Subcutaneous Panniculitis-Like T-Cell Lymphoma: A Case Report
Bai-He Wang, Xiu-Lian Xu, Jian-Fang Sun?
Department of Pathology, Hospital for Skin Diseases (Institute of Dermatology), Chinese Academy of Medical Sciences and Peking Union Medical College, Nanjing, Jiangsu 210042, China.
Introductio n
Subcutaneous panniculitis-like T-cell lymphoma (SPTCL)is a rare cytotoxic T-cell lymphoma that accounts for less than 1% of all peripheral T-cell lymphomas. SPTCL is characterized by multiple subcutaneous nodules or plaques that occur in the extremities, and it has a poor prognosis if accompanied by hemophagocytic syndrome.The histopathological findings and immunophenotype of SPTCL are specific and can help to confirm the diagnosis.We herein report such a rare case involving a woman with a single facial lesion.
Case report
A 33-year-old woman presented with a two-month history of swelling on her right upper eyelid.The lesion began to appear red and swollen without pruritus, pain, and other discomfort, and persisted and expanded to involve the entire eyelid.Several miliary-sized papules were felt in the subcutaneous tissue. The texture of the lesion was tough,and its mobility was poor (Fig. 1A).
Physical examination of the cardiopulmonary system and abdomen showed no abnormalities, and no swelling was found in the superficial lymph nodes.Since symptom onset,the patient had developed no fever or night sweats,her diet and sleep were unaffected, and she had experienced no significant change in body weight.Histopathological examination of the facial lesion showed excessive epidermal reticular keratinization, focal liquefaction of basal cells, infiltration of lymphocytes mainly around dermal blood vessels and appendages, and infiltration of large lymphocytes in subcutaneous fat lobules. The cells were heterogeneous and varied in size(Fig. 2A and 2B). Immunohistochemical examination(Fig. 2C-2H) revealed the following: CD3 (+++), CD2(+++),CD5(+++),CD20(×),CD30(×),T-cell intracellular antigen-1 (++), CD79a (×), CD56 (×), Ki67-positive cells (approximately 25%), Epstein-Barr virus-encoded small RNA (×), CD4 (×), and CD8 (++). Blood tests revealed no evidence of hemophagocytic syndrome.
SPTCL was definitively diagnosed. The patient was treated with prednisone 20 mg per day,methotrexate 5 mg twice a week,and interferon-a at a dose of 3 million units by intramuscular injection twice a week. After two months, the patient’s skin lesion had almost completely subsided (Fig. 1B).
Discussion
SPTCL is a cytotoxic T-cell lymphoma that accounts for less than 1% of all peripheral T-cell lymphomas.1The WHO-EORTC classification defines SPTCL as a tumor that expresses an a/b T-cell receptor (TCR) gene rearrangement.Tumors expressing g/d TCR are classified as primary cutaneous g/d T-cell lymphomas.
The incidence of SPTCL is low, and both children and adults may be affected.The median age at diagnosis is 46.5 years, and about 20% of patients are younger than 20 years.1-2SPTCL generally manifests as one or more painless subcutaneous nodules or indefinite firm plaques that can affect the legs(71%),arms(62%),torso(56%),and/or face(25%).1,3The diameter of the nodules varies from 0.5cm to 20 cm. Necrosis may occur, and ulceration rarely occurs(6%). A single lesion is rare, and approximately 80% of patients have multiple nodules and/or plaques.The disease isoftenaccompaniedbyfever,nightsweats,weightloss,and bone marrow abnormalities. The most common bone marrow abnormality is hemophagocytic syndrome,which is often associated with the prognosis of the disease. A literature review of 16 Japanese with SPTCL showed a higher incidence of B symptoms (81%) and hemophagocyticsyndrome(45%)andalowerincidenceofautoimmune disease(13%).4
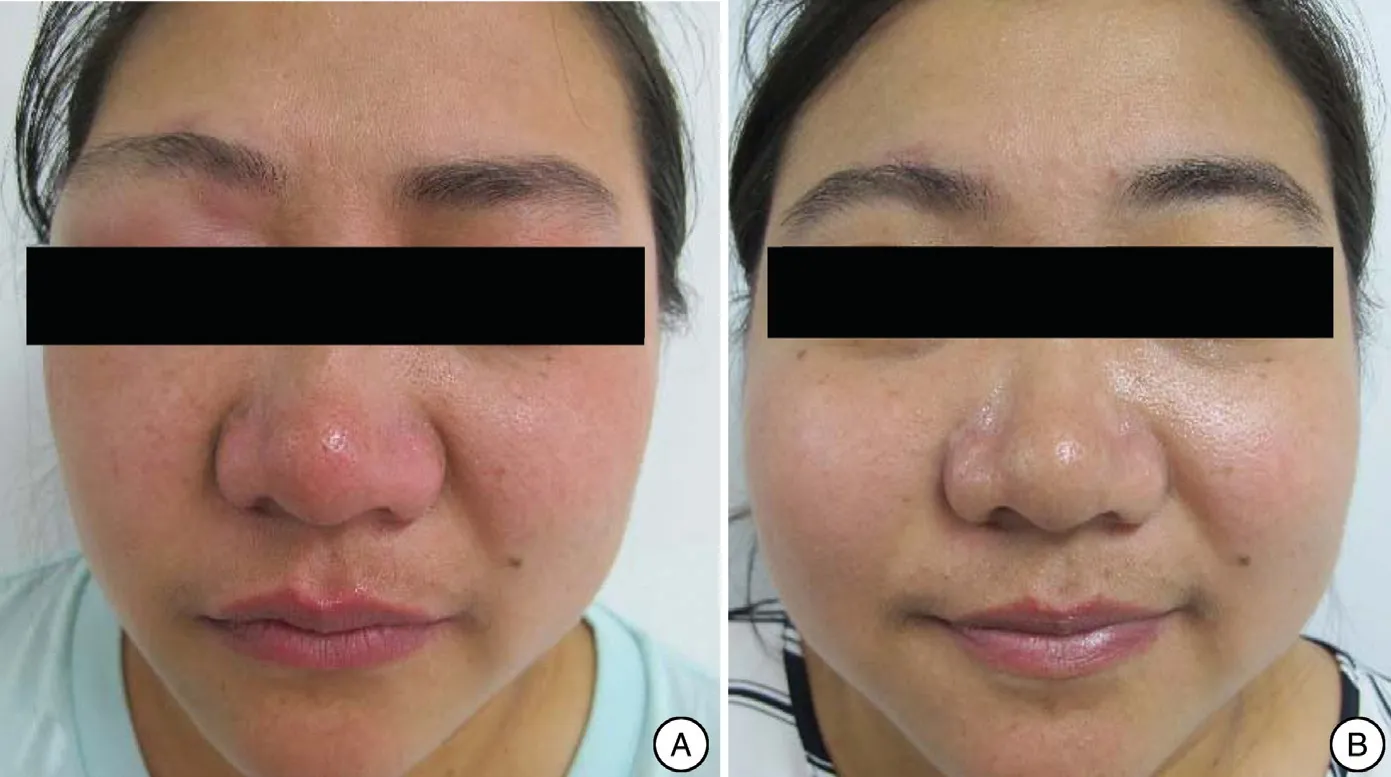
Figure 1. Skin manifestations before and after treatment. (A) Red and swollen upper right eyelid with several miliary-sized papules in the subcutaneous tissue before treatment. (B) The patient’s facial skin lesions had almost completely subsided after treatment.
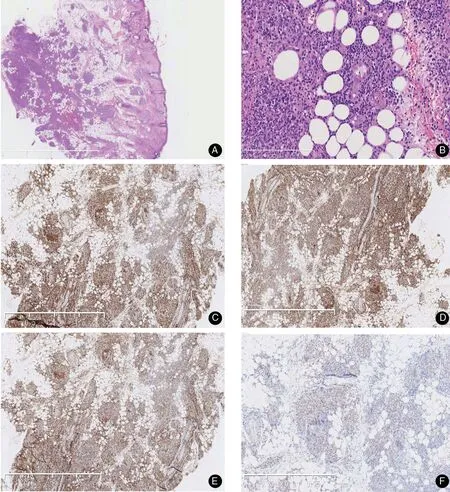
Figure 2. Histopathological(A and B)andhistochemical(C–F)results ofthelesion.(A)Epidermalreticular keratosis,focalbasal cell liquefaction,and a tumornodulelocated inthesubcutaneoustissue(H&E,×40).(B)Infiltrationofsmallfocallymphocytesaroundthedermal vessels and appendages and large lymphocytes in the subcutaneous fat lobules.The cells were heterogeneous and varied in size(H&E,×200).(C)CD2 positive(×400).(D)CD3 positive(×400).(E)CD5 positive(×400).(F)TIA-1 positive(×400).(G)Ki-67 in approximately 25%of cells(×400).(H)CD8 positive(×400).
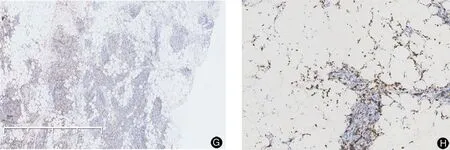
Figure 2. (Continued).
The histology of the disease is characterized by infiltration of pleomorphic malignant T cells in the subcutaneous adipose tissue accompanied by a large number of macrophages. The epidermis and dermis are generally normal, and the arrangement of malignant T cells around a single fat cell is helpful for the diagnosis.Immunohistochemically,most cases of SPTCL are positive for TCR-a/b, CD3, CD8, and cytotoxic proteins, while CD4 is negative.A few CD30-positive and CD56-positive cases have been reported. The diagnosis of SPTCL is relatively difficult because its clinical manifestations are similar to those of some cases of lupus erythematosus patients, and they often occur simultaneously.5The final diagnosis is based on a combination of the patient’s skin histopathological manifestations,immunophenotype,and clinical features.
SPTCL must be differentiated from the following diseases. (1) Primary skin g/d T-cell lymphoma: This disease often involves the dermis and epidermis,and leads to epidermal ulcers. The immunophenotype is similar to that of SPTCL, but this lymphoma simultaneously expresses CD56 and TCRg. In contrast, SPTCL has a better prognosis. (2) Extranodal NK/T-cell lymphoma:This is a peripheral T-cell lymphoma of a natural killer cell line or a T-cell line.It is associated with Epstein–Barr virus infection and usually manifests as mass on the face. The disease can sometimes affect the skin, but it is never restricted to the subcutaneous tissue. Its immunophenotype is similar to that of SPTCL,but it is negative for CD8 and positive for CD56, is often associated with Epstein–Barr virus infection, and is negative for TCR gene rearrangement. (3) Benign panniculitis: This is a group of diseases characterized by inflammation involving the subcutaneous fat.The clinical manifestations are similar to those of SPTCL, but histopathological examination does not show abnormal cells. Additionally, clonal TCR gene rearrangement is lacking.(4)Primary cutaneous degenerative large cell lymphoma: This is a peripheral T-cell lymphoma characterized by diffuse infiltration of large lymphoid cells in the superficial and deep dermis and subcutaneous tissue. Similar to SPTCL, it shows positive immunohistochemical staining for CD3 and expression of cytotoxic molecules (T-cell intracellular antigen-1, granzyme B,and/or perforin),but it is also positive for CD30 and CD4. TCR gene rearrangement is positive.
Most patients with SPTCL have a slow disease course and recurrent episodes of skin lesions. The overall fiveyear survival rate is about 80%, and occasionally the lesions spontaneously resolve. Multidrug combination chemotherapy is no longer the first-line treatment for this disease;however,immunosuppressive agents can result in complete cure in patients with SPTCL, especially those with a history of chemotherapy.2,6–8Sustained low-dose hormones are also necessary during the remission period.6
Acknowledgement
This work was supported by the CAMS Innovation Fund for Medical Sciences (No. CIFMS-2017-I2M-1-107).
- 國(guó)際皮膚性病學(xué)雜志的其它文章
- Blastic Plasmacytoid Dendritic Cell Neoplasm:A Case Report
- Spitz Nevus with Specific Dermoscopic Features
- Cutaneous Rosai–Dorfman Disease Presenting with Multiple Nodules on the Thighs and Buttocks
- Oculocutaneous Albinism with Squamous Cell Carcinoma, Bowen’s Disease and Actinic Keratosis: A Case Report
- Successful Treatment of Synovitis, Acne,Pustulosis, Hyperostosis and Osteitis Syndrome with Thalidomide: A Case Report
- Characteristics of Cutaneous and Subcutaneous Infectious Granuloma at a Signal Center in China:A Five-Year Retrospective Study