Progress in image-guided radiotherapy for the treatment of nonsmall cell lung cancer
Xiao-Cang Ren, Yue-E Liu, Jing Li, Qiang Lin
Abstract
Key words: Non-small cell lung cancer; Radiotherapy; Image-guided radiotherapy;Intensity-modulated radiotherapy; Positioning error
INTRODUCTION
Lung cancer is one of the most common malignant tumors, and it ranks first in both incidence and mortality worldwide. Non-small cell lung cancer (NSCLC) accounts for 80%-85% of all lung cancers. Late diagnosis of NSCLC is very common in clinical practice, and most patients miss the chance for radical surgery. Thus, radiotherapy is one of major treatment modalities for NSCLC. In recent years, continuous advancements in image-guided radiotherapy (IGRT) technology have enabled more accurate positioning and precise radiotherapy. IGRT can decrease errors during treatment, increase the local radiation dose, and reduce the dose of radiation delivered to the normal surrounding tissue to optimize the local tumor control rate and significantly improve patient quality of life. This paper presents a brief review of the technical developments and application of IGRT in recent years.
STATUS OF RADIOTHERAPY
Lung cancer has increased globally in both incidence and mortality. It ranks first among malignant tumors in both incidence and mortality worldwide and is a threat to human health. NSCLC account for 80%-85% of all lung cancers, and early diagnosis is limited. Approximately 85% of patients are in advanced stages at the time of diagnosis. The efficacy of surgical treatment is not ideal, and the 5-year survival rate is only about 16%. According to statistics radiotherapy was widely utilized as high as 55% in all new cancer cases. In traditional two-dimensional radiotherapy, an oncologist must control the treatment based on his experience because the imaging diagnosis and positioning system operate on a two-dimensional plane. Irradiating a large area can easily destroy normal cells around the tumor but not the tumor itself.Therefore, the treatment efficacy is poor, with obvious side effects and many complications. The ideal radiotherapy technique is to deliver a lethal dose to the target area according to the shape of the tumor without irradiating the normal tissue around the target area. In 1959, Dr. Takahashi from Japan first proposed and outlined the concept of conformal radiation therapy. The development and application of technologies such as computed tomography (CT), magnetic resonance imaging, threedimensional treatment planning systems and multi-leaf collimators have made threedimensional conformal radiotherapy possible and facilitated the transition from the 2-dimensional era to the 3-dimensional era. In recent years, many new technologies and new methods for improving the accuracy of treatment have been developed.Technologies such as three-dimensional conformal radiation therapy (3DCRT) and intensity-modulated radiation therapy (IMRT) have solved the problem of dose conformation in stationary target areas. However, the position and shape of the tumor and the positional relationship between the tumor and its surrounding organs can change over the course of treatment. The proactive treatment method uses a certain technique to detect the positioning error and/or movement of the target area and to improve the delivery of radiation to the tumor while correcting the error to better protect the surrounding normal tissues. Methods to ensure and control the quality of radiation therapy are still under active investigation.
DEFINITION OF IGRT
Compared to traditional radiotherapy, IGRT enhances the biological effects of radiotherapy and is considered an extension of 3DCRT and IMRT. It integrates respiratory movement over time during treatment and positioning error between fractions. It is the most advanced four-dimensional radiotherapy technology in the field of tumor treatment, featuring accurate positioning, plan design and control of the accelerators. IGRT can correct the patient's positioning error, aid in planning subsequent radiotherapy, guide real-time beam irradiation, and collect images and/or other signals during treatment in order to ensure the accuracy of radiation delivery.The collected images and/or signals are used to guide and deliver the dose of radiation to the target area and ultimately improve the rate of local control rate and long-term survival in patients with advanced NSCLC. IGRT technology can correct the error between the lesions and the markers and modify the changes in the radiation dose between the tumor and normal tissues. It can reasonably adjust the dose to protect normal tissue while reducing the safe marginal region and increasing dose delivery to the tumor area. IGRT can be achieved using the following technologies:online correction, adaptive radiotherapy, breath-holding and respiratory gating control, four-dimensional radiotherapy and real-time tracking technology.
IMPLEMENTATION OF IGRT IN NSCLC RADIOTHERAPY
Online correction technology
During the course of fractional treatments, two-dimensional or three-dimensional images of the patient are acquired and compared to the planned image (preplaced markers) after positioning to determine the positioning error or the error of the radiation field, which are corrected immediately to obtain the appropriate position of the target area. The optimal radiation dose can then be delivered. In recent years,online correction has evolved from earlier film to current electro phoretic image display technology, which increases the degree of automation and shortens the additional treatment time. Moreover, the X-ray source for imaging has evolved from MV imaging to KV-MV combination imaging or KV imaging alone, and the technology for the calibration image has also evolved from two-dimensional to threedimensional imaging such as spiral CT or cone beam CT (CBCT).
Adaptive radiotherapy
Due to individual differences, the actual appropriate width of the marginal region around the target areas different for each patient. Therefore, it is necessary to set an individualized width of the marginal region according to the individual's positioning error and organ movement data and then to adjust the margins of the planned target volume (PTV) and the clinical target volume. The plan and mode of adaptive radiation therapy can be modified using a systematic feedback of measurements during treatment.
Conventional radiotherapy plans are designed based on CT images obtained before radiotherapy. However, changes in the patient's body mass index, tumor deformation, and movement of the surrounding organs can cause displacement of the target and consequent deformation. CBCT-guided adaptive radiotherapy is a new extension of IGRT technology that allows for feedback of the target tumor volume and position changes during treatment to analyze the difference between the original plan and the treatment and to obtain real-time anatomical images in order to re-design the treatment plan. This technique can ensure appropriate dose delivery to the target area and reduce unnecessary irradiation of normal tissue, thus minimizing the side effects of radiotherapy. A study by Zhao et aldescribed how to delineate the target area using the anatomical images collected by CBCT and how to form an outline of the new target area using deformation registration software. Under the guidance of CBCT, the treatment plan can be re-optimized. CBCT also allows for updated calculations of the actual dose accumulation in the target area and surrounding organs and an accurate final determination of the radiation dose for further treatments in order to reduce damage to normal tissues and increase dose delivery to the target area. Buckley et alproposed CBCT-guided helical tomotherapy (HT) as a replacement for IMRT to achieve adaptive contour delineation, planning, and fractional dose accumulation.Currently, studies of CBCT-guided radiotherapy for NSCLC mainly focus on respiratory movement and shrinkage of the target area. Interference of respiratory movement can be improved by techniques such as respiratory gating, real-time tracking and 4D-CT, while the effect of target shrinkage can be effectively addressed by the timely modification of radiotherapy plans. Adaptive radiotherapy technology based on CBCT image guidance could be comparable to adaptive HT with further optimization of the time required for adaptive radiotherapy planning. De et alreported that HT and IGRT are effective and safe treatment modalities for anal cancer and are considered standard of care for these conditions in our department. A study by Elsayad et aldemonstrated 83% tumor regression and 13% progression in patients with small cell lung cancer (13 patients) or NSCLC (59 patients) undergoing fractional CBCT-guided radiation. Moreover, the decrease in gross tumor volume was associated with the number of CBCT scans (r = 0.313, P = 0.046) and the time of chemotherapy administration (r = 0.385, P = 0.013). Weekly CBCT to monitor changes in the tumor offers the advantage of adaptive treatment for patients with lung cancer.
Breath-holding and respiratory gating technology
If the target area is affected by respiratory movement, breath-holding can temporarily eliminate such movement, allowing for a small marginal region. Before treatment, the patient should perform appropriate breathing exercises to increase the duration of breath-holding during treatment and to reduce the volume of lung radiation exposure. Active respiratory gating technology and deep inspiration breath hold techniques are the two options available to minimize the influence of respiratory movement. Respiratory gating is a technique that collects images from different respiratory phases in NSCLC patients and reconstructs images by using fourdimensional computed tomography (4D-CT). It can be used to calculate and reconstruct doses at different respiratory phases to better eliminate movement artifacts, adjust the radiation plan, and monitor the effects of the patient's respiratory movement on the organ and target tumor area during treatment. Ultimately, this technique allows for control of the intensity of the radiation beam to the linear accelerator and matches the specific phase of the respiratory cycle of NSCLC patients with the controlled radiation beam. Respiratory gating technology can reduce the influence of respiratory movement on radiotherapy. For instance, patients with stage I to II lung cancer who are affected by respiratory movements and patients with subphrenic tumors are better suited to respiratory gating technology with hypofractionated radiation therapy.
During radiotherapy, respiratory and organ movement in NSCLC patients causes movement of the tumor target area and displacement of the tumor's position in the lung, resulting in differences in anatomical position between the planned design and actual treatment. Moreover, changes in the volume and density of the lung tissue result in beam penumbra changes in the field and a lower dose of radiation delivery to the tumor target in lung tissue. Therefore, during IGLFRT, in addition to expansion of the radiation target area, assisted respiratory gating technology can help reduce the scope of treatment while increasing dose delivery to the tumor target area. This can effectively avert the possibility of mistargeted dose delivery and the consequent excessive exposure of normal tissue to radiation due to individual differences in respiratory movement.
Radiotherapy techniques accounting for time
Three-dimensional radiotherapy technology can be further enhanced by accounting for time using a technique that accounts for changes in anatomical structure during imaging positioning, planning, and therapeutic implementation. Three key factors must be taken into consideration: four-dimensional image localization (collecting the time sequence of four-dimensional images throughout all phases in one respiratory cycle), four-dimensional plan design (determination of time-marked field parameters from four-dimensional image data), and four-dimensional treatment implementation(monitoring of the patient's breathing using the same respiratory monitoring device used in the four-dimensional imaging system).
During the course of routine spiral CT scanning, movement artifacts can cause up to 90% volumetric deviation in the 3D reconstruction of the target area. Therefore, it is very important to individualize the target range of movement in NSCLC patients. The development of 4D-CT technology not only effectively eliminates movement artifacts to accurately and reliably reproduce the target area receiving radiotherapy but also can reflect the dynamic characteristics of radiotherapy in the target area with respect to respiratory movements and perform precise, individualized delineation of the target area. 4DCT takes advantage of three-dimensional reconstruction technology and integrates a time factor during image positioning, planning and treatment implementation stages.It also incorporates changes in anatomical structure over time, individualized target volume (ITV) changes and respiratory cycle. A study by Tan et alhas shown that 4D-CBCT is superior to 3D-CBCT in image guidance in small lung tumors because 4D-CBCT can reduce the uncertainty of the tumor location caused by internal respiratory movement, thereby increasing the accuracy of image guidance. Ehrbar et alused 4D-CT to delineate ITV and design a radiotherapy plan for patients with lung cancer. Their results show that ITV ensured tumor coverage but that the lung tissue was exposed to higher doses of radiation. Significantly reduced ITV can improve tumor control while protecting normal tissues. In addition, Jurkovic et alused the average intensity projection and maximum intensity projection techniques to quickly and accurately delineate ITV. These techniques can significantly reduce the physical effort involved in target delineation. ITV delineation based on 4D-CT can increase the target dose and reduce the marginal region, thus reducing the radiation dose delivered to normal lung tissue.
Real-time tracking with stereotactic body radiotherapy
Because human respiratory movement is not strictly identical between two consecutive cycles, and treatment time is often longer than the image positioning time, especially when using hypofractional techniques (such as stereotactic radiotherapy), involuntary movements cannot be predicted. Real-time X-ray tracking treatment techniques have been developed to address this problem.
Image-guided hypofractionated stereotactic radiotherapy after accurate positioning in NSCLC patients can deliver large doses to the tumor target area, whereas the dose of radiation delivered to surrounding normal lung tissue is decreased. The tumor control rate of conventional radiotherapy is low in some patients with early NSCLC who are not candidates for surgical treatment. IGRT treatment can reduce the uncertainty of the positioning error and the movement of the target area, thereby reducing the irradiation volume, which can allow for increased daily treatment doses,shortened treatment time, and improved local control. For patients undergoing hypofractionated stereotactic radiotherapy, during the course of treatment, image guidance techniques are used to correct positioning errors and to monitor changes in tumor volume and location, thus ensuring coverage of the target area and reducing the dose absorbed by surrounding tissues. A study by Ehrbar et alshowed that the control rate and overall survival of patients undergoing hypofractionated stereotactic treatment are superior to those of patients receiving conventional radiotherapy. Moreover, side effects were less common with hypofractionated radiotherapy. Verma et alevaluated 92 patients from 12 institutions and found from their multi-institutional study that the toxicity of stereotactic body radiotherapy(SBRT) in patients with NSCLC tumors ≥ 5 cm was acceptable. Daily treatment are associated with a high toxicity rate. Vivek et alreported that the 1- and 2-year actuarial local control rates in patients with NSCLC tumors ≥ 5 cm were 95.7% and 73.2%, respectively, and the 1-year and 2-year disease-free survival rates were 72.1%and 53.5%, respectively; the 1- and 2-year disease-specific survival rates were 95.5%and 78.6%, respectively. Their study indicates that SBRT is a safe and effective treatment when combined with IGRT technology (Figure 1 and Table 1).
CONCLUSION
In summary, image-guided hypofractionated radiotherapy has several advantages in the treatment of NSCLC. Functional imaging allows for the differentiation of normal tissue from tumor tissue. By ensuring radiotherapy accuracy and appropriate dosing,these technologies can lower the radiation dose delivered to normal surrounding tissue while improving the local tumor control rate of the tumor and reducing the chance of radiation complications. This results in improved the quality of life of patients after treatment. Treatment that is based on advanced image guidance technology and computer-assisted adaptive radiotherapy is likely to become the most common approach for NSCLC radiotherapy in the future.
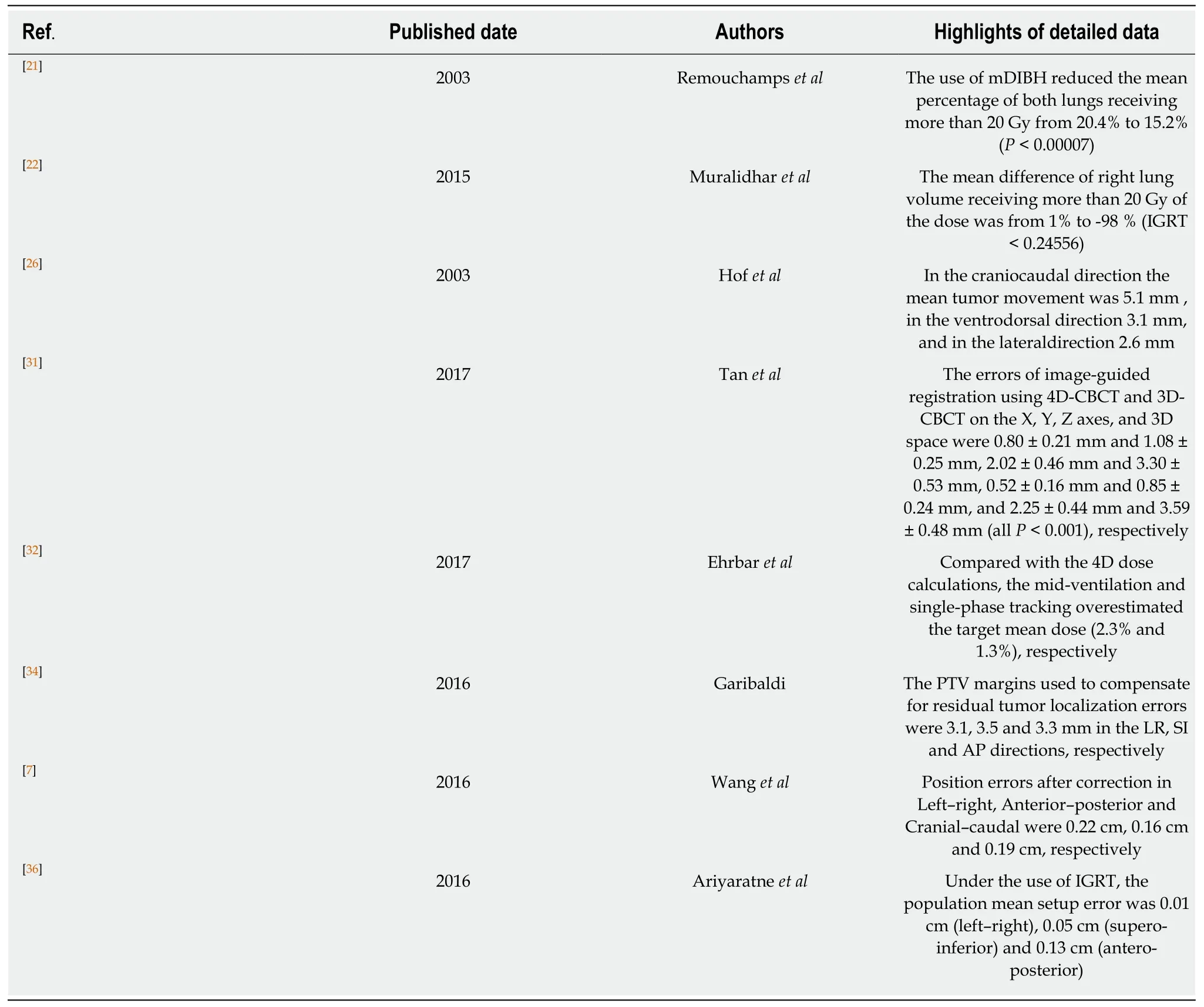
Table 1 Summary of important data of advantage of image-guided radiotherapy in radiotherapy
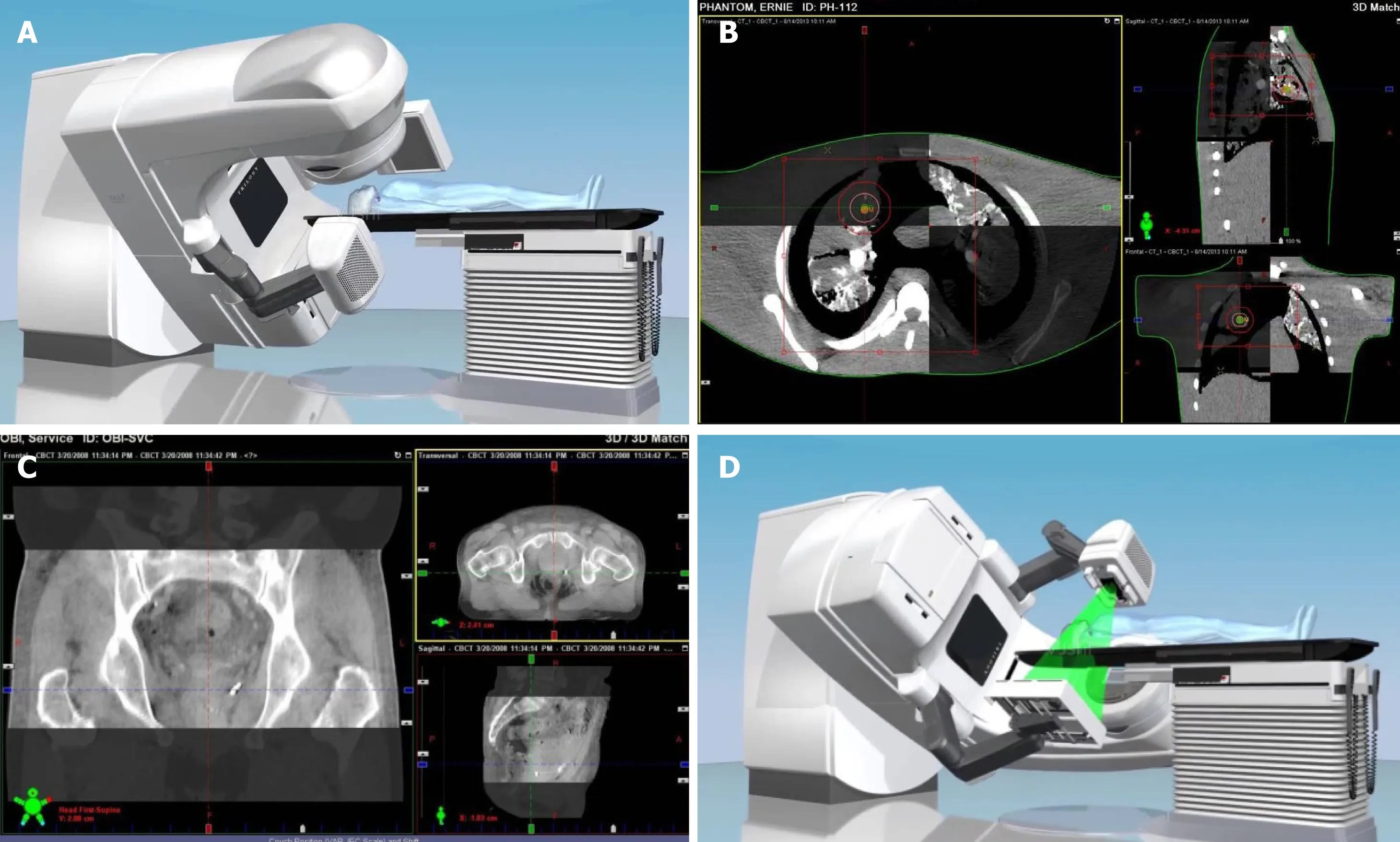
Figure 1 lmages of computed tomography. A: The placement of cone beam computed tomography; B: Chest image fusion; C: Pelvic image fusion; D:Radiotherapy after correction with image-guided radiotherapy.