Clinical observation of laparoscopic radical gastrectomy for advanced gastric cancer
Xiao-Xiao Yan, Yong-Hong Dong, Jing Wang, Ji-Guang Xie, Jun-Jun Su
1Shanxi University of Traditional Chinese Medicine, Taiyuan, Shanxi 030000, China. 2People's Hospital of Shanxi Province, Taiyuan, Shanxi 030000, China. 3Shanxi Medical University, Taiyuan 030000, China.
Introduction
In China, the incidence of gastric cancer accounts for a large proportion, many patients cannot be diagnosed and treated in time. Early symptoms of gastric cancer are not obvious, and some manifestations are weight loss, hematemesis, and loss of appetite. However, most patients have no symptoms and have entered the advanced stage when the disease is first diagnosed. The cancerous tissues of advanced gastric cancer mainly invade the submucosa or serosal layer. The peripheral lymph nodes are the earliest cancer cells to metastasize and may be transferred to the liver, lung, brain and other parts in the later stage, which affects the survival time of patients [1]. According to the AJCC/UICC eighth edition gastric cancer TNM staging, patients with stage II and III are mainly treated with surgery. In addition to the traditional radical surgery for gastric cancer,laparoscopic radical gastrectomy (LRG) is also widely carried out. How to choose a treatment that does not affect the treatment effect and enables the patient to recover quickly is a task for the clinician. The results of recent clinical studies of laparoscopic and open radical gastrectomy in our hospital are reported below.
Materials and methods
General data
116 patients with advanced gastric cancer admitted to our hospital from January 2017 to May 2018 were randomly selected. Among them, 55 patients underwent radical laparoscopic surgery, which was the experimental group; 61 patients under open surgery were included in the control group. The 116 patients were composed of 88 males and 28 females. Inclusion criteria: (1) under endoscopy, the results of the disease showed gastric cancer; (2) patients who met the eighth edition of TNM stage II, III; (3) aged 35-75 years; (4)Voluntary signing of informed consent (5) has been approved by the Ethics Committee of our hospital.Exclusion criteria: (1) patients with the eighth edition of TNM stage I and IV; (2) patients with severe heart, liver,kidney, brain and other complications; (3) patients undergoing chemotherapy before surgery; (4) patients with poor compliance.
Surgical methods
Open surgery is the same as laparoscopic preparation.Before radical laparoscopic surgery, five holes were made in the abdomen, and CO2 pneumoperitoneum was established in the umbilicus, maintaining at 12-15 mmHg. Specific surgical methods and lymph node dissection methods are described in the laparoscopic surgery for gastric cancer (2016 edition) [2]. In the open surgery group, conventional open radical surgery was performed, and a 25-30 cm incision was made in the middle of the abdominal wall of the patient, using conventional D2 radical surgery. Proximal gastrectomy,distal gastrectomy, and total gastrectomy were performed depending on the location and size of the tumor. In the experimental group, 23 patients underwent distal gastrectomy, 17 underwent proximal gastrectomy,and 15 underwent total gastrectomy. In the control group, 21 patients underwent distal gastrectomy, 18 underwent proximal gastrectomy, and 22 underwent total gastrectomy.
Observation indicators
The intraoperative and postoperative clinical treatment effects (operative time, length of incision, exhaust time,intraoperative blood loss, total number of lymph nodes removed, length of hospital stay, enteral nutrition time),tumor markers (CEA, CA-199, AFP), and postoperative complications (incision infection,pulmonary infection, anastomotic leakage, intestinal obstruction, gastroparesis, postoperative bleeding) were observed.
Statistical methods
All data were analyzed by SPSS 21.0 software. The measurement data were expressed by `the mean (`x) ±standard deviation (SD), using t-test or rank sum test;the count data were analyzed by χ2test, expressed by n%, P < 0.05 was considered to be statistical significance.
Results
General Information
There were no significant differences in gender, age,tumor diameter, body mass index, TNM stage, and gastric resection between the experimental group and the control group (P > 0.05) (Table 1).
Comparison of cl inical o utcomes bet ween the tw o groups in operation and postoperative stage
The average operation time, incision length, exhaust time, intraoperative blood loss, the total number of lymph nodes cleaned, hospitalization time, and enteral nutrition time in the experimental group were better than those in the control group (P < 0.05). The comparison was statistically significant (Table 2).
Comparison of CEA, CA-199, and AFP between the two groups before and 1 month after surgery
There were no significant differences in CEA, CA-199,and AFP between the two groups before and 1 month after surgery (P > 0.05), but the tumor index was significantly lower than that before surgery (Table 3).
Comparison of postoperative complications between the two groups
There were 5 cases of postoperative complications in the experimental group, the incidence rate was 9.1%(5/55), including 1 case of wound infection, 1 case of pulmonary infection, 1 case of intestinal obstruction, 1 case of gastroparesis and 1 case of hemorrhage. The incidence of postoperative complications was 17 cases,the incidence rate was 27.9% (17/61), including 2 cases of wound infection, 5 cases of pulmonary infection, 1 case of anastomotic fistula, 3 cases of intestinal obstruction, 4 cases of stomach cramps, 2 cases of hemorrhage.The number of postoperative complications in the experimental group was significantly lower than that in the control group (P < 0.05) (Table 4).
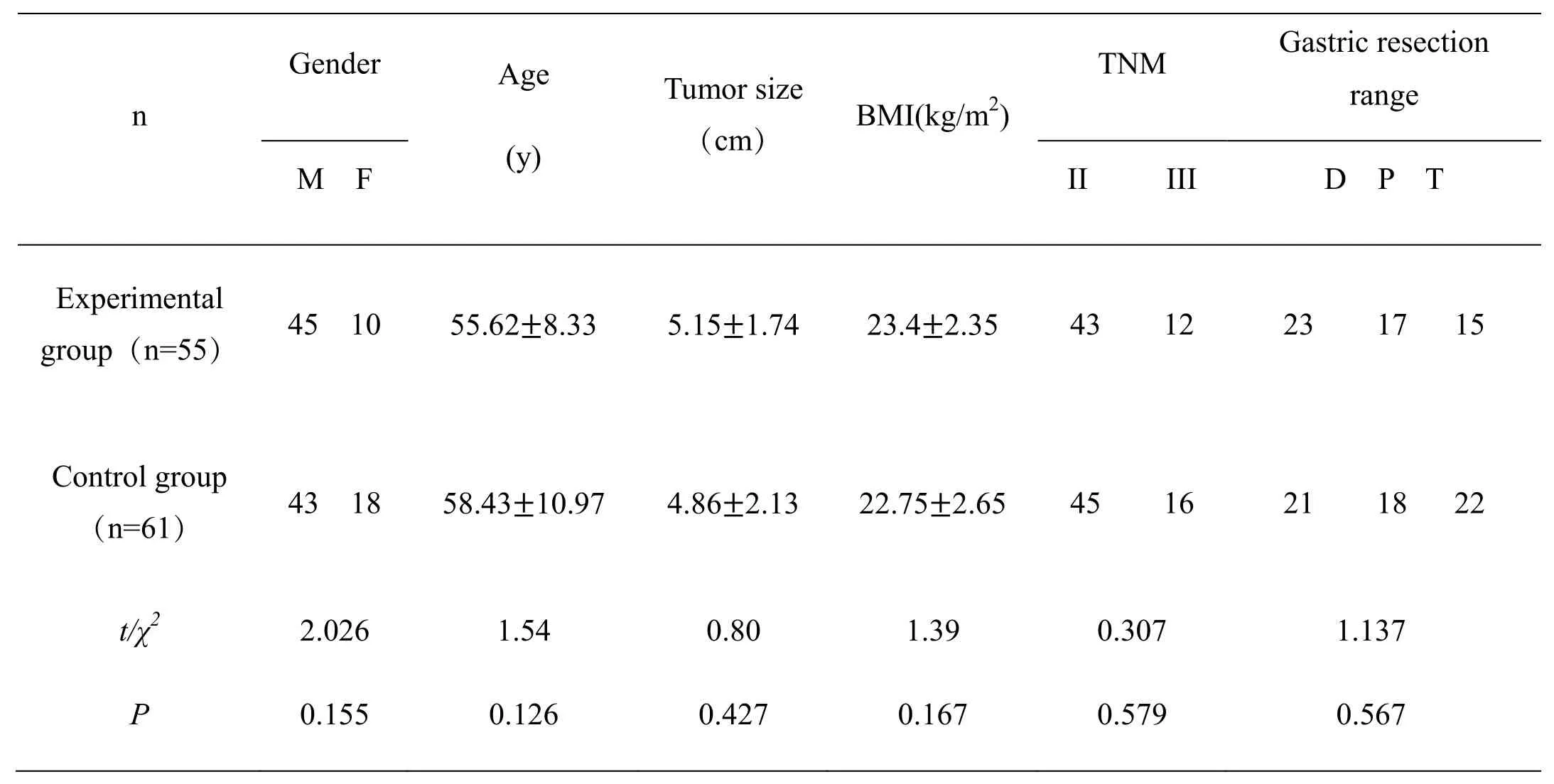
Table 1 Comparison of general conditions between the two groups of patients
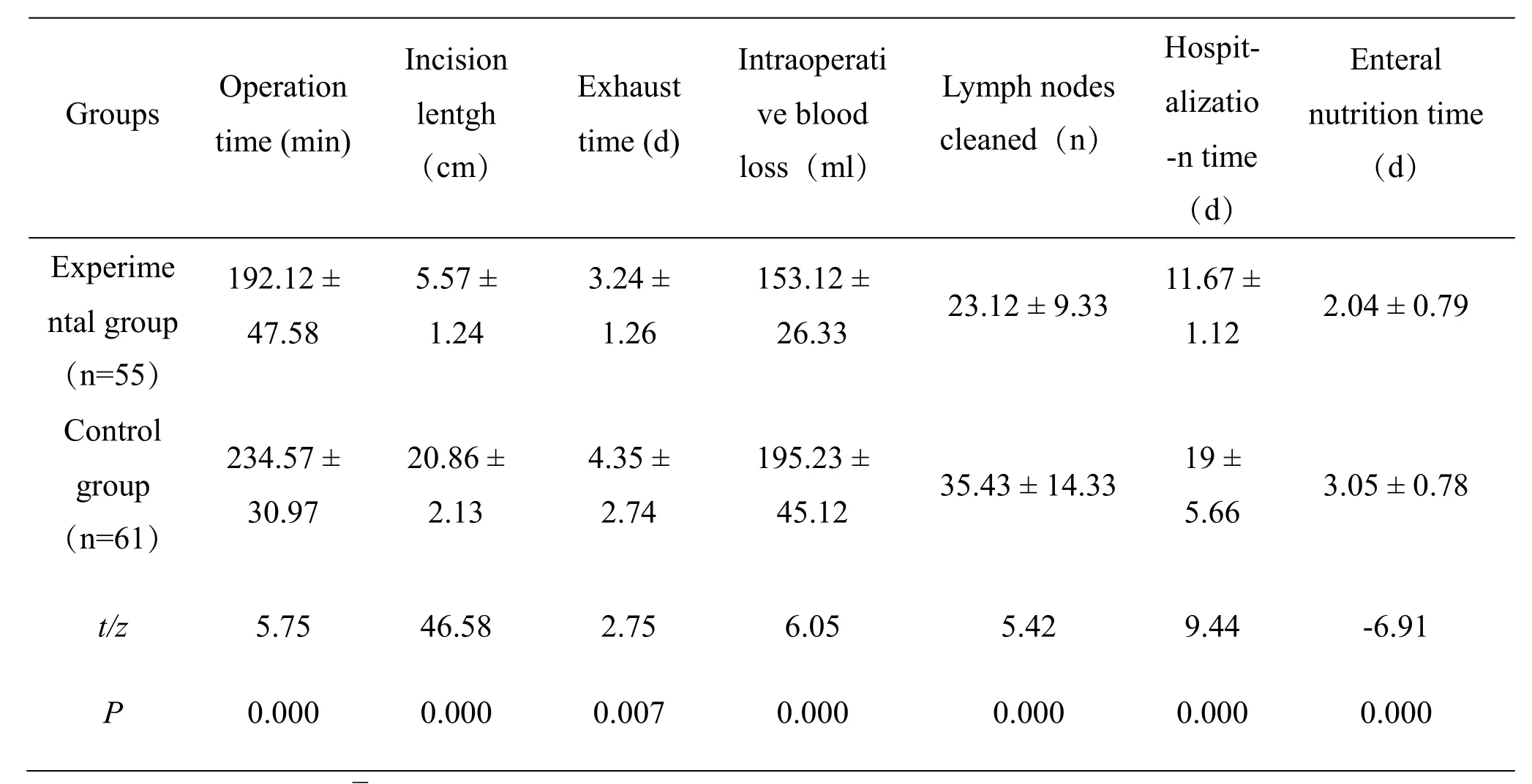
Table 2 Comparison of indexes between the two groups of patients during operation and postoperative (`x ± SD)
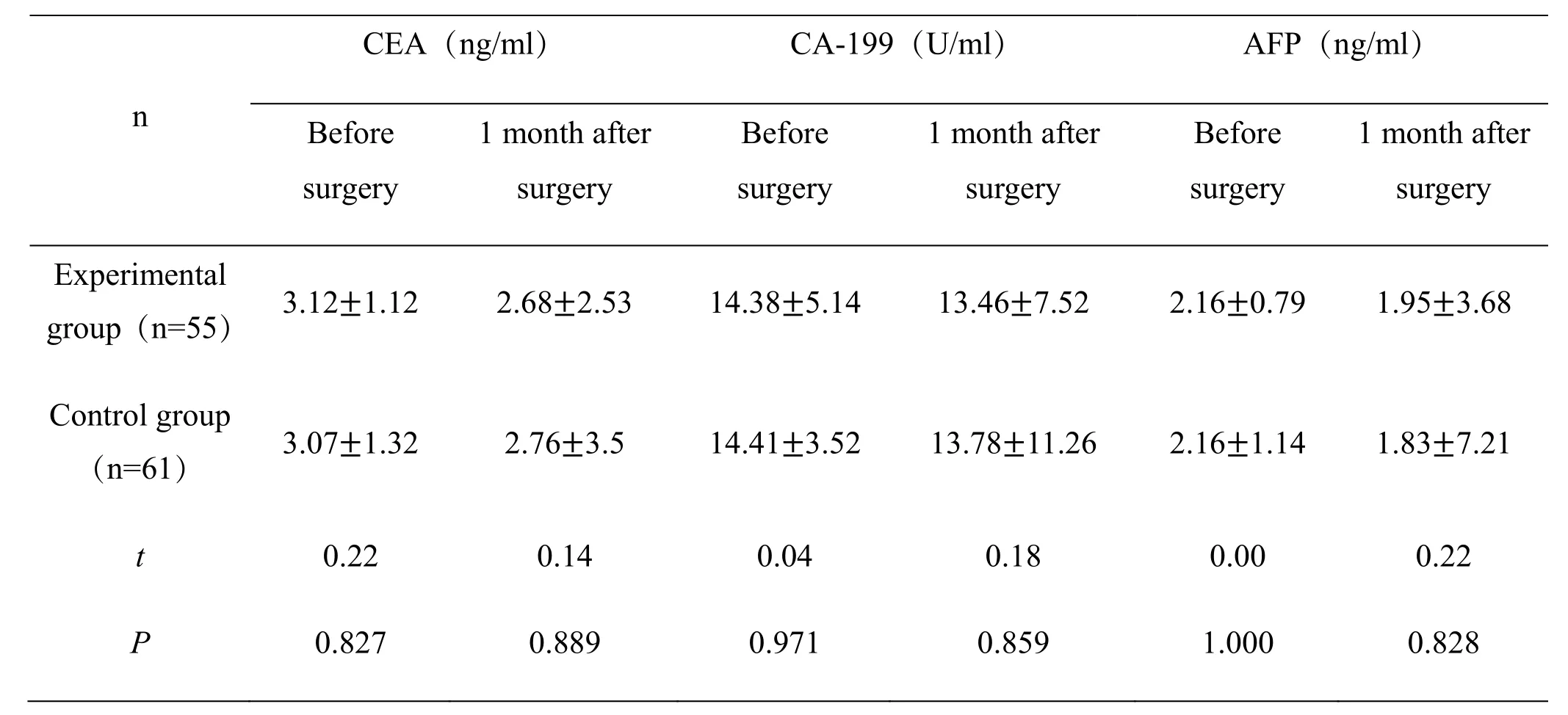
Table 3 Comparison of CEA, CA-199 and AFP between the two groups before and 1 month after surgery
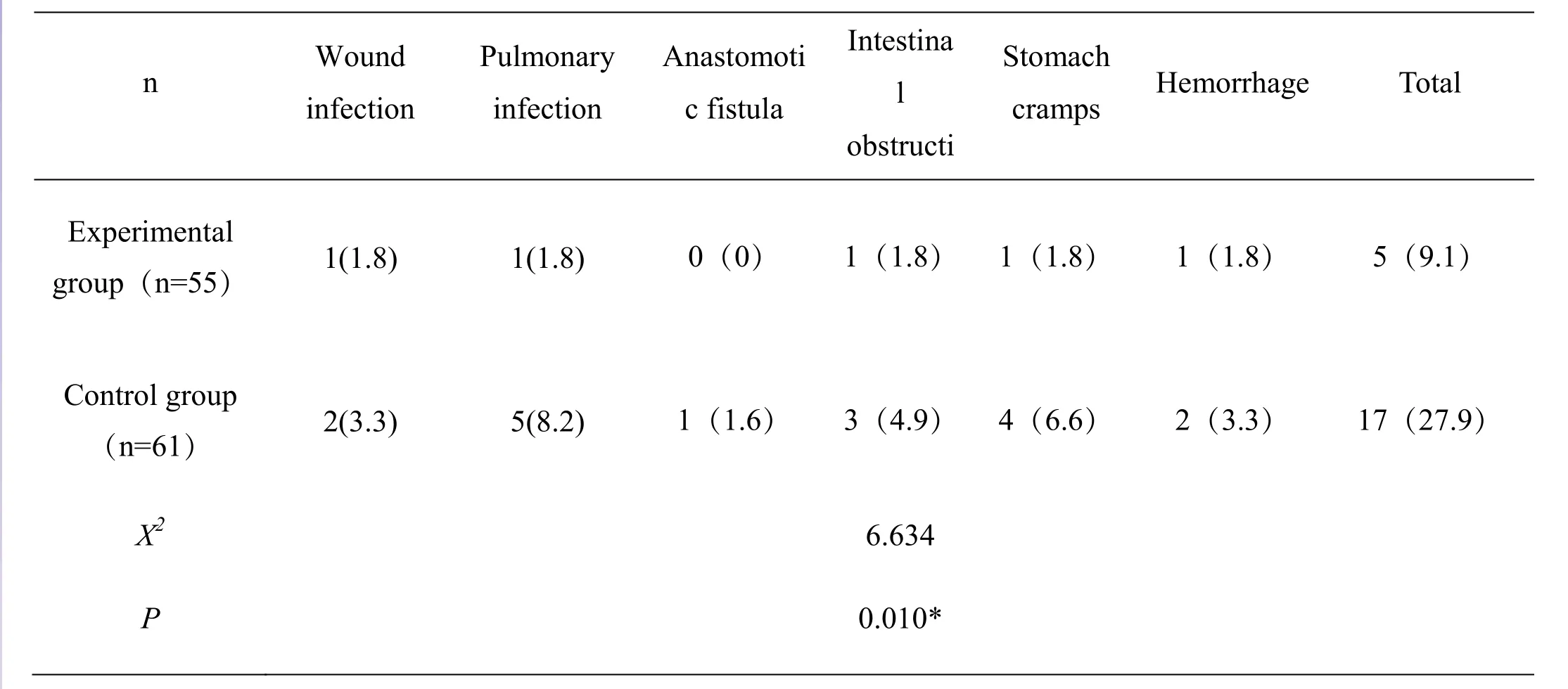
Table 4 Comparison of postoperative complication rates between the two groups (n/%)
Discussion
Traditional open surgery and laparoscopic radical gastrectomy have been carried out in our hospital for several years, and the related operation of laparoscopic radical gastrectomy has already passed the learning curve. A retrospective study of clinical outcomes was performed in the previous period, but randomized studies have not yet been summarized. This study used a randomized study to compare the clinical effects of the two treatments. The results showed that the laparoscopic group of patients during and after the operation (including the operation time, length of the incision, exhaust time, intraoperative blood loss,hospital stay, Enteral nutrition time) was superior to the control group, indicating laparoscopic radical surgery may significantly shorten the length of the surgical incision, which is conducive to postoperative recovery,reduce hospitalization time and improve the quality of life of patients. The result is the same as that of Shen Renbin et al. [3-6] and has great promotion value. This is mainly related to the advantages of laparoscopic itself.For example, Laparoscopy increases the scope of the intraoperative field of view, and an ultrasonic scalpel can also accurately separate blood vessels and tissues.When bleeding occurs, it can quickly stop bleeding and reduce the amount of bleeding. Studies have shown that laparoscopic radical gastrectomy with short incision and small wound surface may effectively shorten postoperative recovery time [7], which can alleviate the suffering of patients and increase the utilization rate of beds. The results of this study showed that the total number of lymph nodes removed by laparoscopic radical gastrectomy was less than that of the open group.However, Yan Pingxiong [8] and other researchers found that there was no difference in the total number of lymph nodes in the two surgical procedures, which may be related to sample size and requires large sample multicenter studies.
Timely detection of serum tumor markers CEA,CA-199, AFP is of great significance for the diagnosis,postoperative treatment, and prognosis of gastric cancer.Studies have shown that AFP and CEA are lower in normal humans, but these two indicators will increase in tumor patients (stomach cancer, colon cancer, et al.),which can reflect the incidence of various tumors.However, clinical findings have a single index specificity, sensitivity, and accuracy, which cannot accurately reflect the disease. Therefore, combined detection of these tumor markers can improve the accuracy of diagnosis of the disease [9-11]. CA199 is one of the tumor antigens. After the cancer cells appear,the blood vessels may enter the blood circulation through the thoracic duct. The index of the tumor patients will increase significantly, and the index is closely related to the tumor size, stage, and degree of infiltration [12]. In this study, the tumor indicators were compared before and after surgery, and the difference was not significant, indicating that the tumor index could not reflect the effect of the two operations in a short period of time, and long-term follow-up observation was needed. This study showed that the incidence of postoperative complications in the laparoscopic group was 9.1% significantly lower than 27.9% in the control group. How to reduce the postoperative complications of radical gastrectomy has always been a close concern of clinicians. Laparoscopic radical gastrectomy can effectively solve this problem.This is mainly due to the wide exposure of laparoscopic surgery, which can effectively reduce bleeding and the length of the abdominal incision.
In conclusion, laparoscopic radical gastrectomy can be worthy of promotion. However, to more effectively reduce the complications of laparoscopic gastric cancer after D2 radical resection, it is necessary to evaluate all aspects before and after surgery, and actively prepare and operate strictly.
Reference
1. Hu WG, Ma JJ, Zang L, et al. Learning curve and long-term outcomes of laparoscopy-assisted distal gastrectomy for gastric cancer. J Laparoendoscopic 2014, 24(7): 487-492.
2. Laparoscopic and endoscopic surgery group of the Chinese medical association surgery branch. Guide for laparoscopic surgery for gastric cancer (2016 edition). Chin J Digestive Surgery 2016, 15:851-857.
3. Shen RB, Xu W. Comparison of the effects of laparoscopic and open radical gastrectomy on regional lymph node dissection and complications.Chin J General Surgery (Electronic Edition) 2017,11: 472-474.
4. Ding DS. Therapeutic effect of laparoscopically assisted distal gastric cancer D2 radical resection for advanced gastric cancer. Chin J General Practice 2016, 14: 1325-1326+1350.
5. Chen SJ, Wang YQ, Liu WN, et al. Clinical effect and prognosis of laparoscopic D2 radical surgery for gastric cancer. Chin J General Surgery(Electronic Edition) 2018, 12: 133-136.
6. Yan PX, Wang ZW, Cui HN, et al. The role of 3D laparoscopy in improving the success rate and safety of gastric cancer radical surgery and its impact on the incidence of surgery-related complications. Chin J General Surgery (electronic version) 2018, 12: 126-129.
7. Li CJ, Shi SC, Luo JB. Clinical comparison of open surgery and laparoscopic assisted radical gastrectomy for distal gastrectomy. J Laparoscopic Surgery 2017, 22: 46-49.
8. Yan PX, Wang ZW, Cui HN, et al. Comparative analysis of the efficacy of laparoscopic and open radical gastrectomy. Chin J General Surgery(Electronic Edition) 2018, 12: 339-342.
9. Xu HH, Yu DX. Clinical value of combined detection of CRP, CEA, CA199 and CA724 in gastric cancer. Modern Diags Treat 2018, 29:2614-2615.
10. Bian XH. Value Analysis of combined detection of tumor markers in CA724, CEA, CA242 and CA199 in gastric cancer. Chin J Woman Child Health Research 2018, 28: 325.
11. Li XC, Feng LZ, Wu CX. Changes of serum TSGF,AFP and HER-2/neuECD in patients with gastric cancer before and after operation and its clinical significance. Chin J Clin Oncol Rehabilitation 2017,24: 1064-1066.
12. Yang W. Analysis of the diagnosis effect of combined detection of serum tumor markers CEA,CA19-9, CA242 and CA724 on gastric cancer. J Mathematical Med 2018, 31: 47-48.
- Cancer Advances的其它文章
- Effective ingredients, potential targets and mechanism in cancers treatment of Bushen Jiedu Sanjie recipe
- Analyzing the effective compounds, potential targets and diseases of Jianpi Jiedu recipe based on network pharmacology and function validation of cytobiology
- Compound Kushen injection combined with chemotherapy in the treatment of gastric cancer: a meta-analysis of randomized controlled trials
- Advances in research on tumor microenvironment of hepatocellular carcinoma