; PostoperativeComplications;Randomized ControlledTrial
Mixed hemorrhoid is a common protological problem withahighandrisingincidencerate[1].Common conservative treatments such as local or oral administrationof medicationaretargetedat alleviating symptoms, while surgery is needed in some severe cases or for serious complications[2].Constipation is a common complication after surgery. It can cause adverse effects including delaying the wound healing,inducing or increasing cutpainand inflammation[3]. Therefore, it’s of great importance to searchatimely andeffectivetreatmentfor postoperativeconstipation.Despitethevarieties of medications for postoperative constipation, they fail to achieve satisfactory results. As an important component of traditional Chinese medicine (TCM), moxibustion has beenlong usedfor treatingconstipationand post-operative rehabilitation[4-5]. We used heat-sensitive moxibustioncombining lactuloseoralliquidto treat postoperativeconstipationof mixedhemorrhoidand compared it with administration of lactulose oral liquid alone to observe its clinical effect. The report is now given as follows.
1 Clinical Materials
1.1 Diagnostic criteria of Western medicine
1.1.1 Diagnostic criteria of mixed hemorrhoid[6]
Blood in stool or anal lump,may be accompanied withdistention,foreignbody sensationor painin surrounding area, or local secretion and itching; lump passes throughdentalline andparallel to anal tube(may appear as skin tag or varicosity under dental line);diagnosedby analinspectionor endoscopy examination.
1.1.2 Diagnostic criteria of constipation[7]
Feeling exertion during at least 25% defecation; lump or hard stool during at least 25% defecation; endless feeling during at least 25% defecation; feeling anal or rectumobstructionduring at least 25% defecation;require manualassistanceduring at least 25%defecation; less than 3 times of defecation in a week.Meeting 2 of the above 6 items, rare loose stool unless using laxatives, and without a clear diagnosis of irritable bowel syndrome, can be diagnosed as constipation.
1.2 TCM pattern differentiation criteria
Conforming to the pattern differentiation criteria of spleendeficiency[8].Mainsymptoms:thoughhaving intentionto defecate,feelingexertionwhenpassing stool, together with symptoms including sweating and shortness of breath, and feeling fatigue after defecation.Secondary symptoms: with a pale complexion, fatigue,shortness of breath, a pale tongue with thin and white coating, and a weak pulse.
1.3 Inclusion criteria
Conforming totheWesternmedicine diagnostic criteriaof mixedhemorrhoidandconstipation;conforming to the TCM pattern differentiation criteria of spleen deficiency; aged between 18 and 60 years,receivedmixedhemorrhoidsurgery within2weeks;without defecationabnormity beforesurgery;good compliance, cooperative to examinations in this study;informed consented.
1.4 Exclusion criteria
Having constipation before surgery; accompanied by irritablebowelsyndrome,boweltumor or other intestinaldiseases;womenduring pregnancy or lactation; having serious heart, brain or kidney diseases;showing noheat-sensitivephenomenonduring moxibustion treatment.
1.5 Rejection and dropout criteria
Those with serious adverse event; poor compliance,used other medication treatment without supervision;initiatively quitting the experiment; insufficient clinical data that may influence clinical efficacy evaluation.
1.6 Statistical methods
TheSPSS version20.0 softwarewas usedfor statistical analysis.Enumerationdata were compared usingχ2test. Measurement data conforming to normal distributionwere describedasmean± standard deviation(±s).Thepairedsamplet-test was for intra-groupcomparisons,andindependent samplet-test for between-group comparisons. Non-parametric testwasfor comparing data that didn’t conform to normaldistribution.AP-valueless than0.05was considered statistical significance.
1.7 General data
All cases were recruited between January 2017 and May 2018in YuhuanHospitalof TraditionalChinese Medicine.All70 patients withmixedhemorrhoid postoperativeconstipationwererandomizedinto a treatment groupandacontrolgroupby arandom number tableaccording totheir visiting sequence.There was no dropout case during the whole treatment period. Between-group comparisons of the gender, age anddurationshowednostatisticalsignificance(allP>0.05), indicating the comparability (Table 1).
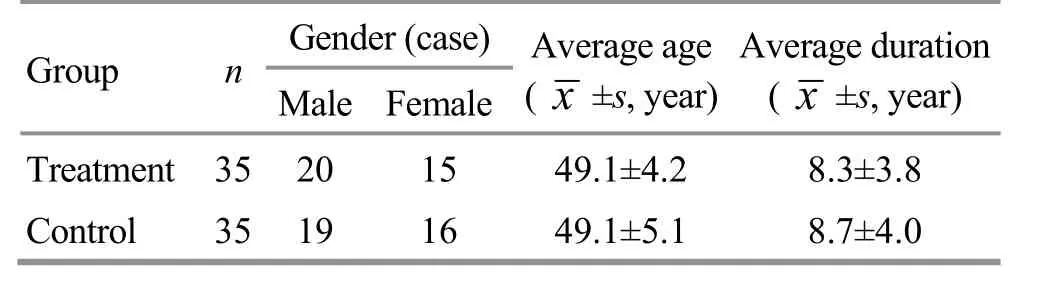
Table 1.Comparison of the general data between the two groups
2 Treatment Methods
2.1 Control group
Patients in the control group received lactulose oral liquid(ChinaFood andDrug Administration approval number: H20171057, Abbott Healthcare Products B.V.,Holland),15mL every time,twice aday for 15 consecutive day.
2.2 Treatment group
Patientsinthetreatment groupreceivedheatsensitivemoxibustiontreatment basedonlactulose treatment (same usage and dosage as in the control group).
Point: Shenque (CV 8).
Methods: Hwato brand moxa stick (Nanyang Wolong HanyiMoxibustionFactory,China)was usedfor moxibustion. Patients took a supine position, with the exposureof Shenque(CV 8).Practitioner performed heat-sensitivemoxibustiontreatment as recordedin theAcupoint Heat-sensitizationMoxibustion:ANew MoxibustionTherapy[9].Firstly,detectedtheheat- sensitive point. Took circling or mild moxibustion with a moxastick near Shenque(CV 8),keeping a3-5cm distance between the ignited moxa stick and the skin.Whenpatients hadaheat-sensitive feeling of heat penetrationor spreading or conduction,or distal radiation heat or non-heat sensation, such location was consideredheat-sensitivepoint.Secondly,continued mildmoxibustionat heat-sensitivepoint,untilheat- sensitive phenomenon disappeared (15-20 min). Took moxibustion treatment once a day for consecutive 15 d.
3 Therapeutic Efficacy Observation
3.1 Observation items
3.1.1 The stool form score, defecation interval time and defecation duration
The stool form score, defecation interval time and defecationduration weremeasuredbefore and after treatment. The scoring criteria of stool form: sausage- shaped stool, soft, lumpy or liquid stool were scored 0 point; sausage-shaped stool with cracked surface were scored1point;sausage-shaped,lumpy stoolwere scored 2 points; hard, nut-like stool lumps were scored 3 points[10].
3.1.2 Defecation pain severity
Thevisualanalog scale(VAS)score wasusedfor evaluating pain severity during defecation. VAS ranged from 0 to 10 points, in which 0 point indicated no pain,and 10 points indicated unbearable pain[11]. Took a ruler of 10 cm mark in front of the patients, and let them point theproper number to representtheir pain severity. The recorded number was the VAS score.
3.1.3 Patient assessment of constipation quality of life questionnaire (PAC-QOL) score
The PAC-QOL was used for evaluating the quality of life(QOL)of the patient.PAC-QOL indicatedthe influence of constipation on patients’ daily life in the past two weeks. A higher score indicated worse QOL[12].3.1.4 Laboratory examination
The morning fasting venous blood was drawn before andafter treatment.Took enzyme-linked immunosorbent assay (ELISA) technique to analyze the serum substance P (SP) and nitric oxide (NO) levels.
3.2 Results
3.2.1 Comparisons of the stool form score, defecation interval time and defecation duration
Beforetreatment,between-groupcomparisons of thestoolformscore,defecationintervaltime and defecation duration showedno statistical significance(allP>0.05).After treatment,the stoolformscore,defecation interval time and defecation duration in both groups alldroppedsignificantly (allP<0.05),and the stoolformscore,defecationintervaltimeand defecationdurationin the treatment group wereall lower thanthoseinthecontrolgroup(allP<0.05),(Table 2).
Table 2.Comparisonsof thestool formscore,defecationinterval time and defecationduration( ±s)

Table 2.Comparisonsof thestool formscore,defecationinterval time and defecationduration( ±s)
Note: Intra-group comparison,1) P<0.05; between-group comparison, 2) P<0.05
GroupnTime Stool form score(point)Defecation interval time (d)Defecation duration (min)Treatment 35Beforetreatment 1.77±0.734.77±1.1123.40±3.70 After treatment 0.83±0.751)2)2.11±0.751)2) 14.46±3.531)2) Control 35Beforetreatment 1.91±0.784.60±1.0923.29±3.84 After treatment 1.48±0.511)2.88±0.801)20.45±3.111)
3.2.2Comparisonof theVASscore
Before treatment, between-group comparison of the VAS score showedno statistical significance (P>0.05).After treatment, the VAS scores in both groups dropped significantly (bothP<0.05), and the VAS scorein the treatment group was significantly lower than that in the control group (P<0.05), (Table 3).
3.2.3Comparisonof thePAC-QOL score
Before treatment, between-group comparison of the PAC-QOL score showednostatisticalsignificance(P>0.05). After treatment, the PAC-QOL scores in both groupsdroppedsignificantly (bothP<0.05),andthe PAC-QOL score in the treatment group was significantly lower than that in the control group (P<0.05), (Table 4).
Table 3.Comparisonof the VASscore( ±s, point)

Table 3.Comparisonof the VASscore( ±s, point)
Note:Intra-groupcomparison,1)P<0.05;between-group comparison, 2) P<0.05
GroupnTime VAS Treatment 35Beforetreatment 5.44±0.84 After treatment 1.62±0.831)2)Control 35Beforetreatment 5.82±0.89 After treatment 2.43±0.881)
Table 4.Comparison of the PAC-QOL score( ±s,point)

Table 4.Comparison of the PAC-QOL score( ±s,point)
Note:Intra-groupcomparison,1)P<0.05;between-group comparison, 2) P<0.05
GroupnTime PAC-QOL Treatment 35Beforetreatment 44.51±2.83 After treatment 25.03±3.071)2)Control 35Beforetreatment 44.94±3.40 After treatment 33.03±4.441)
3.2.4 Comparison of the serum SP and NO levels
Beforetreatment,between-groupcomparisons of theserumSPandNOlevels showednostatistical significance (bothP>0.05). After treatment, the serum SP levels in the two groups increased significantly (bothP<0.05), and the NO levels decreased significantly (bothP<0.05). After treatment, between-group comparisons of serumSP andNOlevelsshowedstatistical significance (bothP<0.05), (Table 5).
Table 5.Comparisonof the serum SP and NOlevels( ±s)
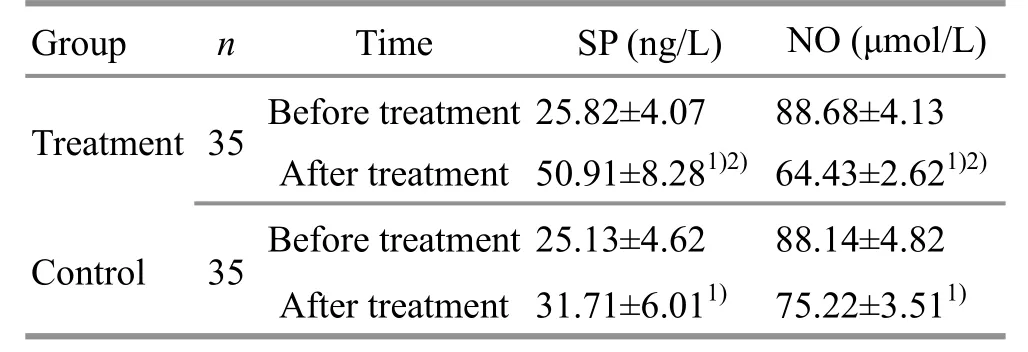
Table 5.Comparisonof the serum SP and NOlevels( ±s)
Note:Intra-groupcomparison,1)P<0.05;between-group comparison, 2) P<0.05
GroupnTime SP (ng/L)NO(μmol/L)Treatment 35Beforetreatment 25.82±4.0788.68±4.13 After treatment 50.91±8.281)2)64.43±2.621)2)Control 35Beforetreatment 25.13±4.6288.14±4.82 After treatment 31.71±6.011) 75.22±3.511)
3.2.5 Comparison of the adverse events
During treatment,2patients inthecontrolgroup showedabdominaldistentionandpain,and1showed nauseaandvomiting.Onecaseinthetreatmentgroup showedabdominaldistentionandpain,and1showed diarrhea.Adverseeventsinthetwogroupswere mild andwerealleviatedina few days. After treatment,the blood,urineandstoolroutinesaswellasliver and kidney functionsinthe two groupsshowednoobvious abnormity.
4 Discussion
Postoperative constipation of mixedhemorrhoidis a commonproblemwithvarious causes.Thefivemain causesincludeusageof anesthetic or painkiller to slow downbowelmovements;changeindietary habit or foodstructure,subjectivediet controlwhichleadsto thereductionof defecation,moreover,reductionof crudefiber intake canalso slow downbowel movements;fear of thecut painwhichdelays patients’defecationroutine,causing stagnationof stoolinthe bowel, and thedeprivationof water willdry thestoolto causedifficulty passing,thus causing constipation;long-termbedrest andphysicalinactivity canslow downbowelmovement;unaccustomedto bedrest defecation,thuslosing desireto defecate[13-14].Ina word, the cause of constipation is complicated, and is generally consideredtobe linkedwithcolorectum mobility disorder,abnormalgastrointestinalreflex,pelvic functional disorder and mental factors[15].
Recent research showed that SP and NO played an important part in constipation. First, SP is an exciting neurotransmitter spreading across bowelmyenteric nerve plexus. Second, SP can stimulate longitudinal and circular muscleof the gastrointestinaltract,and promote bowelmovement.Third,SP canalso bind specific receptor on the cytomembrane, and facilitate excitement conduction among synapses. Fourth, SP will alsostimulateionchannelonthesmoothmuscle surfaceto change their electricalactivity,andthus promote bowel movement. Fifth, SP can interact with mastocyte and increase capillary permeability and gland secretion.Besides,by activating platelet to discharge serotonin, SP can excite gastrointestinal smooth muscle and cholinergic and non-cholinergic neurons, which will adjust intestinaltransmission, andpromote bowel movement and liquid secretion[16-17]. Zhang YX[18]found that serumSPshowedalow levelinconstipation patients.After treatment,SPlevelsobviously rose together with the improvement of defecation hardness and exhaustion. Therefore, a low SP level might be an important cause of constipation. NO is a non-cholinergic inhibitory neurotransmitter indigestivetract.By elevating the cGMP level in gastrointestinal tract, NO canrelax smoothmuscle,decrease gastrointestinal excitement andcontractionfrequency, andinhibit evacuationtoaggravateconstipation[19].Wang JM,et al[20]observed rats of slow transit constipation model,and found after TCM treatment, model rat’s defecation number, water content and intestinalpropulsiverate improved significantly, together with reduction of NO andnitric oxidesynthase(NOS)levels.Therefore,adjustment of NOlevelmay improveconstipation symptoms.
In TCM, constipation is mainly associated with the large intestine, and also related to the spleen, lung, liver andkidney.Themaincauses of constipationare retainedheat inthestomachandintestine,qi stagnation, spleen qi deficiency, spleen yang deficiency,yindeficiency andintestine dryness[8].Postoperative constipation of mixed hemorrhoid is generally caused by qiandbloodlossduring operation,or lossof appetite in the rehabilitation process which can lead to stagnation of qi andblood. Spleen qideficiency is a common pattern, mainly manifested as having intention to defecate, feeling exertion when passing stool, fatigue after defecation,sweating andshortnessof breath.Therefore, the treatment strategies are to tonify spleen qi and lubricate the intestines.
Heat-sensitivemoxibustioncanstimulate points under sensitized state through its warming effect. As a new typeof moxibustiontreatment,itcan transmit stimulationthroughsaturatedmoxibustion[9].Heatsensitive moxibustion has the merits of penetrating and supplementationthroughwarming anddredging,as wellastonifying.Besides,it canalsosupplement healthy qi, warm yang qi, and dredge meridians, which are especially suitable for the treatment of constipation of spleen qi deficiency. We chose Shenque (CV 8) as the heat-sensitive moxibustion point because it’s a crucial point in the Conception Vessel, and can warm spleen yang and harmonize gastrointestinal function. Applying saturated heat-sensitive moxibustion to Shenque (CV 8)can maximize its advantages of supplementing spleen qi,warming and unblocking qi movement and regulating Zang-fu organs.
Our research showed that after treatment, the stool form score, defecation interval time and duration time in the two groups all decreased significantly (allP<0.05).Thestoolformscore,defecationintervaltimeand duration time in the treatment group were significantly lower than those in the control group (allP<0.05). The VAS scoresinthetwogroupsdroppedsignificantly (bothP<0.05),andtheVAS score inthetreatment group was significantly lower than that in the control group (P<0.05). The PAC-QOL scores in the two groups dropped significantly (bothP<0.05), and the PAC-QOL scorein the treatment group was significantly lower than that in the control group (P<0.05). The serum SP levels in the two groups increased, and the NO levels in the two groups decreased significantly (allP<0.05). And,the between-groupcomparisonsof theNOandSP levels showedstatisticalsignificance(bothP<0.05).Therefore, heat-sensitive moxibustion plus lactulose can improve stool form score, shorten defecation interval and defecation duration time, and alleviate defecation pain, improve QOL in patients with mixed hemorrhoid postoperative constipation, which may relate with the adjustment of serum SP and NO levels. The result of our study was still limited by a small sample size and lack of along-term follow-up visit. Thus, a study of a larger sample size and longer investigation term is needed in the future to provide more evidence for this treatment.
Conflict of Interest The authorsdeclare that there isnoconflict of interest in thisarticle.Statement of Informed Consent Informed consent wasobtained from all individual participants.
Received:19September 2019/Accepted:24October 2019
 Journal of Acupuncture and Tuina Science2020年3期
Journal of Acupuncture and Tuina Science2020年3期
- Journal of Acupuncture and Tuina Science的其它文章
- Therapeutic observation on lung-clearing and spleen-strengthening tuina in children with exogenous cough
- Therapeutic efficacy observation on auricular point sticking therapy for cardiac syndrome X in women
- Effects of electroacupuncture plus drug anesthesia on pain and stress response in patients after radical surgery for stomach cancer
- Therapeutic effect of heat-sensitive moxibustion plus medications for senile osteoporosis and its effect on serum BMP-2 and OPG levels
- Efficacy of transcutaneous electrical acupoint stimulation (TEAS) for menopausal insomnia and its effect on serum hormone levels
- Therapeutic observation of manipulation plus exercise therapy in treating upper crossed syndrome postures of primary school students
