Effect of warm bladder irrigation fluid for benign prostatic hyperplasia patients on perioperative hypothermia, blood loss and shiver: A meta-analysis
Jie Co , Xi Sheng , Yn Ding , Lingjun Zhng *,Xioying Lu *
a Department of Urology, Changhai Hospital, Second Military Medical University, Shanghai, China
b Department of Robotic Urology Operating Theatre, Changhai Hospital, Second Military Medical University, Shanghai, China
c Nursing Department, Changhai Hospital, Second Military Medical University, Shanghai, China
KEYWORDS Irrigation fluid;Temperature;Bladder fluid;Benign prostatic hyperplasia;Hypothermia;Blood loss;Shiver
Abstract Objective: To find out whether warm bladder irrigation fluid can decrease the occurrence of perioperative hypothermia,blood loss and shiver in patients treated with benign prostatic hyperplasia (BPH).Method: A comprehensive literature review and meta-analysis that included randomized controlled trials (RCTs) related to temperature of irrigation fluid in the perioperative treatment for BPH was taken by researchers.The relevant literature were searched in Chinese database, such as Retrieval Chinese Journal Full-text Database, VIP Journal Database, Wanfang database, as well as in English search engine and database, including Embase, Cochrane and Medline till January 2018.The study quality was assessed by recommended standards from Cochrane Handbook (version 5.1.0).Results: A total of 28 RCTs and 3858 patients were included. The results showed that the incidences of shiver (risk ratio [RR] = 0.32, 95% confidence interval [CI]: 0.28-0.36,p <0.001, I2 = 0%) and hypothermia (RR = 0.36, 95% CI: 0.21-0.59, p <0.001, I2 = 67%)in the group of warm irrigation fluid were lower than the group having room-temperature fluid.Room-temperature irrigation fluid group caused a greater drop in body temperature compared to warm irrigation fluid group(p <0.001,I2=96%).We performed a narrative descriptive statistics only because of substantial heterogeneity.Conclusions: Warm bladder irrigation fluid can decrease the drop of body temperature and the incidence of hypothermia and shiver during and after the operation for BPH. Warm irrigation fluid should be considered as a standard practice in BPH surgeries.
1. Introduction
Benign prostatic hyperplasia (BPH) is a common disease in elderly male that may cause bothersome lower urinary tract symptoms.There are a number of surgical options for BPH patients, i.e., transurethral resection of the prostate(TURP), transurethral plasmakinetic resection of the prostate (TURPK), holmium laser enucleation of the prostate(HoLEP), or transurethral plasmakinetic vaporization prostatectomy (TUPKVP), all of which require intra- and postoperative continuous bladder irrigation to prevent blood clot formation and catheter associated urinary tract infection. The low temperature of the irrigation fluid may result in hypothermia, blood loss and shiver, which may influence the effect of surgery and prolong the length of hospital stay [1]. In this paper, we used the method of meta-analysis to include related randomized controlled trials (RCTs), and evaluate the influence of warm irrigation fluid on the patients’ body temperature, blood loss and shiver.
2. Materials and methods
2.1. Study type
All the RCTs articles related to the effect of warm bladder irrigation fluid for BPH patients on the occurrence of intra- and postoperative hypothermia, blood loss and shivering.
2.2. Subject
BPH patients who received bladder irrigation during TURP,TURPK, HoLEP, or TUPKVP were included in the present study.
2.3. Literature review strategy
The relevant literature were searched in Chinese database including Retrieval Chinese Journal Full-text Database, VIP Journal Database, Wanfang database and English literature search engine and database, including Embase, Cochrane and Medline till January 2018, using the following key words: Irrigation fluid, temperature, bladder irrigation,shiver, hypothermia, and blood loss. Full text for all relevant key articles were retrieved and reviewed by first manually screening through titles and abstracts. The authors’ countries, the article’s publication year, type of surgery,bladder irrigation temperature and risk assessment items were recorded.
2.4. Selection of studies
A total of 162 Chinese literature and 14 English literature were retrieved. Two researchers independently screened the literature according to the following criteria: (1) Inclusion criteria: RCTs published before January 2018 regarding the influence of warm irrigation fluid on body temperature,blood loss and shiver,with the intervention of warm irrigation fluid. (2) Exclusion criteria: Non-RCTs studies; patients who had not undergone BPH surgeries,no bladder irrigation, or missing data.
2.5. Data extraction
Data extraction was performed independently by two reviewers according to the inclusion and exclusion criteria.If divergence occurred during the process of data extraction,a third party was joined in the discussion to solve the problem. The first author, published date, intervention,and results were extracted.
2.6. Quality of literature evaluation
According to the Cochrane handbook [2], the following quality evaluation standard items combined with the characteristics of studies were selected to test the stability of the conclusion: (1) Randomized distribution method; (2)allocation concealment; (3) comparability of baseline parameters; (4) result integrity; (5) method of blinding; (6)selective reporting; And (7) other sources of bias.
2.7. Statistical analysis
Revman 5.3, originally developed by the Cochrane Network, was used to perform the meta-analysis. Relative risk (RR) was used as the effect indicator of enumeration data and the 95%confidence interval(CI)was calculated.Q test was used to evaluate study heterogeneity. A p >0.1 with I2<50% was regarded as no heterogeneity between studies, and a fixed effects model was adopted. A random effects model was used otherwise. Inverted funnel plots were used to evaluate publication bias. If the funnel is symmetrical, the publication bias is considered small.
3. Results
Forty-eight studies were included for full-text retrieval from 176 studies screened.Twenty studies were excluded for the following reasons: (1) Thirteen studies had unspecified volume of bleeding;(2)Seven studies had unquantified drop in body temperature. Finally, 28 RCTs involving 3858 patients were included(Fig.1).The general information and quality assessment of included literature were summarized in Table 1.
3.1. Perioperative body temperature drop
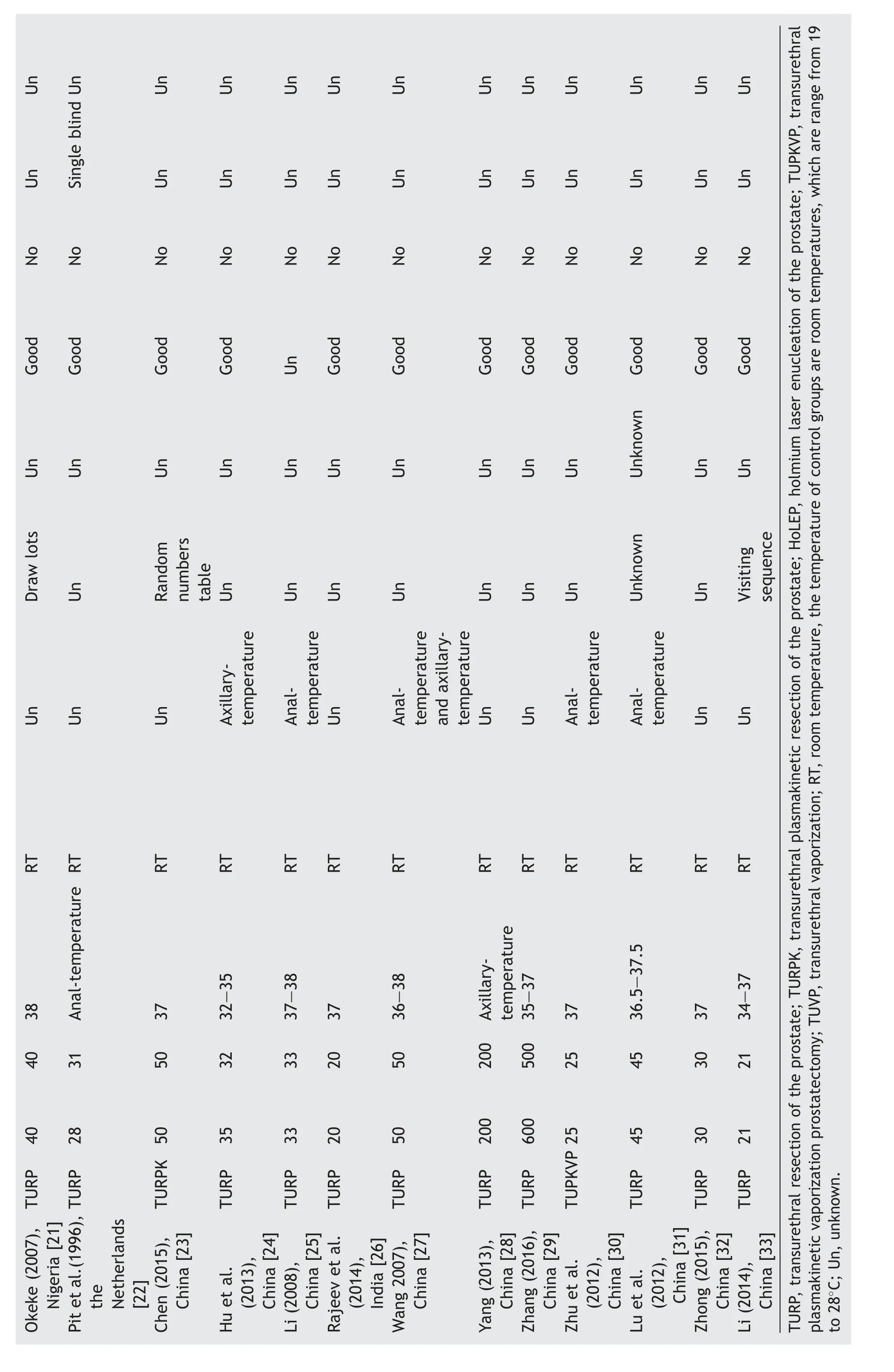
Six studies reported body temperature drop involving 429 patients, which was shown in Fig. 2. We omitted the combined statistics and performed a narrative descriptive statistics only because of substantial heterogeneity(P <0.00001, I2= 96%). All studies were consistent in the direction of results, which illustrated that warm irrigation fluid decreased the occurrence of body temperature drop.
3.2. Incidence of perioperative shiver
Nineteen studies reported the incidence of perioperative shiver and there was no significant heterogeneity among these studies(p=0.99,I2=0%).The incidence of shiver in the group of patients receiving warm irrigation fluid was lower than those receiving room-temperature fluid(RR = 0.32, 95% CI: 0.28-0.36, p <0.00001) (Fig. 3).
3.3. Incidence of perioperative hypothermia
Six studies reported the incidence of perioperative hypothermia and there was substantial heterogeneity between these studies(p=0.010,I2=67%).Warm irrigation fluid group had a lower incidence of hypothermia compared with roomtemperature group (RR = 0.36, 95% CI: 0.21-0.59,p <0.0001)(Fig.4).
Xu et al. [3] measured the temperature of lower esophagus and the other five studies measured body surface temperature. These might have caused the heterogeneity,therefore were excluded from the present study. Fig. 5 showed that after the sensitivity analysis, the heterogeneity disappeared(RR=0.29,95%CI:0.20-0.41,p <0.0001).
3.4. Perioperative blood loss
The amount of blood loss was recorded in milliliter. Three studies reported the patients’ blood loss and there was heterogeneity in between (p <0.00001, I2= 99%), which was shown in Fig. 6. We used the random effects mode combined analysis, and the results showed that there was no statistical significance between warm and roomtemperature irrigation fluid groups on the amount of patients’blood loss(mean deviation(MD)=-141.68,95%CI:-250.25 to -33.11, p = 0.01).
3.5. Inverted funnel plots
Inverted funnel plots were used to examine the publication bias in the literature,and the results showed that the figure was basically symmetrical, suggesting a small publication bias. Inverted funnel plot of perioperative blood loss was statistically insignificant, possibly due to a limited number of literature being included (Figs. 7-10).
4. Discussion
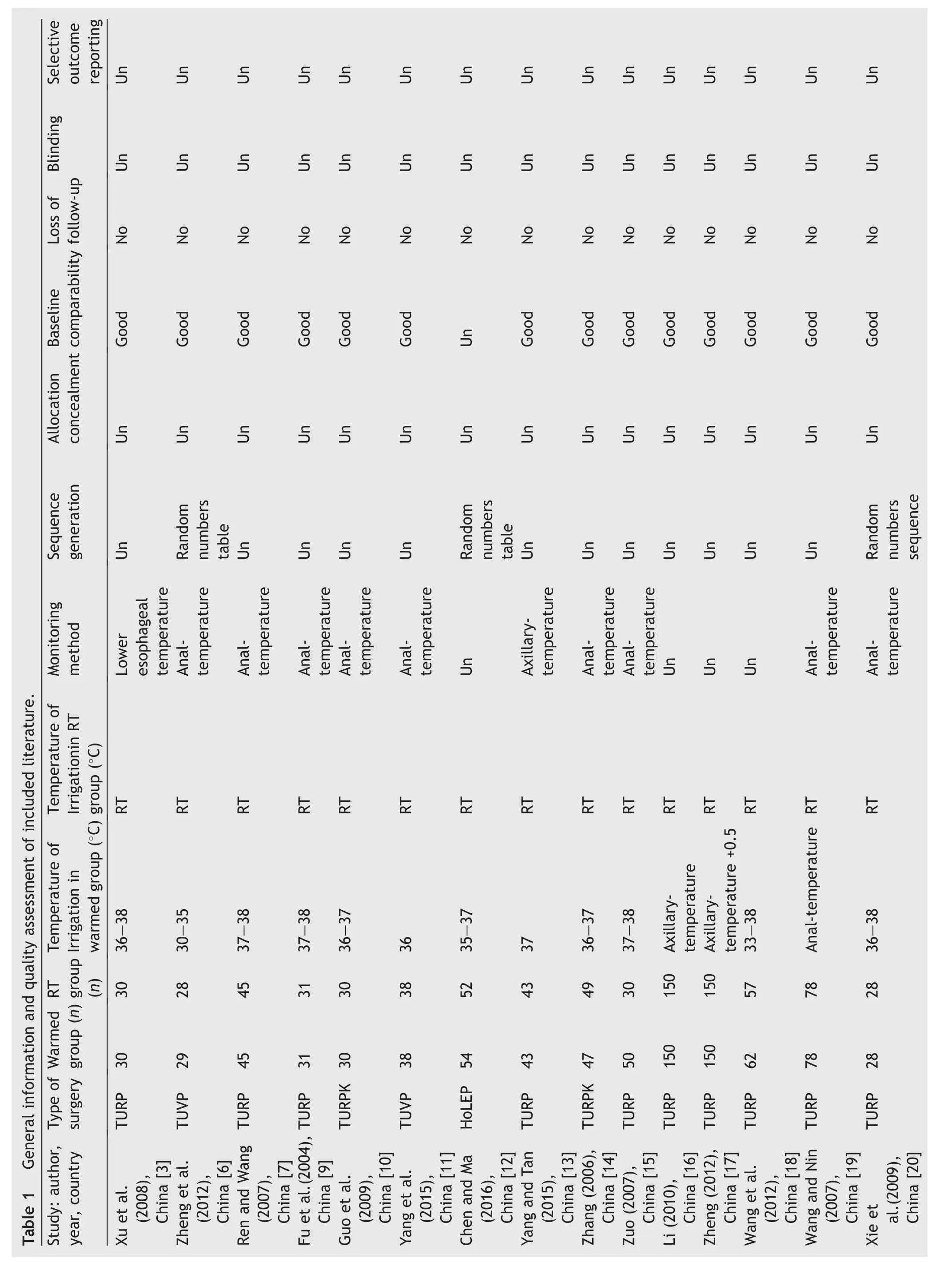
Table 1 General information and quality assessment of included literature.Study: author,year, country Type of surgery Warmed group (n)RTgroup(n)Temperature of Irrigation in warmed group(°C)Temperature of Irrigationin RT group (°C)Monitoring method Sequence generation Allocation concealment Baseline comparability Loss of follow-up Blinding Selective outcome reporting Xu et al.(2008),China [3]TURP 30 30 36-38 RT Lower esophageal temperature Un Un Good No Un Un Zheng et al.(2012),China [6]TUVP 29 28 30-35 RT Analtemperature Random numbers table Un Good No Un Un Ren and Wang(2007),China [7]TURP 45 45 37-38 RT Analtemperature Un Un Good No Un Un Fu et al.(2004),China [9]TURP 31 31 37-38 RT Analtemperature Un Un Good No Un Un Guo et al.(2009),China [10]TURPK 30 30 36-37 RT Analtemperature Un Un Good No Un Un Yang et al.(2015),China [11]TUVP 38 38 36 RT Analtemperature Un Un Good No Un Un Chen and Ma(2016),China [12]HoLEP 54 52 35-37 RT Un Random numbers table Un Un No Un Un Yang and Tan(2015),China [13]TURP 43 43 37 RT Axillarytemperature Un Un Good No Un Un Zhang (2006),China [14]TURPK 47 49 36-37 RT Analtemperature Un Un Good No Un Un Zuo (2007),China [15]TURP 50 30 37-38 RT Analtemperature Un Un Good No Un Un Li (2010),China [16]TURP 150 150 Axillarytemperature RT Un Un Un Good No Un Un Zheng (2012),China [17]TURP 150 150 Axillarytemperature +0.5 RT Un Un Un Good No Un Un Wang et al.(2012),China [18]TURP 62 57 33-38 RT Un Un Un Good No Un Un Wang and Nin(2007),China [19]TURP 78 78 Anal-temperature RT Analtemperature Un Un Good No Un Un Xie etal.(2009),China [20]TURP 28 28 36-38 RT Analtemperature Random numbers sequence Un Good No Un Un
Okeke (2007),Nigeria [21]TURP 40 40 38 RT Un Draw lots Un Good No Un Un Pit et al.(1996),theNetherlands[22]TURP 28 31 Anal-temperature RT Un Un Un Good No Single blind Un Chen (2015),China [23]TURPK 50 50 37 RT Un Random numbers table Un Good No Un Un Hu et al.(2013),China [24]TURP 35 32 32-35 RT Axillarytemperature Un Un Good No Un Un Li (2008),China [25]TURP 33 33 37-38 RT Analtemperature Un Un Un No Un Un Rajeev et al.(2014),India [26]TURP 20 20 37 RT Un Un Un Good No Un Un Wang 2007),China [27]TURP 50 50 36-38 RT Analtemperature and axillarytemperature Un Un Good No Un Un Yang (2013),China [28]TURP 200 200 Axillarytemperature RT Un Un Un Good No Un Un Zhang (2016),China [29]TURP 600 500 35-37 RT Un Un Un Good No Un Un Zhu et al.(2012),China [30]TUPKVP 25 25 37 RT Analtemperature Un Un Good No Un Un Lu et al.(2012),China [31]TURP 45 45 36.5-37.5 RT Analtemperature Unknown Unknown Good No Un Un Zhong (2015),China [32]TURP 30 30 37 RT Un Un Un Good No Un Un Li (2014),China [33]TURP 21 21 34-37 RT Un Visiting sequence Un Good No Un Un TURP, transurethral resection of the prostate; TURPK, transurethral plasmakinetic resection of the prostate; HoLEP, holmium laser enucleation of the prostate; TUPKVP, transurethral plasmakinetic vaporization prostatectomy;TUVP,transurethral vaporization;RT,room temperature,the temperature of control groups are room temperatures,which are range from 19 to 28°C; Un, unknown.
The incidence of BPH presents a rising trend in aged population.It affects the quality of life of elderly patients[4].After BPH surgeries, clinical nursing staffs usually use the bladder irrigation to prevent blood clot from forming and blocking the catheter. Bladder irrigation is a key intervention for urologic patients that are used continuously from the beginning of the surgery to approximately one day postoperatively. This article is a meta-analysis of relevant RCTs to evaluate the influence of warm irrigation fluid on perioperative hypothermia, blood loss and shiver, which can help medical staffs to determine the appropriate temperature of bladder irrigation fluid.
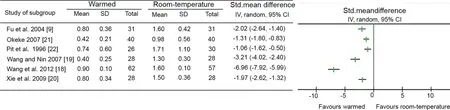
Figure 2 The value of perioperative body temperature drop for warmed group and room-temperature group.Std,standard;SD,standard difference; CI, confidence interval. CI, confidence interval.
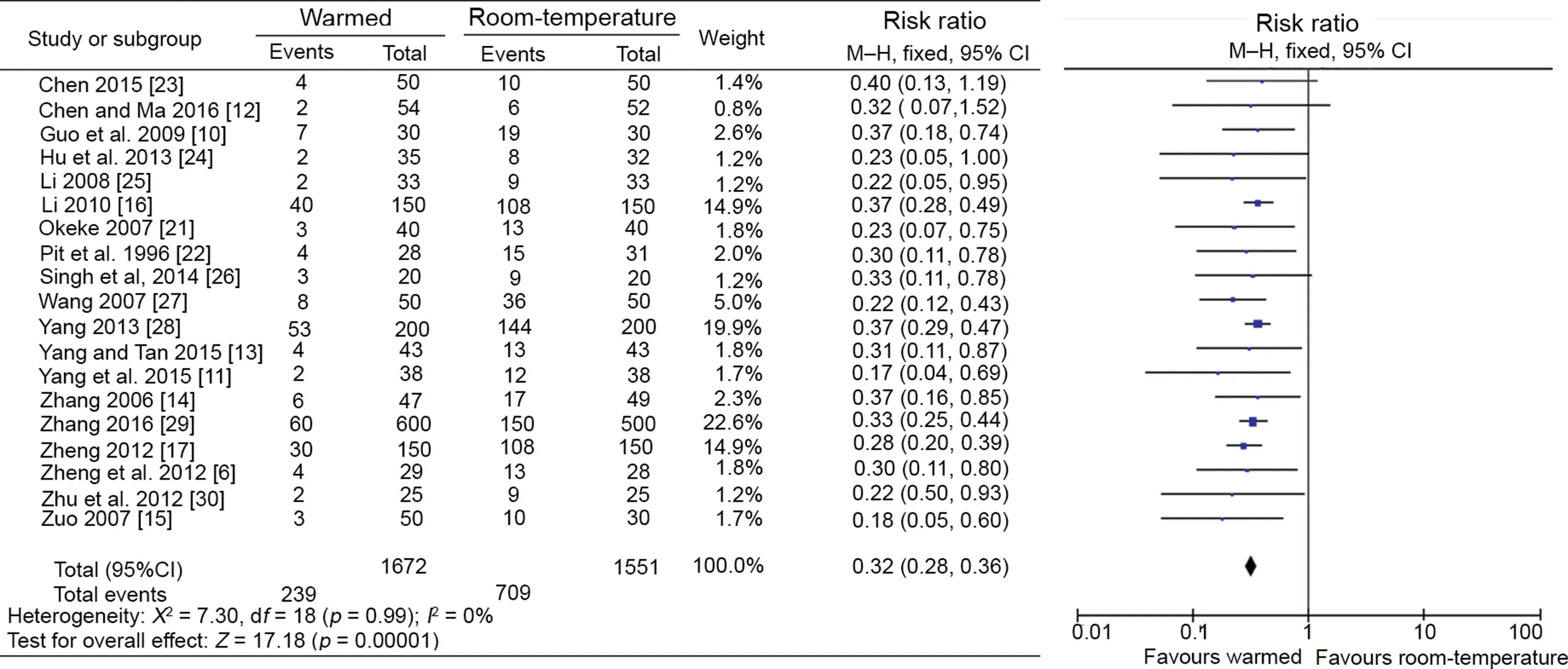
Figure 3 The incidence of perioperative shiver for warmed group and room-temperature group. CI, confidence interval.
4.1. The advantage of warm bladder irrigation
Perioperative hypothermia is defined as perioperative core temperature being lower than 36.0°C[5,32].The difference in body temperature is related to the temperature regulating function in different patients, the ambient temperature of the operating room,type of the operation,and the duration of the operation, especially the operation with longer time of bladder irrigation. Room-temperature irrigation fluid may lower the core and peripheral body temperature[6].Several researches have concluded that roomtemperature irrigation fluid can cause a drop of body temperature, which may even lead to perioperative hypothermia[3,7].Perioperative hypothermia causes a series of disadvantages,such as delayed awakening from anesthesia,influence to cardiovascular function, reduce the blood pressure of the patient, increased risk of surgical site infection and shiver [8-10]. Shiver may increase patients’discomfort, anxiety and oxygen consumption. It also increases the load on the heart and even lead to onset of cardiovascular diseases. Excitation of the sympathetic nerve can reduce renal blood flow and glomerular filtration rate significantly, which results in renal insufficiency [11].Some researchers reported that patients with shiver increased the incidence of myocardial ischemia, and the drop of body temperature caused various physiological function changes [12,13]. Zhang and Zuo [14,15] reported that body-temperature irrigation fluid reduced the occurrence of perioperative hypothermia and increased operation safety. Li and Zheng [16,17] reported that body temperature fluid did not irritate the bladder, thus reducing the incidence of bladder spasm and keeping the bladder blood vessels in a normal function.
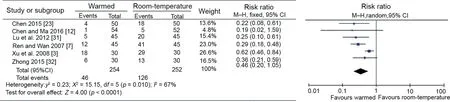
Figure 4 The incidence of perioperative hypothermia for warmed group and room-temperature. CI, confidence interval.
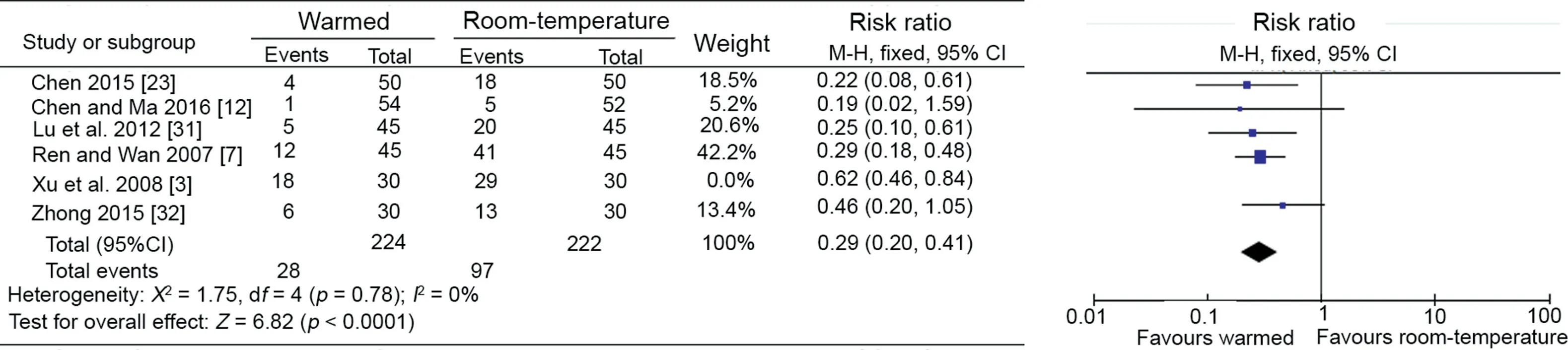
Figure 5 Sensitivity analysis of the incidence of perioperative hypothermia for warmed group and room-temperature. CI, confidence interval.
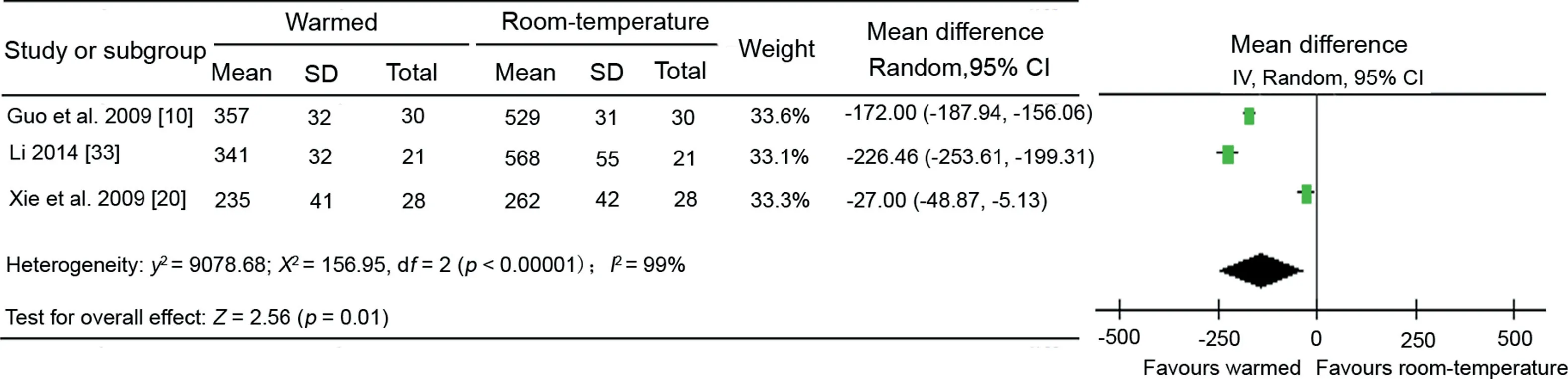
Figure 6 The value of perioperative blood loss for warmed group and room-temperature group. CI, confidence interval.
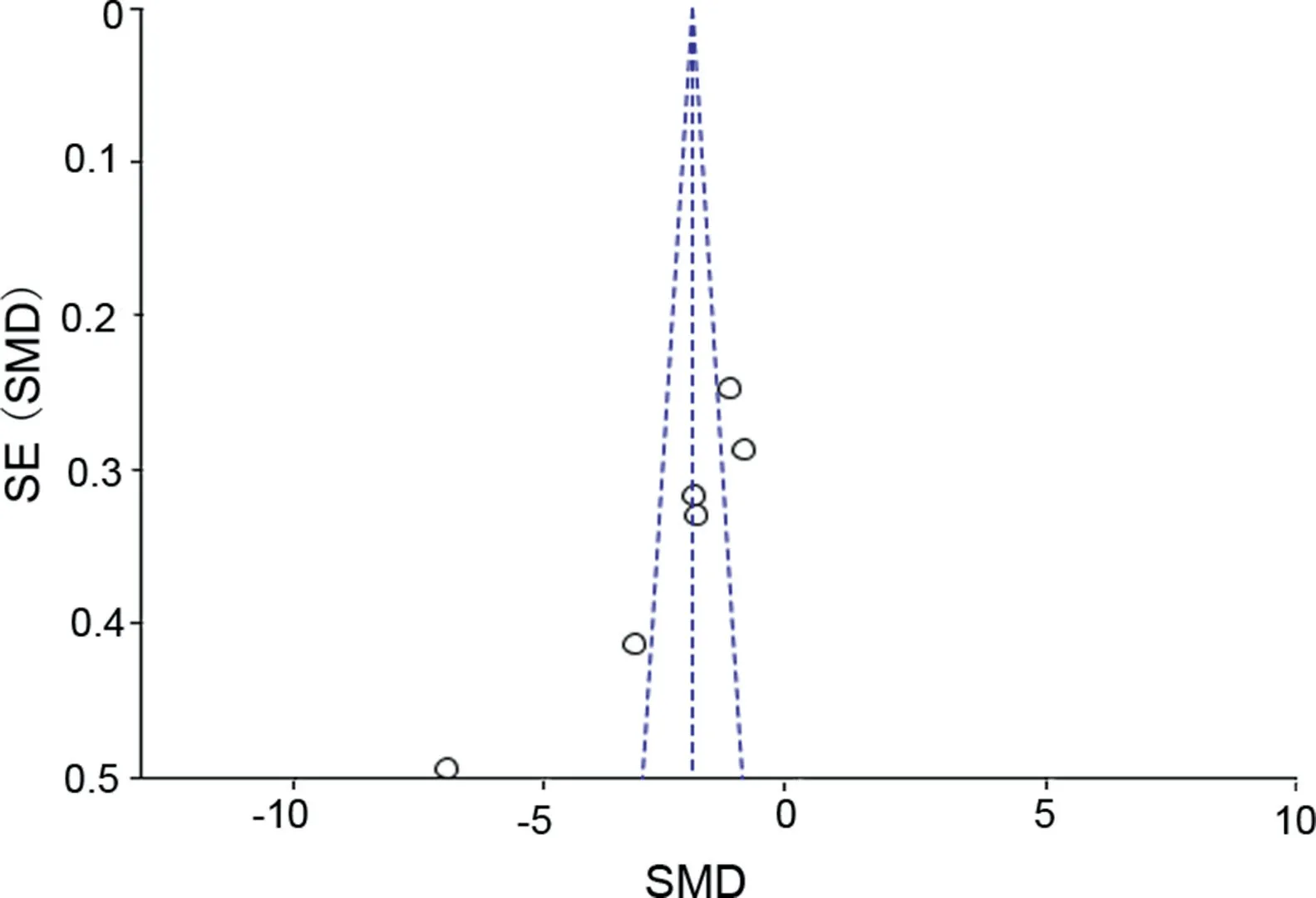
Figure 7 Inverted funnel plot of perioperative temperature drop. SMD, standardised mean difference; SE, standard error.
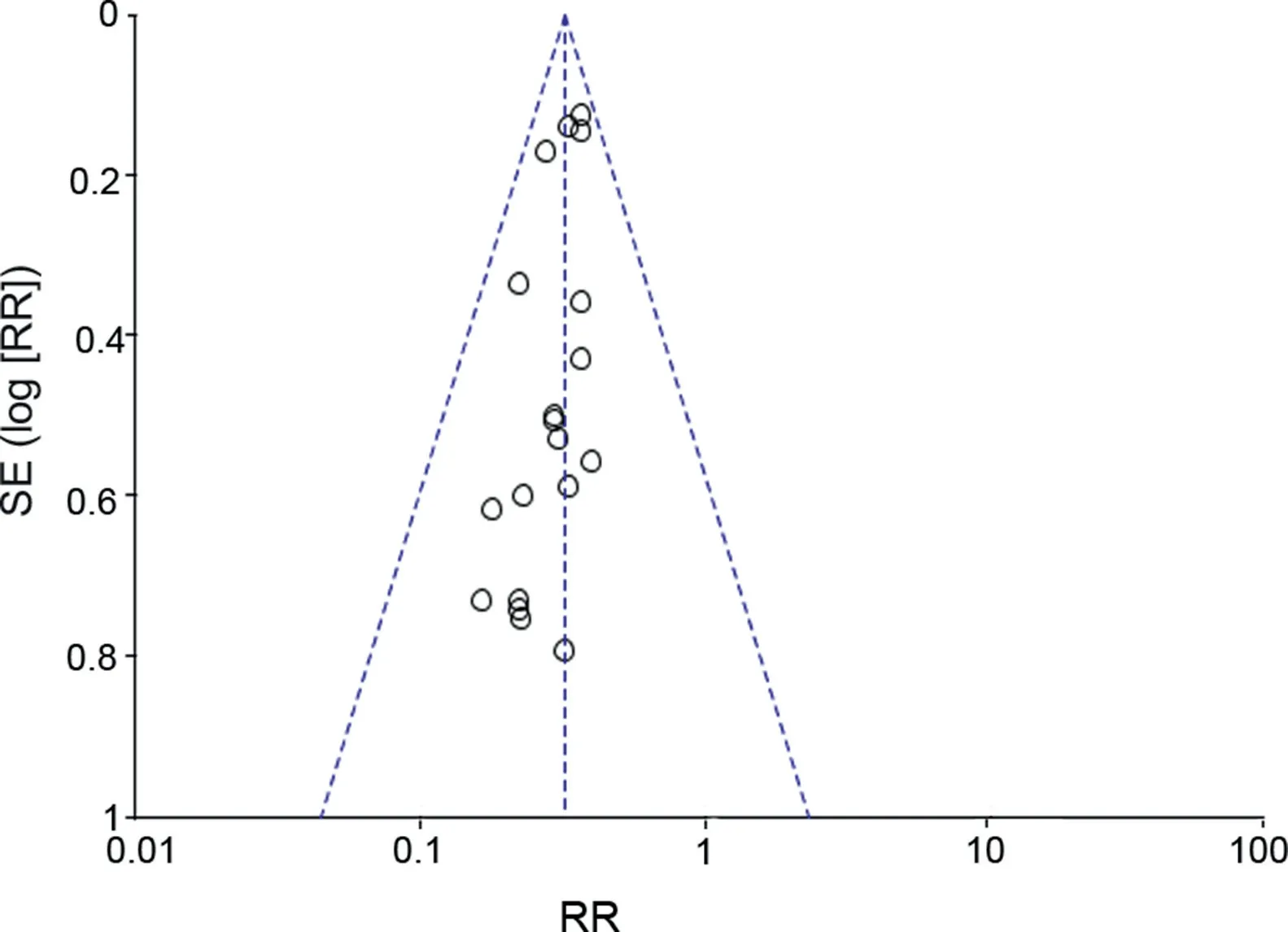
Figure 8 Inverted funnel plot of perioperative shiver. SE,standard error; RR, risk ratio.
4.2. The limitations of research
Some literature was not accessible, including unpublished and grey literature, which may lead to deviation. A small sample of RCTs was used, which may cause a generally low study quality.All researches included were not sufficient in research method information and the methodological quality was low on hidden, blinded, and other factors such as bias report.
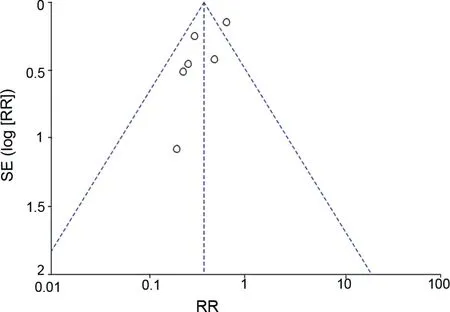
Figure 9 Inverted funnel plot of perioperative hypothermia.SE, standard error; RR, risk ratio.

Figure 10 Inverted funnel plot of perioperative blood loss.SE, standard error; MD, mean difference.
5. Conclusion
We now have a deeper understanding on prostate surgeryrelated complications through the systematic review results. We can draw the conclusion that warm bladder irrigation fluid can decrease the drop of body temperature and the incidence of hypothermia and shiver during and after the operation for BPH.Warm irrigation fluid should be considered as a standard practice in BPH surgeries. Large sample of RCTs are hoped to be taken to provide more strengthened evidence in the future.
Author contribution
Study design: Jie Cao, Lingjuan Zhang.Data acquisition: Yan Ding.Data analysis: Jie Cao,Yan Ding.Drafting of manuscript: Jie Cao.Critical revision of the manuscript:Xia Sheng,Xiaoying Lu.
Conflicts of interest
The authors declare no conflict of interest.
 Asian Journal of Urology2019年2期
Asian Journal of Urology2019年2期
- Asian Journal of Urology的其它文章
- Asynchronous abdominal wall and sigmoid metastases in clear cell renal cell carcinoma:A case report and literature review
- Compliance in patients with dietary hyperoxaluria: A cohort study and systematic review
- Dose escalation of external beam radiotherapy for high-risk prostate cancer-Impact of multiple high-risk factor
- Is Retzius-sparing robot-assisted radical prostatectomy associated with better functional and oncological outcomes?Literature review and meta-analysis
- Beyond prostate, beyond surgery and beyond urology: The “3Bs” of managing non-neurogenic male lower urinary tract symptoms
- Systemic treatment for metastatic prostate cancer
